First-generation antipsychotics (FGAs) are drugs used primarily for the treatment of schizophrenia and related psychotic disorders. The use of FGAs has declined in the last few years, mainly because of an increase in prescriptions of second-generation agents. Since FGAs are considerably less expensive than newer antipsychotics, they remain a valuable option in the treatment of psychotic disorders. This article is an introduction to terminology, mechanism of action, classifications and potency of conventional antipsychotics.
History and Definitions
First-generation antipsychotics are also known as: typical antipsychotics, dopamine antagonists, neuroleptics and classic antipsychotics. Each term has important historical and conceptual implications.
Neuroleptics
The term “neuroleptic” refers to the ability of a drug to cause a syndrome known as “neurolepsis”. This syndrome has three main features [1]:
- Psychomotor slowing
- Emotional quieting
- Affective indifference
Initially, clinicians deduced that this symptomatology was a reliable sign of antipsychotic efficacy. Later it was discovered that these effects are not required for therapeutic actions.
Dopamine antagonists
The designation dopamine antagonists proposes differentiating FGAs and SGAs based on general pharmacodynamic differences. According to this terminology, SGAs are known as dopamine-serotonin antagonists, mainly because of their high affinity for 5HT2A receptors [2].
Typical Antipsychotics
This is the most commonly used term in clinical practice. It is based on the view that second-generation antipsychotics (SGAs) have atypical properties, such as a low risk of extrapyramidal symptoms (EPS). Drugs that do not have atypical properties are considered typical or conventional antipsychotics. The problem was that the original concept of atypicality (low EPS risk) changed to a broader definition that included efficacy for negative and cognitive symptoms in schizophrenia [3]. This definition was revised after the CATIE trial failed to confirm that SGAs are more effective than FGAs (with the exception of clozapine for treatment-resistant schizophrenia). In order to avoid confusion regarding effectiveness in schizophrenia, the World Psychiatric Association suggested the term first-generation antipsychotics.
Mechanism of Action
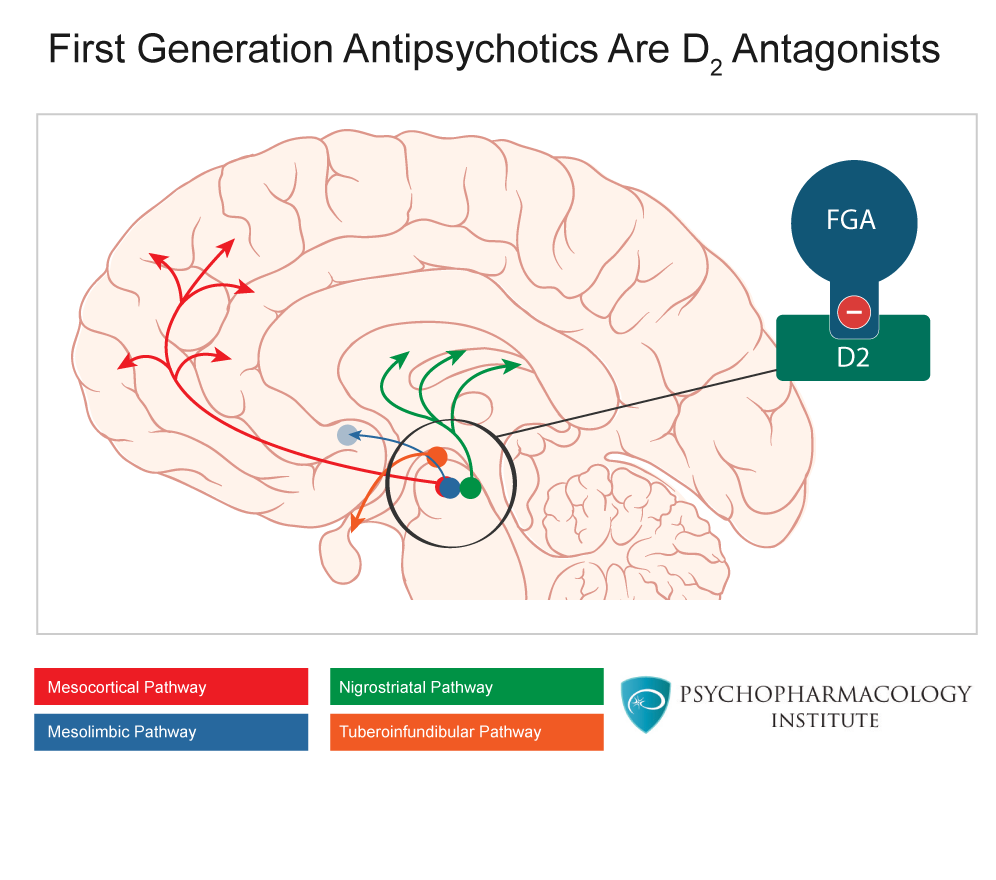
Effects of first-generation antipsychotics on the four dopamine pathways
The implications are the following:
Mesocortical pathway.
Research on schizophrenia pathophysiology suggests that a dysfunction of this pathway is associated with cognitive impairments and disturbances of emotions and affect (negative symptoms). Blockade of the mesocortical pathway by high doses of first-generation antipsychotics can induce secondary negative symptoms and cognitive effects.
Mesolimbic pathway: Antipsychotic effects
As explained earlier, overactivity of this pathway is thought to be involved in the pathophysiology of positive symptoms of schizophrenia. Blockade of D2 receptors in the mesolimbic pathway has been proposed as a possible mechanism of antipsychotic action of first-generation agents.
Nigrostriatal pathway: Extrapyramidal Symptoms
Antagonism of D2 receptors in the nigrostriatal pathway is associated with increased risk of extrapyramidal symptoms.
Tuberoinfundibular pathway: Hyperprolactinemia
Dopamine acts as a prolactin-inhibiting factor, D2 blockade increases prolactin levels by promoting its release in the pituitary gland.
Chemical Classification
Phenothiazines
The phenothiazines are the largest chemical group, comprising more than 40 compounds (only the most relevant are listed below) grouped under three subtypes.

Drugs in this group share the same three-ring structure with different side chains joined at the nitrogen atom of the middle ring. The activity of the group can be affected by substitutions at position 2 or 10. The phenothiazines are categorized into three subclasses based on substitutions at position 10: aliphatic, piperidine, and piperazine phenothiazines. Table 1 is a selection of the most commonly prescribed phenothiazines, the list also specifies potency according to side chain subtype.
Table 1- Phenothiazines chemical classification
| Chemical Class | Side Chain | Drug |
|---|---|---|
| Phenothiazines | Aliphatic (low/medium-potency agents) | Chlorpromazine |
| Levomepromazine | ||
| Promazine | ||
| Triflupromazine | ||
| Piperidine (low/medium potency agents) | Mesoridazine | |
| Pericyazine | ||
| Pipotiazine | ||
| Thioridazine | ||
| Piperazine (medium/high-potency agents) | Perphenazine | |
| Fluphenazine | ||
| Trifluoperazine |
Butyrophenones, thioxanthenes, dihydroindolones, dibenzepines and diphenylbutylpiperidines
Table 2 lists non-phenothiazine first-generation antipsychotics. This list does not include all non-phenothiazine antipsychotics available worldwide, but offers an overview of the most commonly used agents.
Table 2: Non-phenothiazine antipsychotics
| Chemical Class | Drug |
|---|---|
| Butyrophenones (high-potency agents) | Benperidol |
| Droperidol | |
| Haloperidol | |
| Thioxanthenes (low/medium-potency agents) | Clopenthixol |
| Flupenthixol | |
| Thiothixene | |
| Zuclopenthixol | |
| Dihydroindolones (low/medium-potency agents) | Molindone |
| Dibenzepines (low/medium-potency agents) | Clotiapine |
| Loxapine | |
| Diphenylbutylpiperidines (high-potency agents) | Fluspirilene |
| Pimozide |
Receptor Affinity Profile
| Dosage forms | D2 Activity | 5HT2 Activity | Muscarinic Activity | Alpha-1 adrenergic Activity | Antihistamine Activity | |
|---|---|---|---|---|---|---|
| Chlorpromazine (Thorazine) | T, I | |||||
| Fluphenazine (Prolixin) | T, L, I, I (LA) | |||||
| Perphenazine (Trilafon) | T | |||||
| Trifluoperazine (Stelazine) | T | |||||
| Thioridazine (Mellaril) | T | |||||
| Mesoridazine (Serentil) withdrawn from US market in 2004 | T | |||||
| Haloperidol (Haldol) | T, L, I, I (LA) | |||||
| Molindone (Moban) *discontinued by manufacturer in 2010 | T | |||||
| Thiothixene (Navane) | C | |||||
| Loxapine (Loxitane) | C |
Level/degree of effect: (+) – low (++) – moderate (+++) – high (++++) – very high Adapted from Hahn, Albers and Reist. Psychiatry, 2008 Edition
Adverse Effects Profile
| Drug | Sedating effects | Anticholinergic effects | Extrapyramidal side effects | Hypotensive effects |
|---|---|---|---|---|
| Chlorpromazine | High | High | Low | IM-High |
| PO-Moderate | ||||
| Fluphenazine | Low | Low | Very high | Low |
| Haloperidol | Very low | Very low | Very high | Very low |
| Loxapine | Moderate | Low | Moderate | Moderate |
| Molindone | Very low | Low | Moderate | Low |
| Perphenazine | Low | Low | High | Low |
| Pimozide | Low | Low | High | Very low |
| Thioridazine | High | High | Low | High |
| Thiothixene | Low | Low | High | Low |
| Trifluoperazine | Low | Low | High | Low |
Antipsychotic Potency: Chlorpromazine Equivalent Doses
First-generation antipsychotics can be classified according to their potency. All FGAs are compared to chlorpromazine for equivalence purposes. Potency should not be confused with effectiveness. For example, if we know that haloperidol is more potent that chlorpromazine, it means that a lower dose of haloperidol is required to achieve the same therapeutic effect, but not that haloperidol is more effective than chlorpromazine. The table below shows doses equivalent to 100 mg of chlorpromazine, this table is a combination of two sources: The Maudsley Prescribing Guidelines [5], and the Manual of Clinical Psychopharmacology [6].
| Drug | Maudsley Prescribing Guidelines | Manual of Clinical Psychopharmacology |
|---|---|---|
| Chlorpromazine | 100 mg/day | 100 mg/day |
| Fluphenazine | 2 mg/day | 2 mg/day |
| Trifluoperazine | 5 mg/day | 5 mg/day |
| Flupentixol | 3 mg/day | |
| Zuclopentixol | 25 mg/day | |
| Haloperidol | 3 mg/day | 2 mg/day |
| Sulpiride | 200 mg/day | |
| Pimozide | 2 mg/day | |
| Loxapine | 10 mg/day | 10 mg/day |
| Molindone | 10 mg/day | |
| Perphenazine | 10 mg/day | |
| Prochlorperazine | 15 mg/day | |
| Thioridazine | 100 mg/day | |
| Thiothixene | 4 mg/day |
Key points
- First-generation antipsychotics are also known as typical antipsychotics, conventional or classic antipsychotics and dopamine antagonists.
- FGAs reduce dopaminergic neurotransmission in the four dopamine pathways by blocking D2 receptors.
- FGAs differ in potency, not effectiveness.
- High-potency: haloperidol, fluphenazine
- Mid-potency: perphenazine, loxapine
- Low-potency: chlorpromazine
References
- Stahl, S M. Stahl’s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications. 3rd ed. New York: Cambrigde University Press; 2008
- Sadock, B J., V A. Sadock, and P Ruiz. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 9th ed. Philadelphia: Lippincott Williams & Wilkins, 2009.
- Grunder, G., H. Hippius, and A. Carlsson. “The ‘Atypicality’ of Antipsychotics: A Concept Re-Examined and Re-Defined.” Nat Rev Drug Discov 8.3 (2009): 197-202
- Schatzberg, AF, Nemeroff, C . The American Psychiatric Publishing Textbook of Psychopharmacology. 4th ed. American Psychiatric Publishing, 2010.
- Taylor, D; Paton,C ; Kapur, S (Editors)The Maudsley Prescribing Guidelines in Psychiatry, Wiley-Blackwell; 11th Edition,2011
- Schatzberg, AF., Cole, JO, and DeBattista, C. Manual of Clinical Psychopharmacology. 7th ed. American Psychiatric Publishing, 2010.



