Slides and Transcript
Slide 1 of 20
So let's move on to the next section, Psychiatric Comorbidities with Alcohol Use Disorder: Prevalence and Management.
Slide 2 of 20
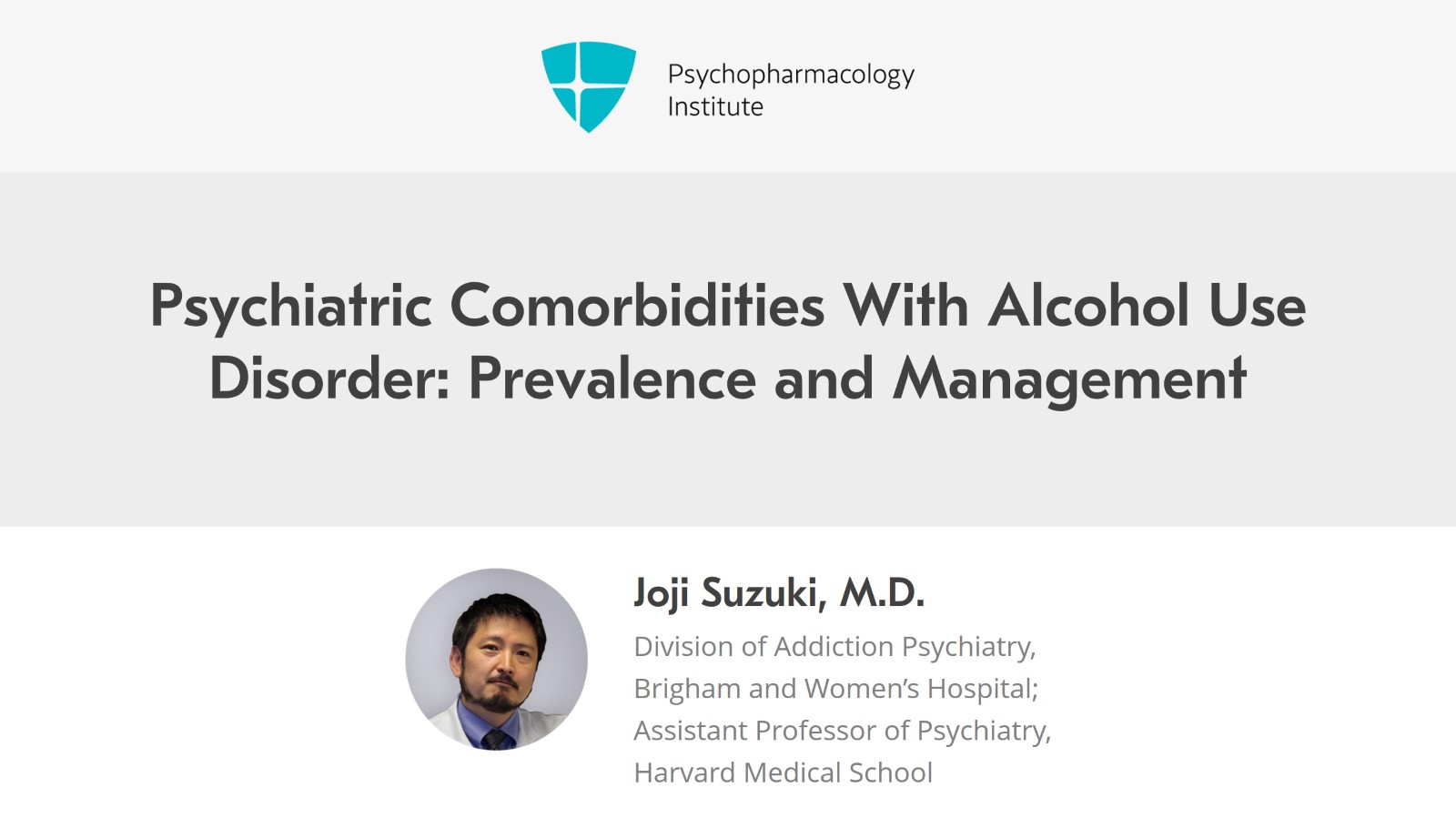
So both mood and anxiety disorders frequently co-occur with substance use disorders. And data from the NESARC study that I mentioned at the beginning of this talk, as many as 40% of individuals with alcohol use disorder had a current mood disorder and then 30% with a current anxiety disorder.
References:
- Grant, B. F., Stinson, F. S., Dawson, D. A., Chou, S. P., Dufour, M. C., Compton, W., Pickering, R. P., & Kaplan, K. (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry, 61(8), 807.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 20
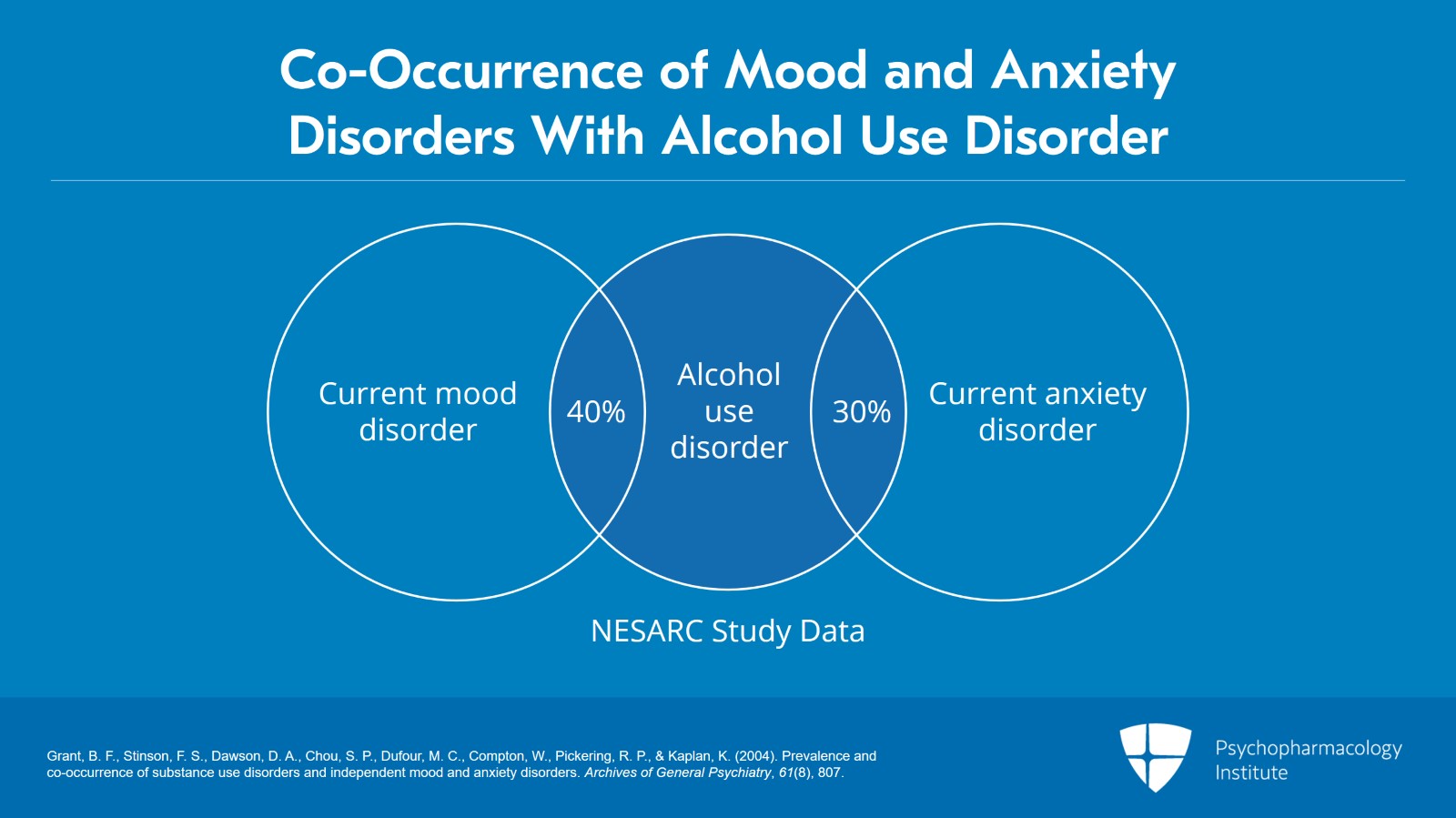
I'll just point out that the relationship between negative affect or the psychiatric diagnoses like mood and anxiety disorders and alcohol is a complicated bidirectional relationship. So on the one hand, alcohol use disorder or alcohol use can worsen depression. Alcohol on itself independently can worsen mood and sort of contribute to the development of a depressive disorder or anxiety disorders later. Alcohol is a depressant so it can worsen depression on its own. It can actually prolong the course of depression. But the converse could be true. Somebody who's depressed might use alcohol first to self-medicate, to feel better. Depression can actually make it more difficult to sort of maintain abstinence. And so depression on its own might contribute to somebody picking up a drink in the first place or making the alcohol worse.
References:
- Grant, B. F., Stinson, F. S., Dawson, D. A., Chou, S. P., Dufour, M. C., Compton, W., Pickering, R. P., & Kaplan, K. (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry, 61(8), 807.
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Slide 4 of 20
On the other hand, both of these things could be stemming from some shared vulnerability, early life childhood adversities, for example, or genetic predispositions, or it could be that these are common diagnoses and they just happen to occur by chance. It's really important in my mind to avoid any simplistic explanations of this dual diagnosis to simply categorize this comorbidity as self-medication or that mood symptoms are always a result of substance use. I believe it's a complicated sort of bi-directional and multi-directional relationship. Regardless of what the relationship is, the presence of this comorbidity often makes treatment challenging because even if both are treated, having both disorders actually, likely means that the treatment outcomes wouldn't be as good with individual, the independent diagnosis alone.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 20
Another complicating factor of this comorbidity is that symptoms of major depression and anxiety can mimic those of alcohol use disorder and vice versa. Therefore, it becomes important to discern if there is an independent mood or anxiety disorder as opposed to disorders that are substance induced.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Slide 6 of 20
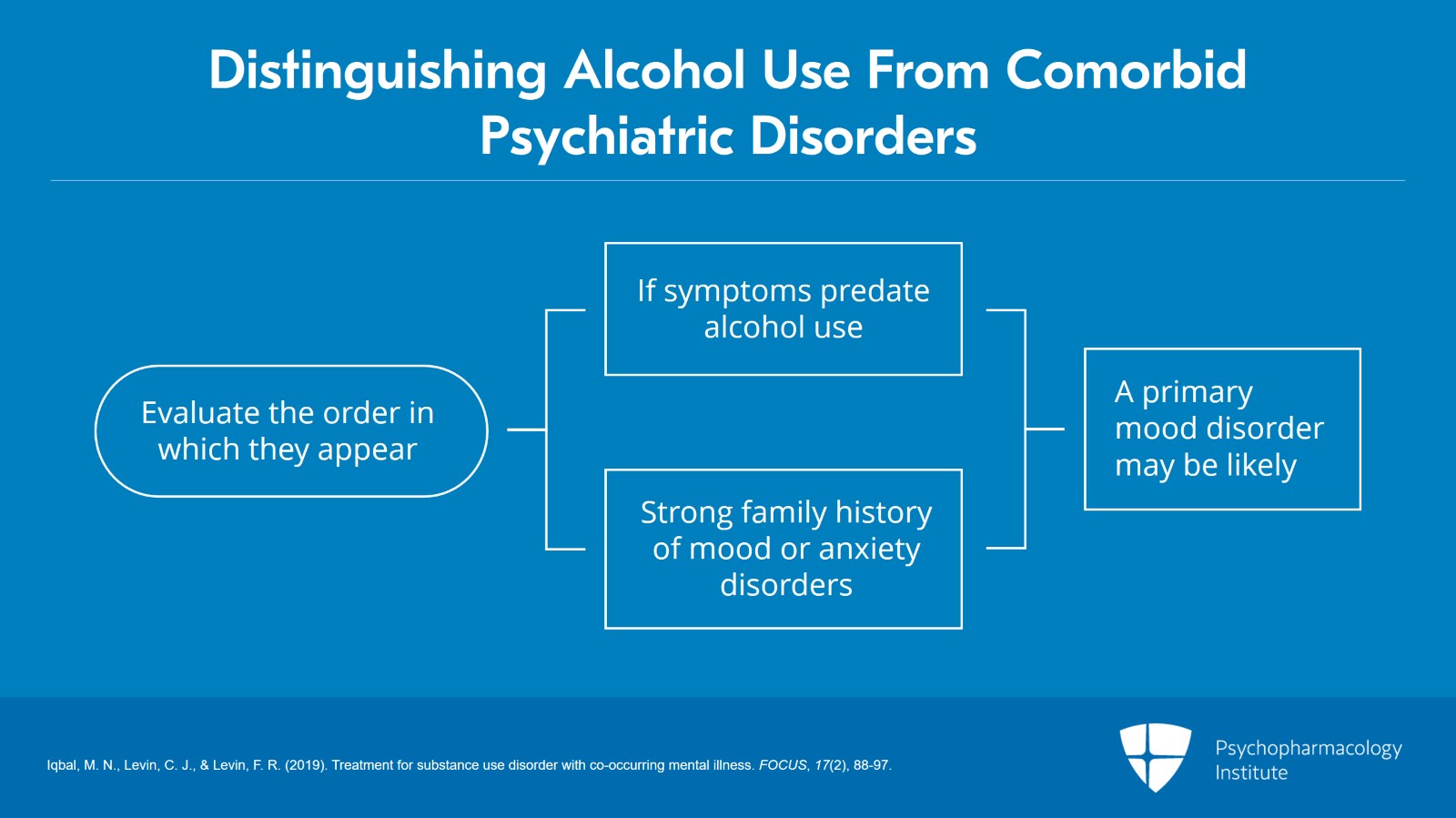
So there are several ways to distinguish these. One is the order in which they appear. If the most symptoms predate alcohol use, then a primary mood disorder in addition to an alcohol use disorder may be likely. A strong family history of the disorders whether it's mood disorder or anxiety disorder actually might, give you a stronger justification to diagnose a primary mood or anxiety disorder.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 20
Of note, anxiety disorders more often than not predate the development of substance use disorder and therefore actually might play a greater etiologic role for many patients. This actually becomes even more strong of a predictor. So early life trauma and traumatic experiences actually may play a substantial etiologic role in the development of substance use disorder later in life.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Slide 8 of 20
The next thing to assess in the history is the presence of mood or anxiety symptoms during sustained periods of abstinence. If they are largely absent, during periods of abstinence, the person reports really minimal mood or anxiety symptoms or that those symptoms remitted pretty rapidly over the course of several weeks, then actually perhaps a diagnosis of a substance-induced disorder may be more likely.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 20
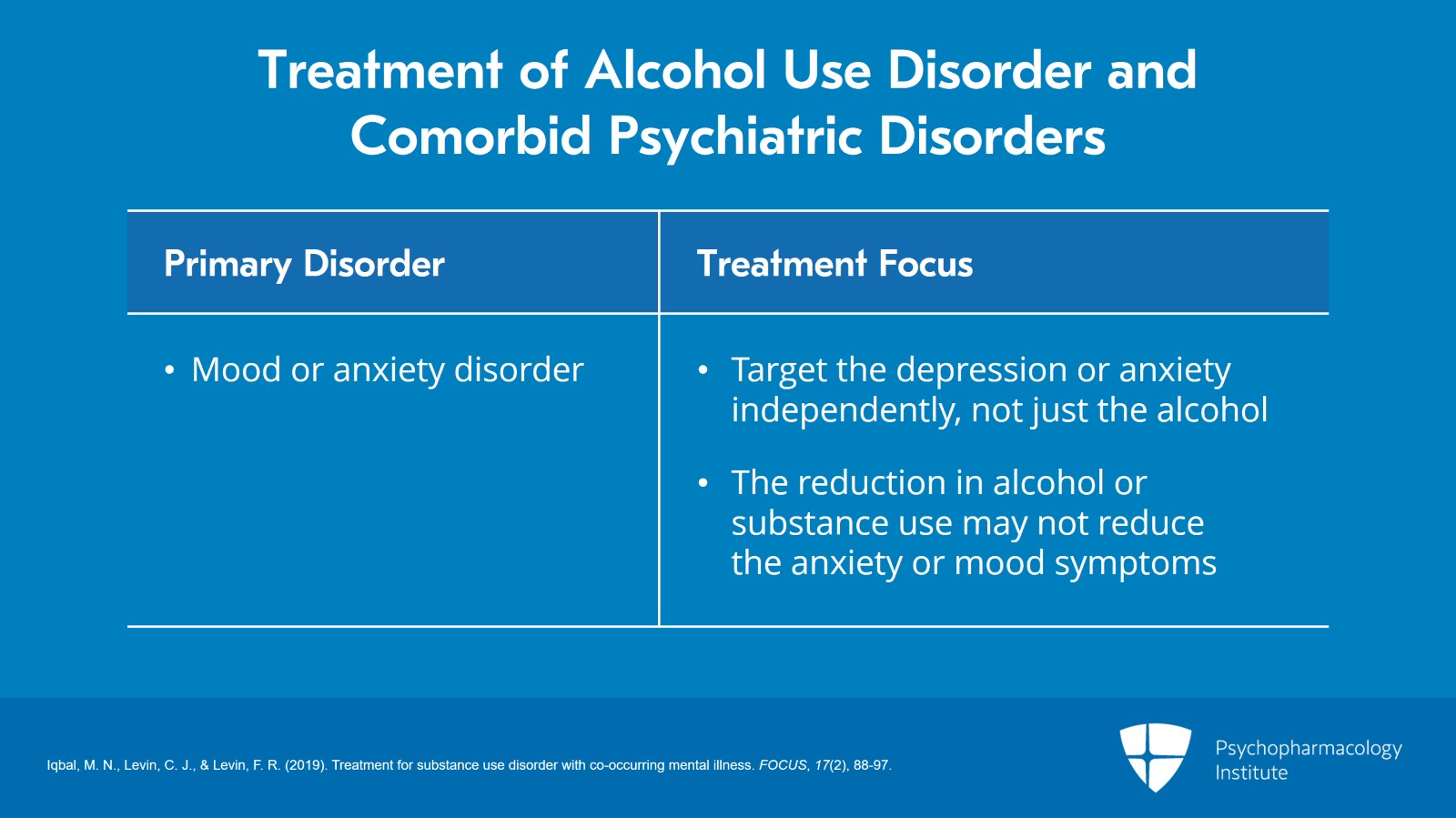
Now, distinguishing these can be important because the presence of a primary mood or anxiety disorder generally means that you really want to target that disorder independently you might have to actually target the depression or anxiety and not just target the alcohol, the reduction in alcohol use or substance use generally may not actually reduce the anxiety or mood symptoms.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Slide 10 of 20
Now, on the contrary, if the evidence points strongly to a substance-induced disorder, then it's reasonable to actually really focus on cessation of alcohol use or dramatic reduction and to see where the mood symptoms go. Then they actually may not need any targeted interventions for the mood or anxiety disorders. A reasonable sort of course to take, is to first target the alcohol use really aggressively and then only treat the mood disorder if it actually turns out that it may be an independent disorder.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 20
In reality, many individuals who are diagnosed with a substance-induced mood disorder or anxiety disorder turn out eventually to be diagnosed with a primary mood disorder anyway. And therefore, the clinician should err on the side of treating the mood disorder as if they were independent unless you have strong evidence to support that it's likely to be a substance-induced mood disorder.
References:
- Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88-97.
Slide 12 of 20
Now, antidepressants which are commonly used for both mood and anxiety disorders exert only a mild level of benefit for those who have a concurrent substance use disorder and mood disorder. It has a mild effect on substance use and a little bit better on depression. So because of this, the current recommendation again is to really offer evidence-based psychosocial treatments for those with mild to moderate level of depression and a comorbid substance use and to see where the depression goes. You do the best you can to reduce that, cut back, you know, attain abstinence if you can and then see where the mood symptoms go. But offer evidence-based psychosocial treatments to support it, CBT, for example. But if the depression is severe or the depression doesn't get better during that time, then a much more early introduction of medication treatment to address the depression may be warranted like antidepressants.
References:
- Nunes, E. V., & Levin, F. R. (2004). Treatment of depression in patients with alcohol or other drug dependence. JAMA, 291(15), 1887.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 20
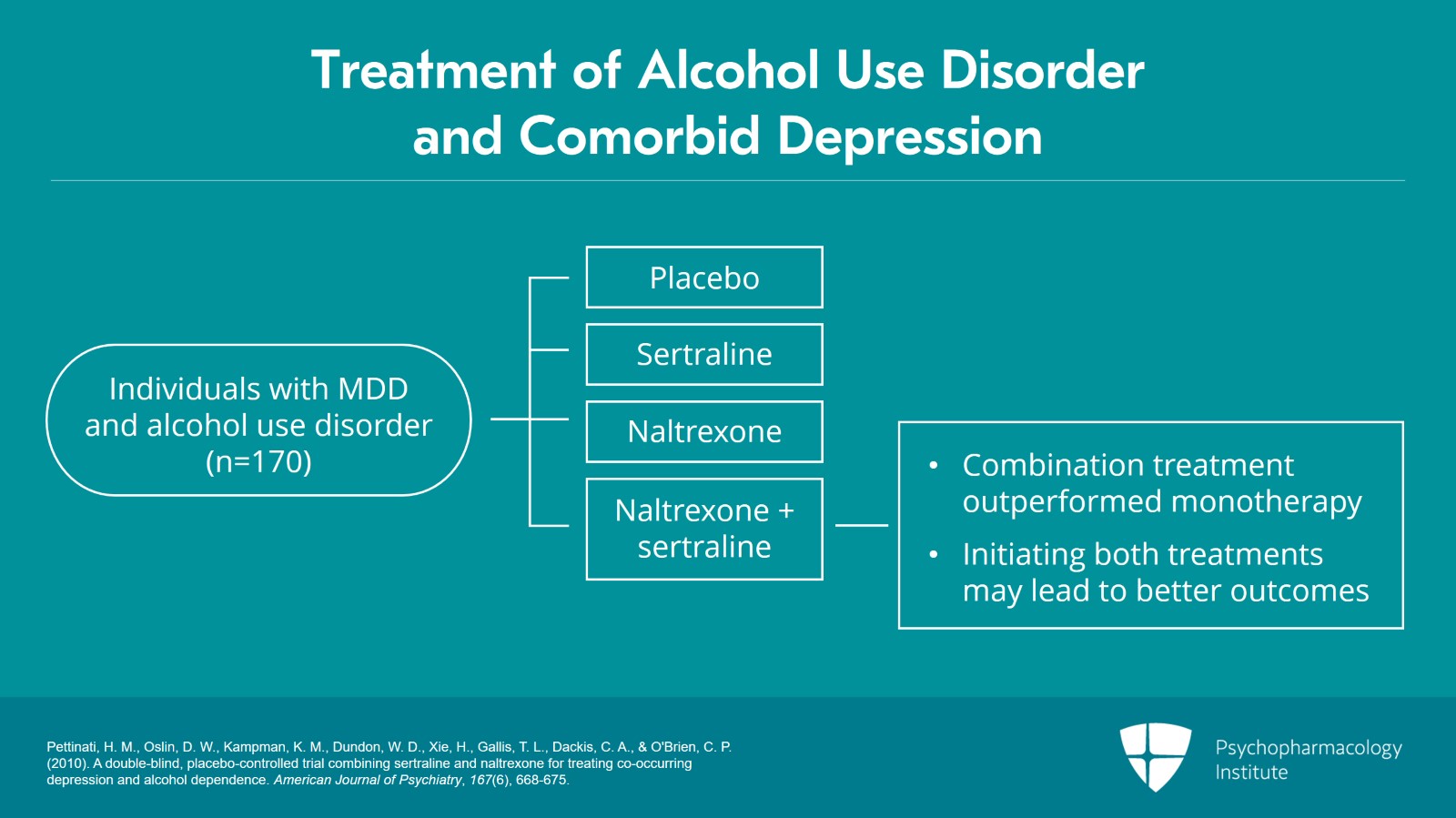
Now, this raises the question of whether antidepressants and medications for alcohol use disorder really should be combined for those with comorbid depression and alcohol. So there's actually one trial that enrolled individuals with both major depressive disorder and alcohol use disorder. And those patients were randomized to receive placebo, sertraline, naltrexone or naltrexone and sertraline. And the results really showed that, when 170 individuals were randomized to these four groups, results really indicated that the combination treatment outperformed monotherapy of either, really suggesting that if you really have an independent mood disorder and alcohol use disorder then initiation of concurrent treatment may actually be not a bad idea. If you're pretty confident this is an independent mood disorder and the symptoms are severe enough, initiating both treatments to target both actually may lead to better outcomes than a sequential treatment approach.
References:
- Pettinati, H. M., Oslin, D. W., Kampman, K. M., Dundon, W. D., Xie, H., Gallis, T. L., Dackis, C. A., & O'Brien, C. P. (2010). A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. American Journal of Psychiatry, 167(6), 668-675.
Slide 14 of 20
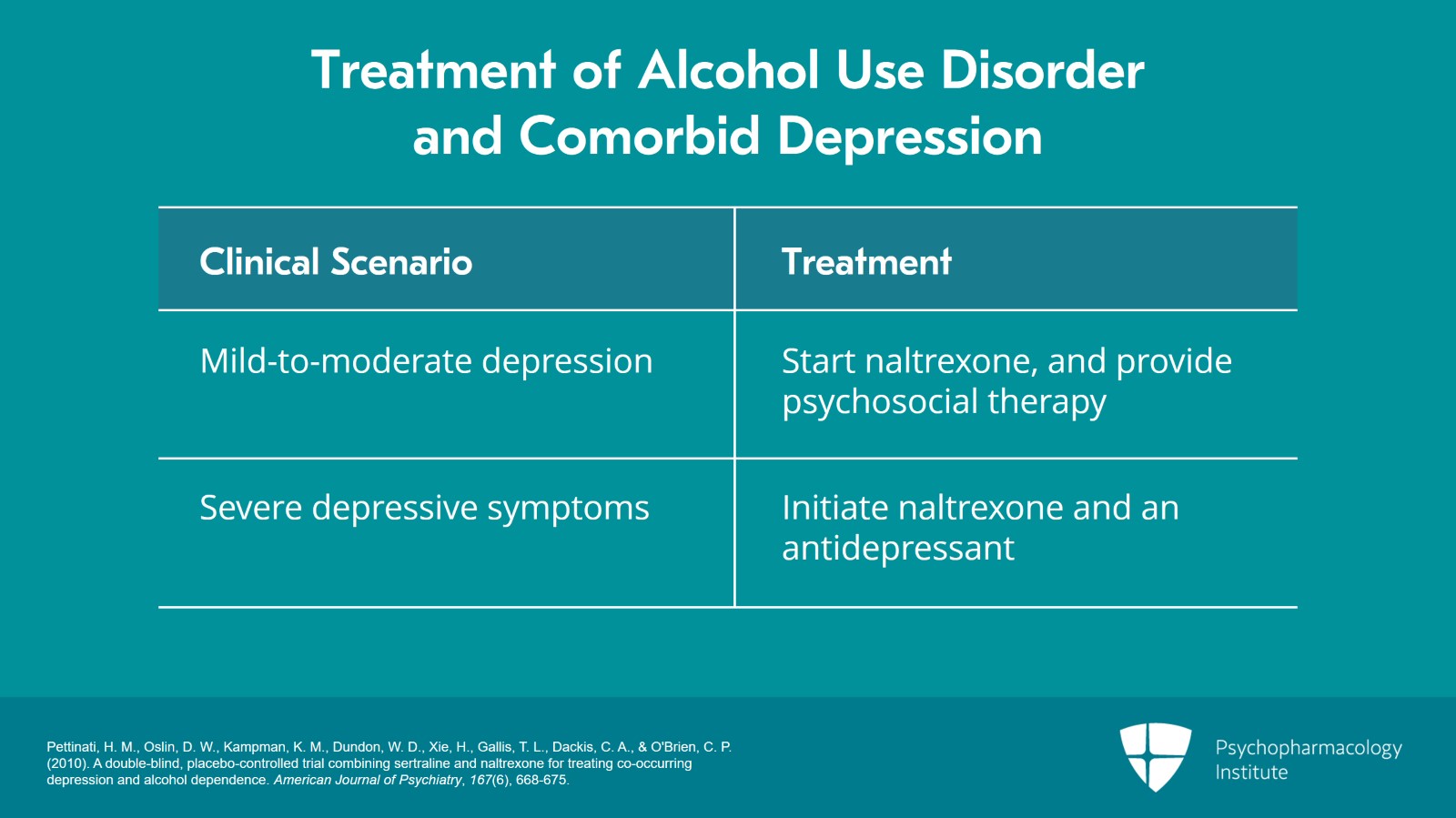
Now, really the evidence base is only on sertraline and the other SSRIs and medications that have been tried are fluoxetine and tricyclics but really the sertraline has the most evidence base and therefore is the one that's recommended. And whether to really start this, both at the same time or not really sometimes comes down to patient preference as well. It may hinge on the severity of the mood symptoms at the time that you're evaluating the patient.
References:
- Pettinati, H. M., Oslin, D. W., Kampman, K. M., Dundon, W. D., Xie, H., Gallis, T. L., Dackis, C. A., & O'Brien, C. P. (2010). A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. American Journal of Psychiatry, 167(6), 668-675.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 20
If it's still mild to moderate, then it's not unreasonable to start naltrexone and provide psychosocial therapy and then only add antidepressants if the mood symptoms don't remit or if they continue to be severe or patient preference or they start out severe then I think in that situation I would strongly recommend the simultaneous initiation of both. Of course, in pharmacotherapy, we try to avoid starting two medications at the same time because of confusion around tolerability which is causing side effects. But if the symptoms are severe enough and especially if they have a prior history of tolerating it, for example, then I would probably encourage initiation of both.
References:
- Pettinati, H. M., Oslin, D. W., Kampman, K. M., Dundon, W. D., Xie, H., Gallis, T. L., Dackis, C. A., & O'Brien, C. P. (2010). A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. American Journal of Psychiatry, 167(6), 668-675.
Slide 16 of 20
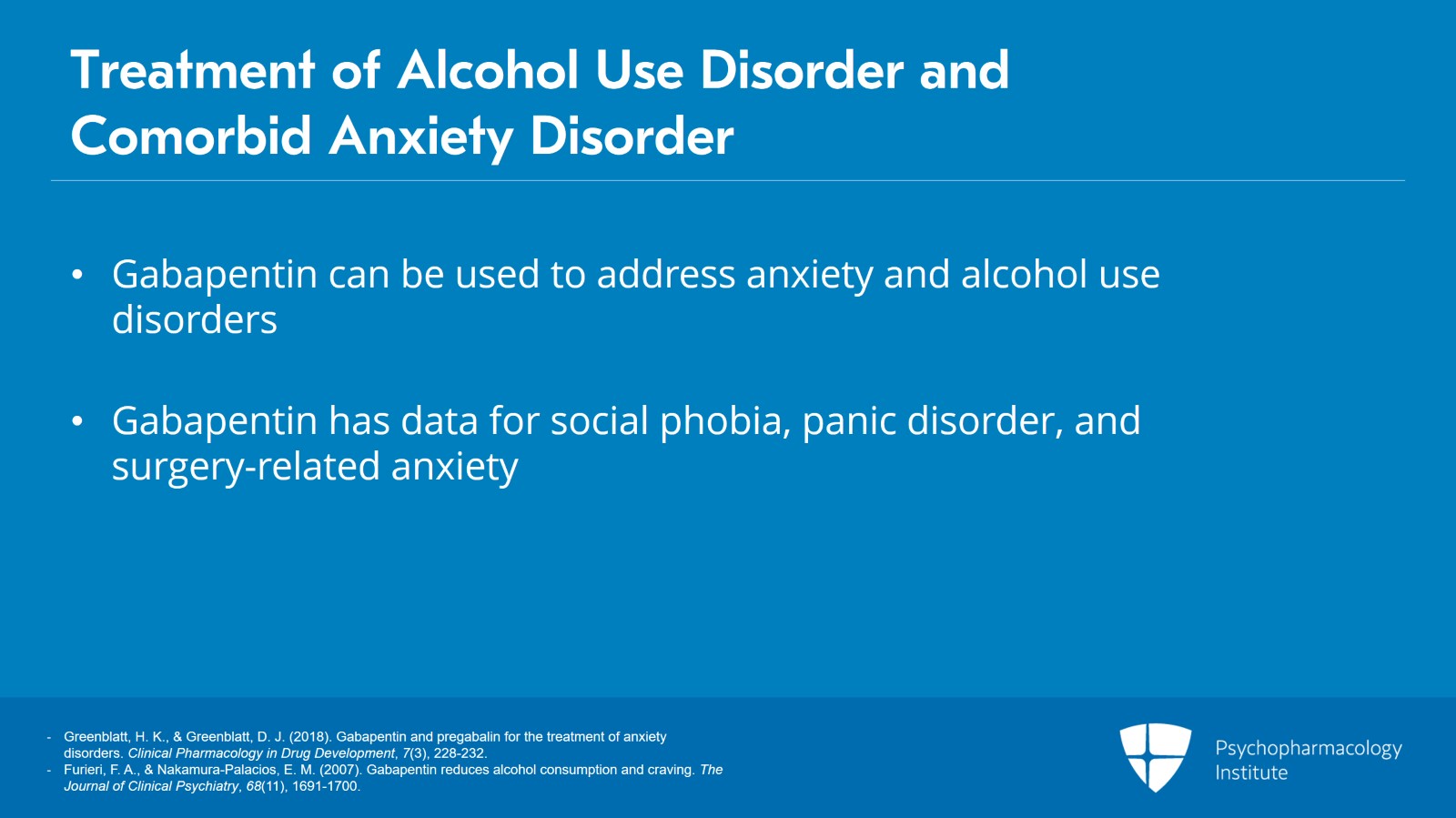
Now, in terms of comorbid anxiety disorders, I mentioned earlier gabapentin can be used. And so here's an example where gabapentin may be a good medication to do dual duty to address both the anxiety disorder and the alcohol. And there's actually quite a bit of data for social phobia, panic disorder and sort of anxiety related to surgery for gabapentin. And so it may be a reasonable thing to combine when we're treating alcohol and anxiety.
References:
- Greenblatt, H. K., & Greenblatt, D. J. (2018). Gabapentin and pregabalin for the treatment of anxiety disorders. Clinical Pharmacology in Drug Development, 7(3), 228-232.
- Furieri, F. A., & Nakamura-Palacios, E. M. (2007). Gabapentin reduces alcohol consumption and craving. The Journal of Clinical Psychiatry, 68(11), 1691-1700.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 20
Now, benzodiazepines, I've talked about using them for withdrawal management but using benzodiazepines to treat things like insomnia or anxiety in individuals with alcohol use disorder would be relatively contraindicated. This will not be recommended. There's a greater likelihood for misuse of benzos. And therefore, unless there's a very targeted reason for using them in the very short term, benzodiazepines would not be your first-line treatment for concurrent anxiety or insomnia in patients with alcohol use disorder. You would want to use things like trazadone, other anticonvulsants, ramelteon, for example, even quetiapine if needed. And lifestyle modifications would be recommended.
References:
- Mueller, T. I., Pagano, M. E., Rodriguez, B. F., Bruce, S. E., Stout, R. L., & Keller, M. B. (2005). Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcoholism: Clinical & Experimental Research, 29(8), 1411-1418.
Slide 18 of 20
So key points here. Depression and anxiety disorders frequently co-occur with alcohol use disorder and clinicians should assess whether the mood or anxiety symptoms represent an independent disorder or a substance-induced disorder.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 20
Now, treatment of depression should be initiated alongside treatment for alcohol use disorder but it's reasonable to start with psychosocial treatment first unless the depression is severe or there's patient preference or the mood symptoms don't remit in which case medication treatment like antidepressants is warranted.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.