Slides and Transcript
Slide 1 of 9
Video number 11. Venlafaxine and prazosin. This was the most frequent combination of the interactions in my sample from Genoa Healthcare. And I believe that’s because they both are considered to be useful in the off-label treatment of PTSD.
Slide 2 of 9
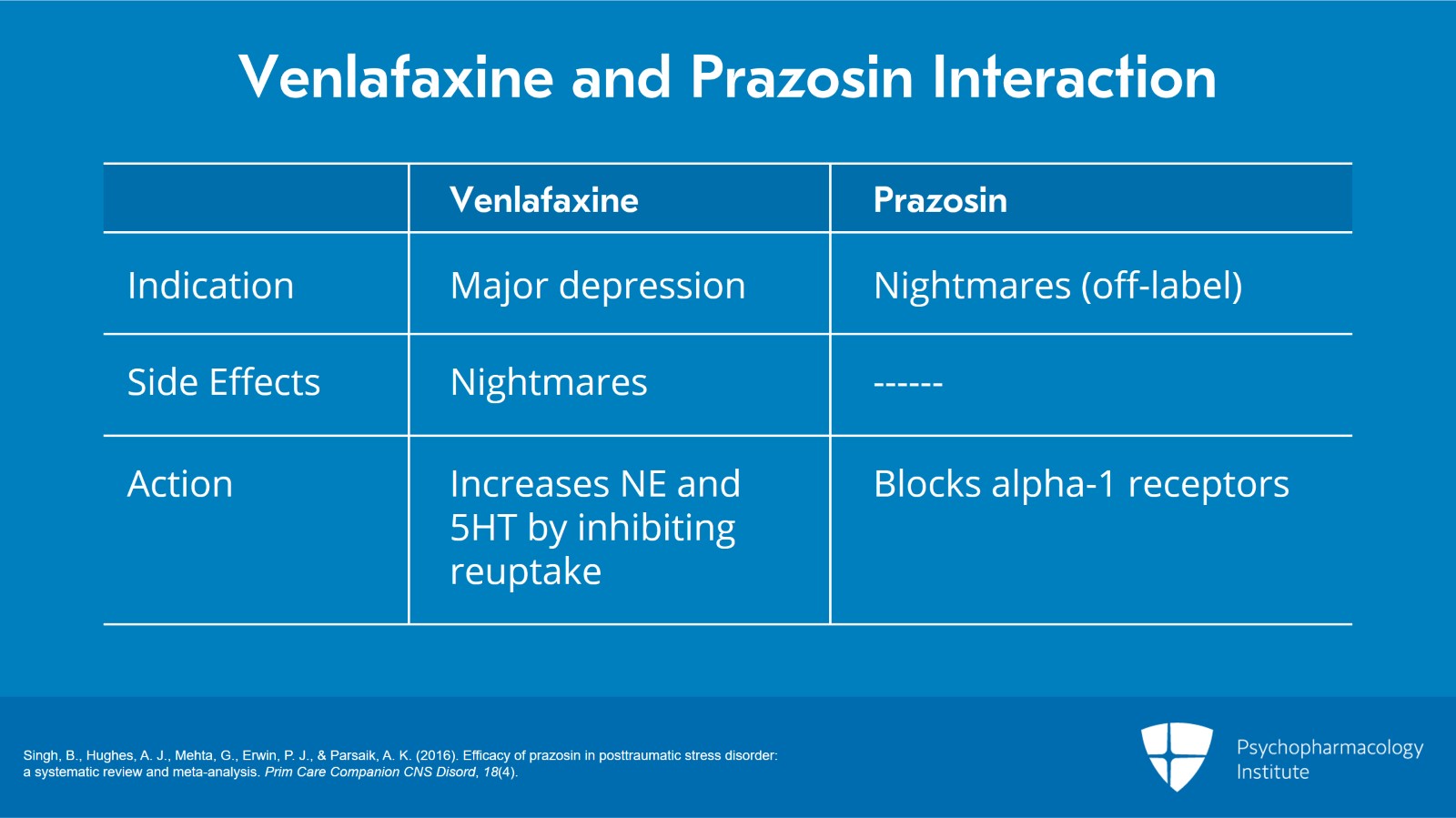
How this works is venlafaxine has an FDA indication for major depression.
However, in pre-marketing studies, 7% of patients treated with venlafaxine had nightmares versus only 2% on placebo.
In clinical practice, I believe this leads to the prescription of prazosin to treat nightmares.
And this interaction is likely at the alpha-1 receptors which prazosin blocks.
Venlafaxine increases norepinephrine and also increases serotonin through the inhibition of the reuptake in enzymes.
References:
- Singh, B., Hughes, A. J., Mehta, G., Erwin, P. J., & Parsaik, A. K. (2016). Efficacy of prazosin in posttraumatic stress disorder: a systematic review and meta-analysis. Prim Care Companion CNS Disord, 18(4).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 9
There is one similar interaction, a combination I didn’t include in my sample because I believe it should be categorized as treating the side effect of an SSRI that is unwanted.
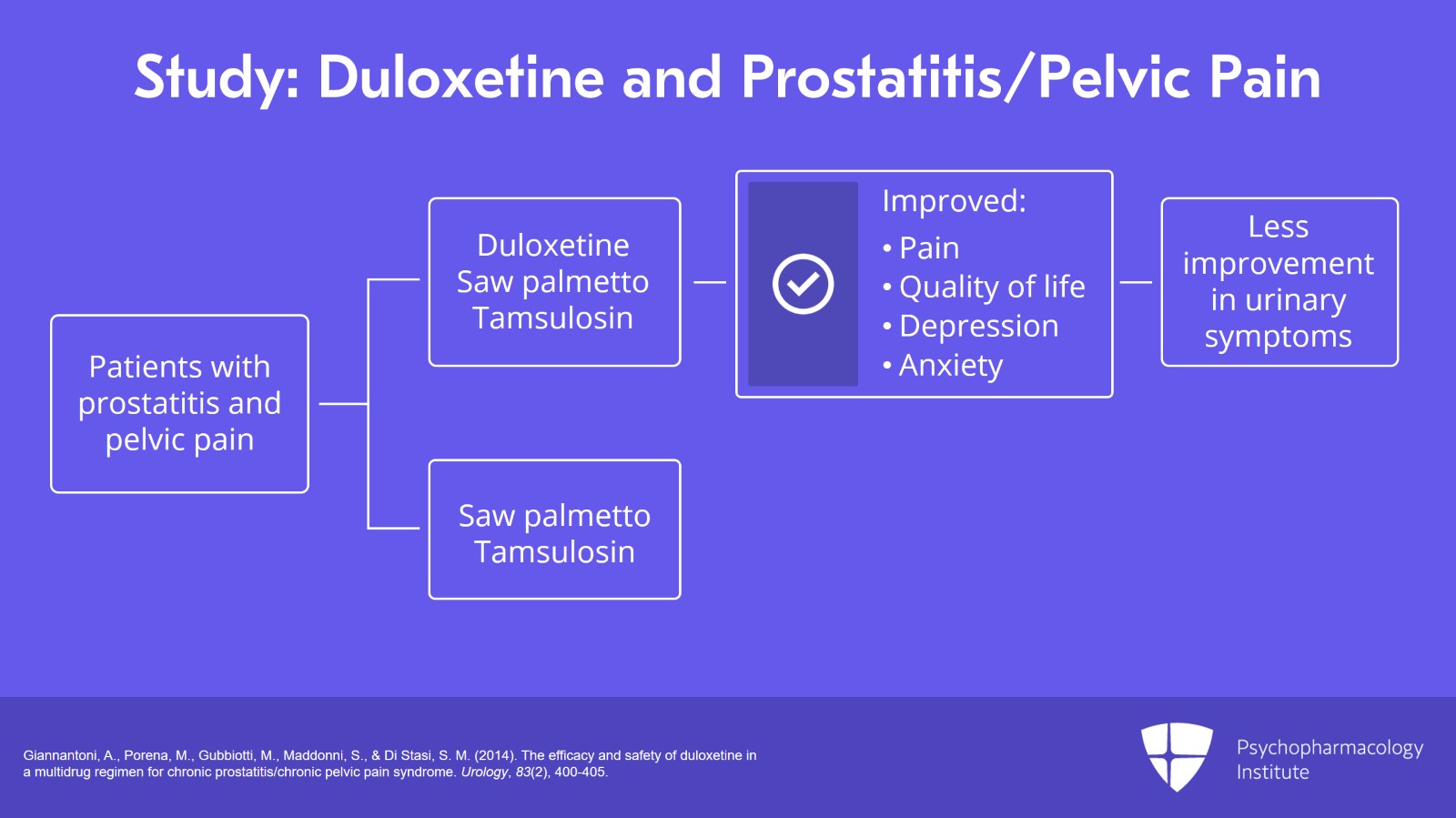
In this case, duloxetine was used in the treatment of chronic prostatitis and chronic pelvic pain syndrome.
And duloxetine when added to tamsulosin and saw palmetto was superior to just tamsulosin and saw palmetto.
And it was improvement in pain, quality of life, depression and anxiety. The pain is likely due to the unblocked beta-receptors. The quality of life, depression and anxiety likely due to duloxetine’s serotonin reuptake inhibition.
However, when they studied the urinary symptoms, they found that the patients that were given duloxetine had slightly lower or less improvement in their NIH-CPSI urinary symptoms indicating that likely the increased noradrenergic activity of duloxetine was possibly making their urinary symptoms more difficult to treat.
However, in the study, they both improved. There was only a trend difference of 0.07 between the two of them.
References:
- Giannantoni, A., Porena, M., Gubbiotti, M., Maddonni, S., & Di Stasi, S. M. (2014). The efficacy and safety of duloxetine in a multidrug regimen for chronic prostatitis/chronic pelvic pain syndrome. Urology, 83(2), 400-405.
Slide 4 of 9
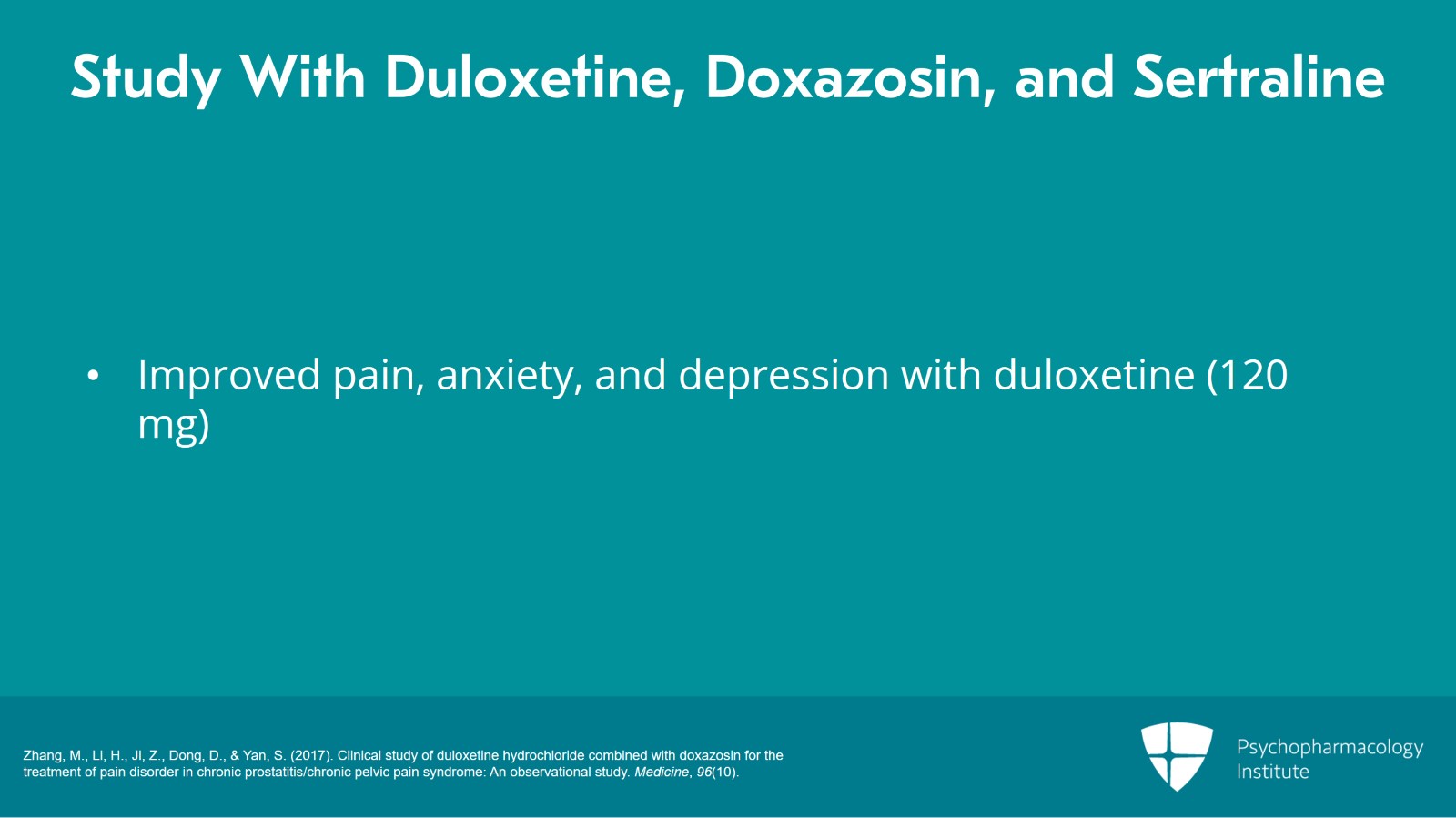
There was another study that found similar results with duloxetine, doxazosin or doxazosin and sertraline in which they found improved pain, anxiety and depression in those with duloxetine.
However, the duloxetine was titrated to 120 mg per day while the sertraline was held to 100 which I believe in clinical practice most prescribers would have gone to 200 mg for patients that were not responding.
References:
- Zhang, M., Li, H., Ji, Z., Dong, D., & Yan, S. (2017). Clinical study of duloxetine hydrochloride combined with doxazosin for the treatment of pain disorder in chronic prostatitis/chronic pelvic pain syndrome: An observational study. Medicine, 96(10).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 9
Finally, to avoid nightmares in polypharmacy, for people with PTSD, it is advisable to avoid noradrenergic-type medicines that increase noradrenergic activity.
And this is likely because patients with PTSD have been found to have increased levels of norepinephrine and its metabolites in cerebrospinal fluid. This increased norepinephrine could be the cause of their nightmares.
And the reason is because in normal sleep with REM that is when norepinephrine levels are the lowest. They’re intermediate in non-REM sleep and they’re the highest when people are awake, meaning that it is possible that in people with PTSD, with their higher levels of circulating norepinephrine, it leads to nightmares, thus the efficacy of prazosin which then blocks alpha-1 receptors and allows them to sleep peacefully and dream peacefully without nightmares.
References:
- BOEHNLEIN, J. K., & KINZIE, J. D. (2007). Pharmacologic reduction of CNS noradrenergic activity in PTSD: the case for clonidine and prazosin. Journal of Psychiatric Practice®, 13(2), 72-78.
Slide 6 of 9
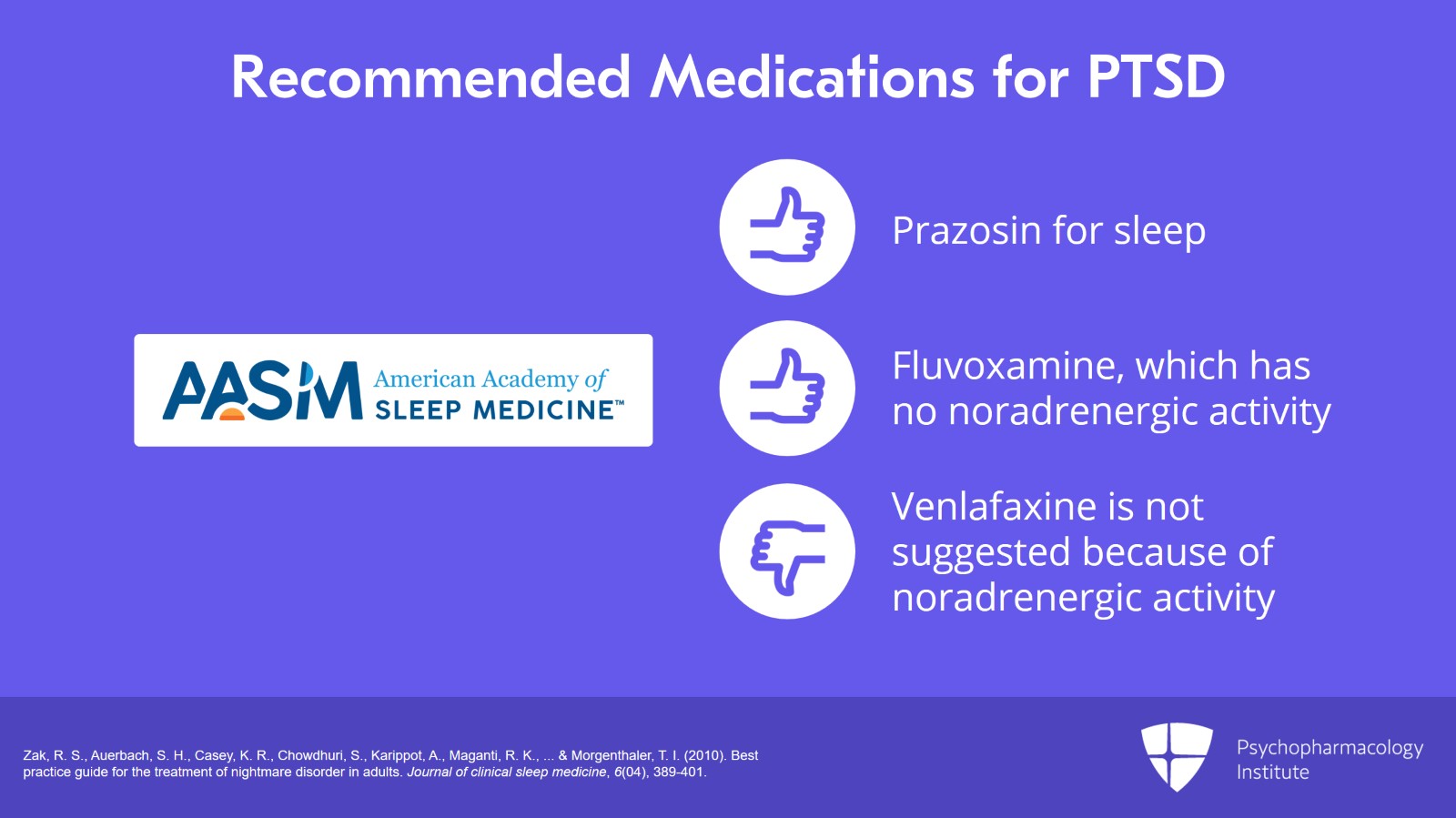
The best practices task force of the American Academy of Sleep Medicine has recommended prazosin for sleep.
Fluvoxamine which does not have noradrenergic activity may be considered.
And their lowest recommendation is for venlafaxine in which they say it’s not suggested. And that’s based on a large placebo-controlled study in which most symptoms of PTSD improved with a 12-week course but disturbing dreams did not likely because of the increased noradrenergic activity that venlafaxine offers.
References:
- Zak, R. S., Auerbach, S. H., Casey, K. R., Chowdhuri, S., Karippot, A., Maganti, R. K., … & Morgenthaler, T. I. (2010). Best practice guide for the treatment of nightmare disorder in adults. Journal of clinical sleep medicine, 6(04), 389-401.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 9
So the key points I’d like to summarize are that venlafaxine and prazosin are both prescribed in the off-label treatment of symptoms of PTSD. They have opposite effects on nightmares due to opposite action at alpha-1 receptors. SSRIs may address symptoms of PTSD without risk of exacerbating nightmares.
Slide 8 of 9
Although the noradrenergic activity of duloxetine may exacerbate urinary symptoms, this may be addressed with an alpha-1 blocker leaving the other beneficial effects of increased noradrenergic activity intact including pain reduction.
The last point, avoiding the interactions at the primary receptor of mechanism of action may improve overall efficacy of medication regimens.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.