Discontinuation symptoms can occur with all antidepressant classes, and you will see many articles referring to SSRI discontinuation syndrome. The reason is that SSRIs are by far the most commonly prescribed antidepressant class. This syndrome consists of usually mild and reversible symptoms that can be grouped into six categories. As a general guideline, management involves restarting antidepressant medication.
Let’s see an overview of this topic.
Discontinuation symptoms can occur with all antidepressant classes, and you will see many articles referring to SSRI discontinuation syndrome. This has to do with the fact that SSRIs are by far the most commonly prescribed antidepressant class.
This syndrome consists of usually mild and reversible symptoms that can be grouped into six categories. As a general guideline, management involves restarting antidepressant medication.
Clinical Relevance

The first question we are addressing here is: Are antidepressants addictive?
The term withdrawal is often avoided, as it may imply that antidepressants are addictive or cause a dependence syndrome. As pointed out by Haddad and Anderson, the occurrence of withdrawal symptoms doesn’t in itself indicate that a drug causes dependence. There is no evidence that patients crave antidepressants once they have stopped them.
So, one of the messages we can send our patients is that antidepressants are not addictive. This is important as fear of addiction can reduce treatment adherence.
Why should we care about antidepressant discontinuation syndrome?
In this slide, I list three reasons: the first is morbidity. Even though discontinuation symptoms are rarely fatal, they are associated with discomfort and some degree of psychosocial impairment.
The second is a misdiagnosis. Discontinuation symptoms can be confused with a recurrence of psychiatric illness or other medical problems. We’ll discuss this in the next slide.
The third is treatment adherence. After experiencing discontinuation symptoms, patients may be unwilling to use psychotropic medications in the future.
Let’s focus now on the problem of misdiagnosis.
Discontinuation symptoms can be confused with adverse effects of a new medication. This may lead us to the incorrect conclusion that the patient can’t tolerate the new medication. This can happen when switching antidepressants with different mechanism of action, for example, from paroxetine to bupropion .
Discontinuation symptoms can also be confused with recurrence of the underlying psychiatric illness. An example of this would be the following situation: a patient has achieved remission of depressive symptoms and the physician recommends stopping the antidepressant but doesn’t advise how to do it. So, the patient stops medications abruptly, leading to discontinuation symptoms. If the prescriber is not aware of this abrupt interruption, then he or she might confuse this with depression recurrence.
Discontinuation symptoms might also be confused with a failure to respond to treatment, especially mental symptoms such as irritability or anxiety. Discontinuation symptoms can also be misdiagnosed as medical problems, this may lead to unnecessary referrals and evaluations by other specialists.
The discontinuation syndrome can be divided into six clusters of symptoms. Sensory symptoms, disequilibrium, general somatic symptoms, affective symptoms, gastrointestinal symptoms, and sleep disturbance.
This syndrome was initially based on case reports, but the evidence expanded to include prospective studies, with randomized double-blind interruption periods.
Sensory symptoms include: paresthesia, numbness, electric shock-like sensations, rushing noise “ in head” and palinopsia, or visual trails.
Disequilibrium symptoms include light-headedness, dizziness and vertigo.
General somatic symptoms have been compared to a flu-like syndrome. This includes lethargy, headache, tremor, sweating and anorexia.
Affective symptoms that can be part of the discontinuation syndrome are irritability, anxiety, low mood and tearfulness.
Gastrointestinal symptoms include nausea, vomiting and diarrhea.
The last cluster of symptoms is related to sleep disturbances, including: insomnia, nightmares and excessive dreaming.
There’s also a mnemonic to help us remember the discontinuation symptoms.
It’s the word FINISH, F for flu-like symptoms, I for Insomnia, N for nausea, I for imbalance, S for sensory disturbances, and H for hyperarousal.
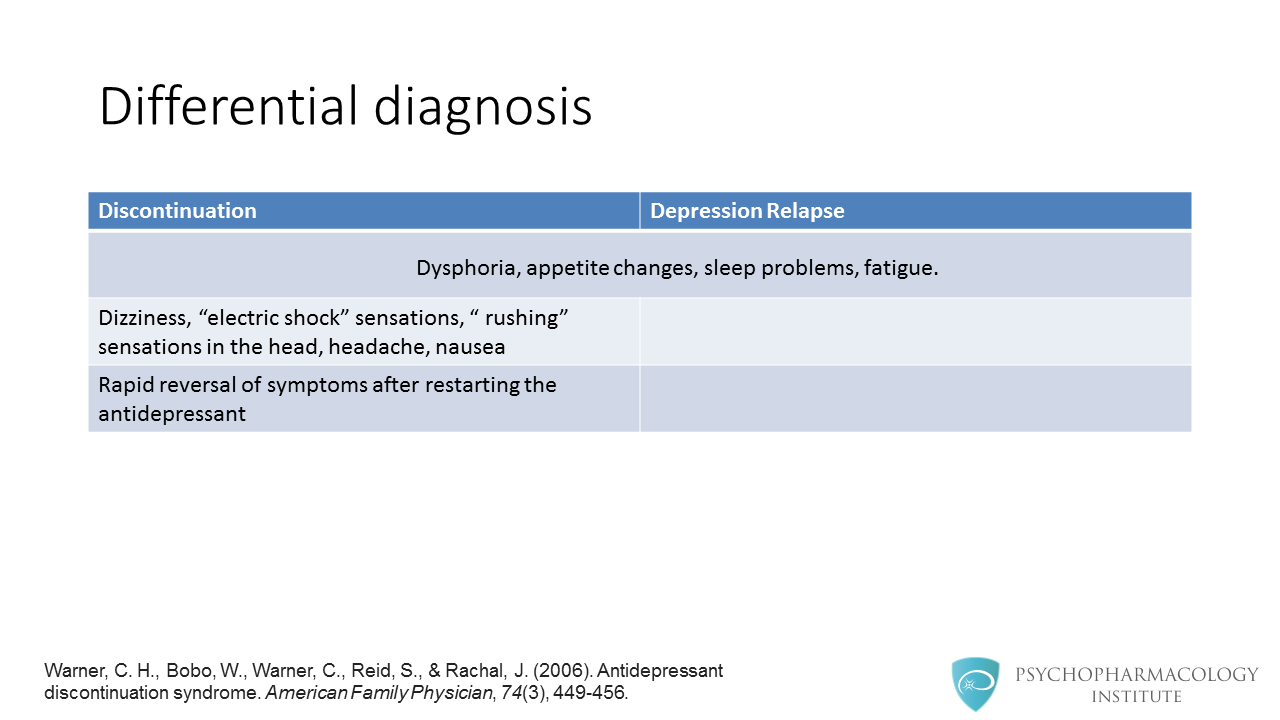
How do we differentiate discontinuation symptoms from a depressive relapse? They have in common symptoms such as dysphoria, appetite changes, sleep problems and fatigue. It’s practical to look for symptoms that are not seen in depression relapse, some examples are dizziness, “electric shock” sensations, rushing sensations in the head, headache and nausea. Also, we can see a rapid reversal of symptoms after restarting the antidepressant.
Prevention and Management
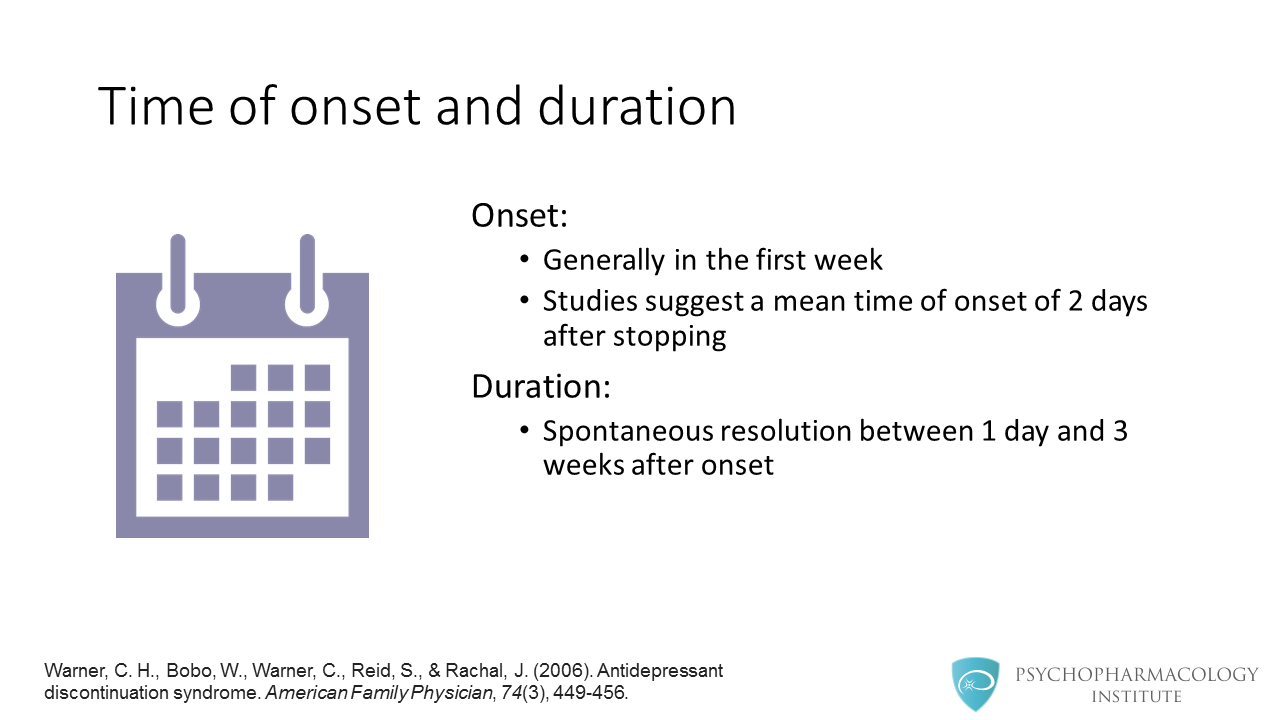
So, what do we do with a patient suffering from discontinuation symptoms? First of all, we provide reassurance. We do this by explaining that this syndrome is reversible, not life-threatening, and that it will run its course within 1 to 2 weeks.
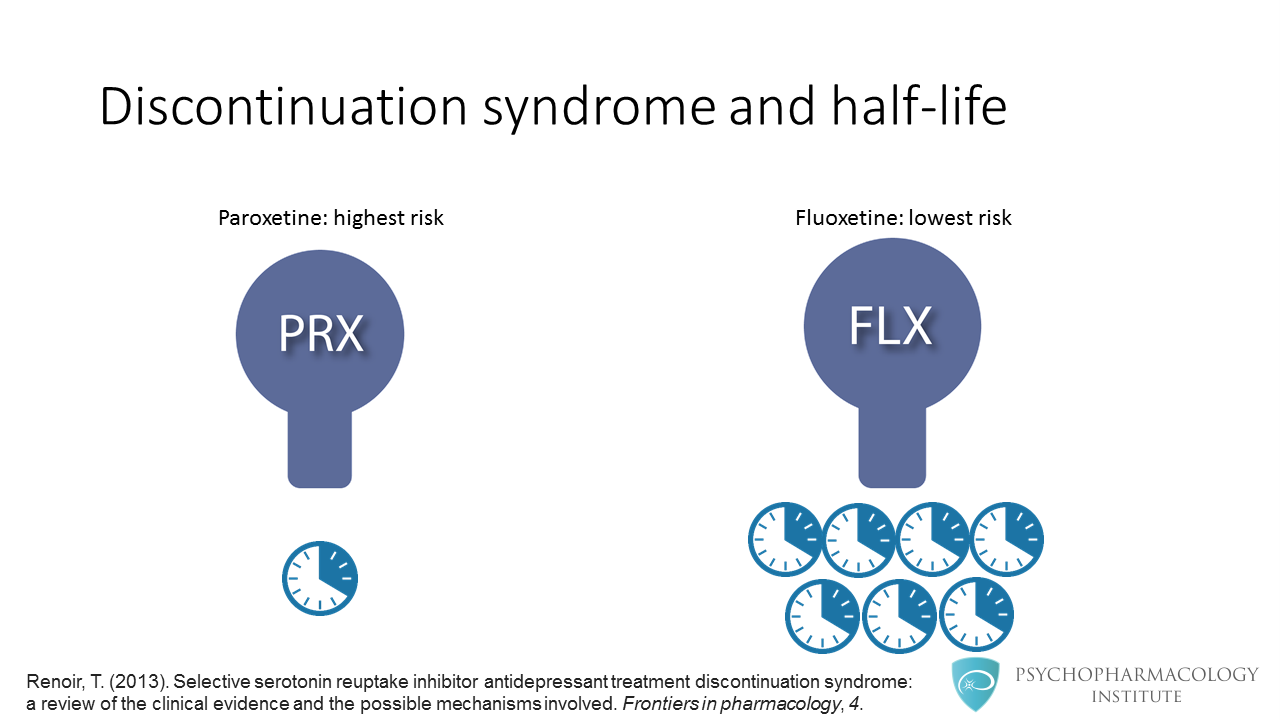
Second, we restart the medication with a slow dose taper. What if symptoms occur during tapering? In this case, we should consider restarting at the original dose and then taper at a slower rate. If slow tapering is poorly tolerated, we can consider substituting with fluoxetine.
Key Points
The key points are the following:
- Discontinuation symptoms include flu-like symptoms, insomnia, nausea, imbalance, sensory disturbances and hyperarousal. We can use the mnemonic FINISH to keep these symptoms in mind.
- This syndrome is more commonly seen with paroxetine.
- From a therapeutic standpoint, restarting the antidepressant is generally enough as management strategy.
References
- Haddad, P. M., & Anderson, I. M. (2007). Recognising and managing antidepressant discontinuation symptoms . Advances in Psychiatric treatment,13(6), 447-457.
- Warner, C. H., Bobo, W., Warner, C., Reid, S., & Rachal, J. (2006). Antidepressant discontinuation syndrome . American Family Physician, 74(3), 449-456.
- Renoir, T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved . Frontiers in pharmacology, 4.



