Slides and Transcript
Slide 1 of 13
Now, we're going to talk about using clozapine for treatment-resistant psychosis as well as mood disorders. And here, I'd like to highlight several expert consensus guidelines and algorithms regarding the use of clozapine.
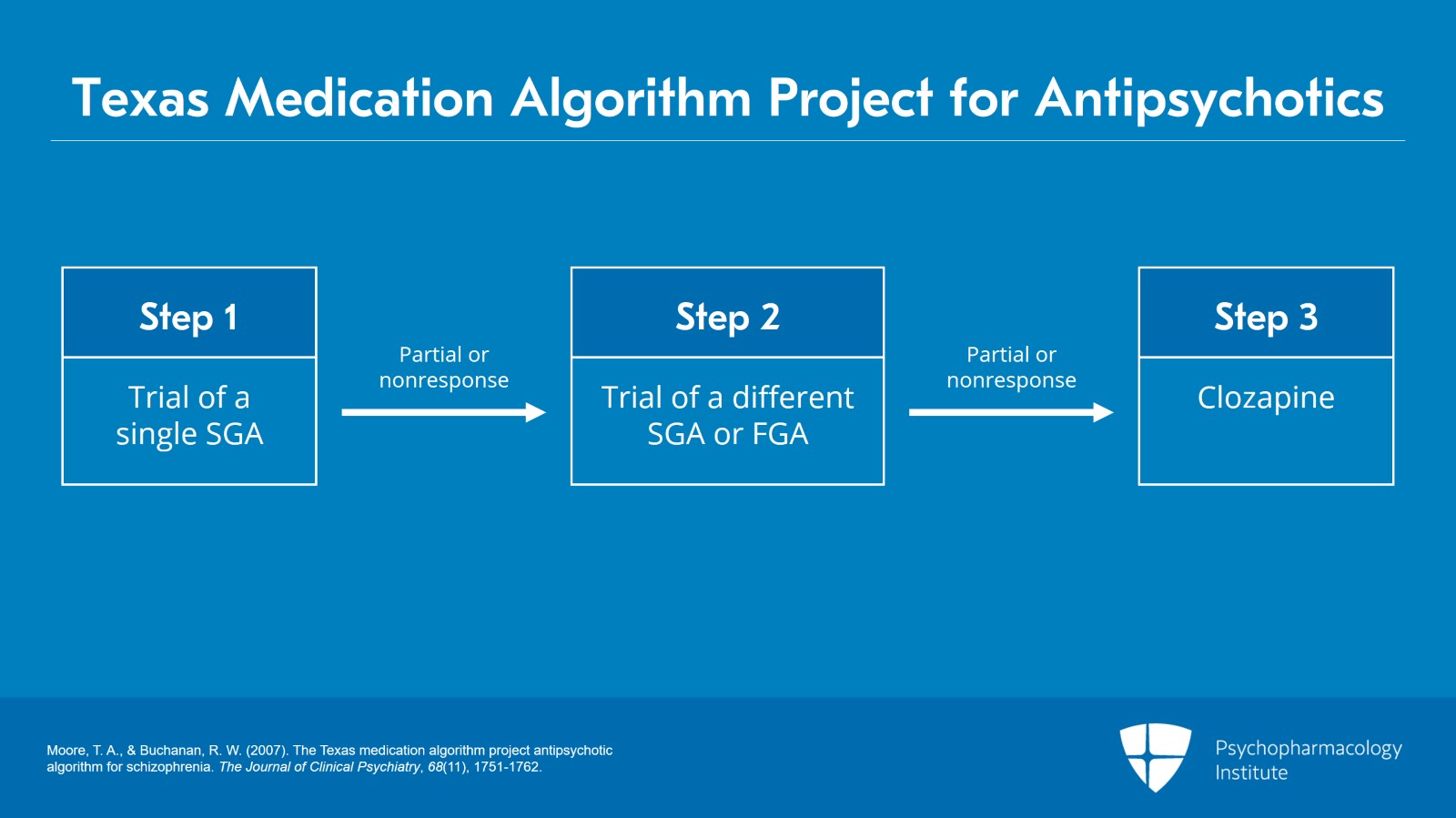
Slide 2 of 13
So beginning with treatment-resistant psychosis, there are three such guidelines that I'd like to share with you. The first is the so-called TMAP or Texas Medication Algorithm Project for antipsychotics. Step one in that algorithm is a trial of a single second-generation antipsychotic for an adequate dose and duration. If the patient has only a partial or nonresponse, step two is a trial of a different single second-generation antipsychotic or alternatively a first-generation antipsychotic. And again, if after an adequate trial in terms of dose and duration there's a partial or nonresponse, stage three would be a trial of clozapine.
References:
- Moore, T. A., & Buchanan, R. W. (2007). The Texas medication algorithm project antipsychotic algorithm for schizophrenia. The Journal of Clinical Psychiatry, 68(11), 1751-1762.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 13
I think this is very interesting because those of us who treat patients with schizophrenia and other psychotic disorders when we take a psychiatric history and we ask about what antipsychotic medications the patient has taken in the past, it's not uncommon to get a laundry list of five, six or even more different antipsychotics that they've been tried on. And when we ask about have you ever heard of clozapine or were you ever on clozapine, there's kind of a deer-in-headlights look that we receive. Yet, this particular algorithm suggests clozapine is third line after just two failed trials.
References:
- Moore, T. A., & Buchanan, R. W. (2007). The Texas medication algorithm project antipsychotic algorithm for schizophrenia. The Journal of Clinical Psychiatry, 68(11), 1751-1762.
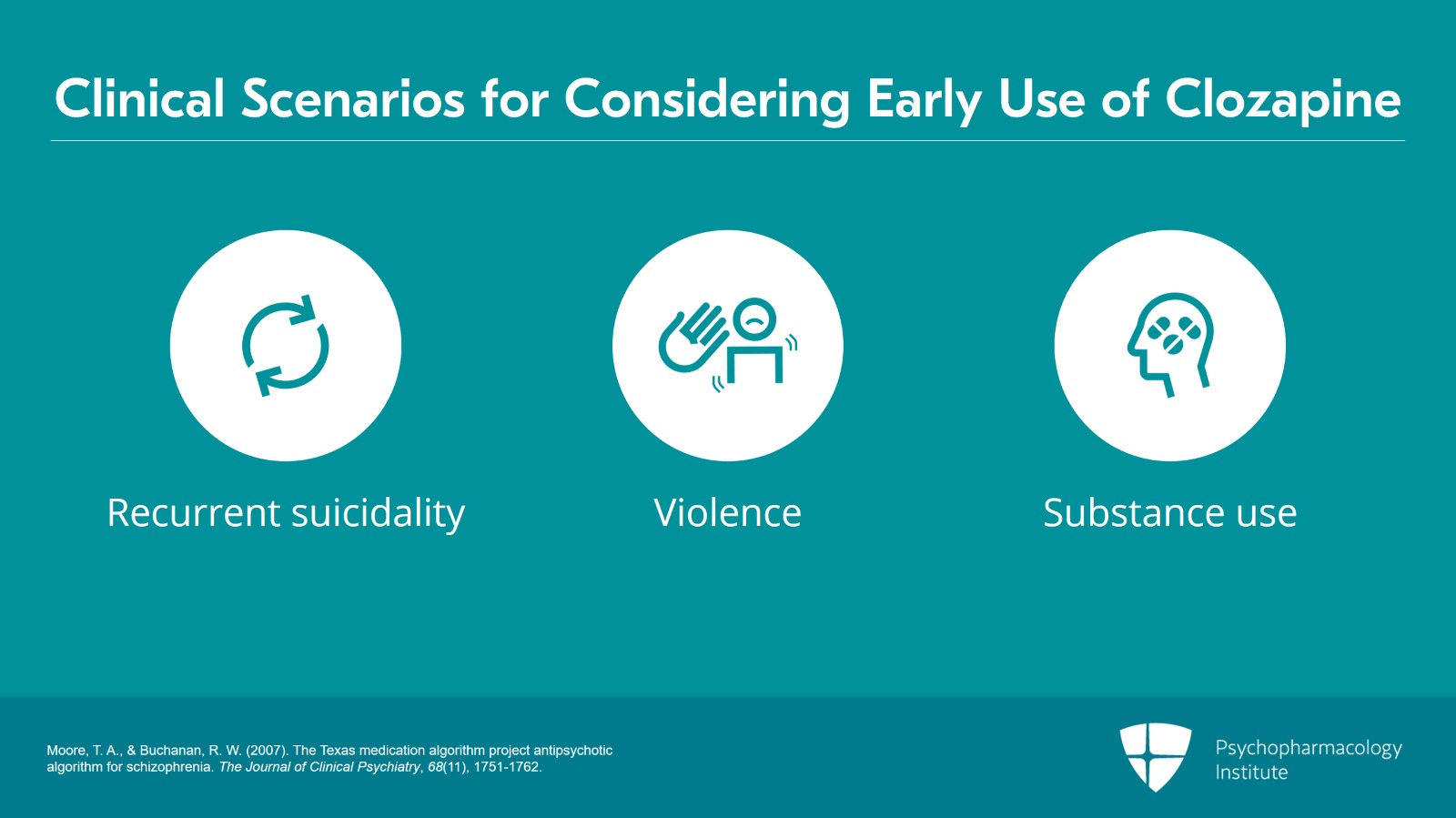
Slide 4 of 13
And even more importantly, clozapine could be considered earlier in this algorithm in patients who have a history of recurrent suicidality, violence, or substance use comorbidity, so exactly what we were discussing previously about clozapine's indication.
References:
- Moore, T. A., & Buchanan, R. W. (2007). The Texas medication algorithm project antipsychotic algorithm for schizophrenia. The Journal of Clinical Psychiatry, 68(11), 1751-1762.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 13
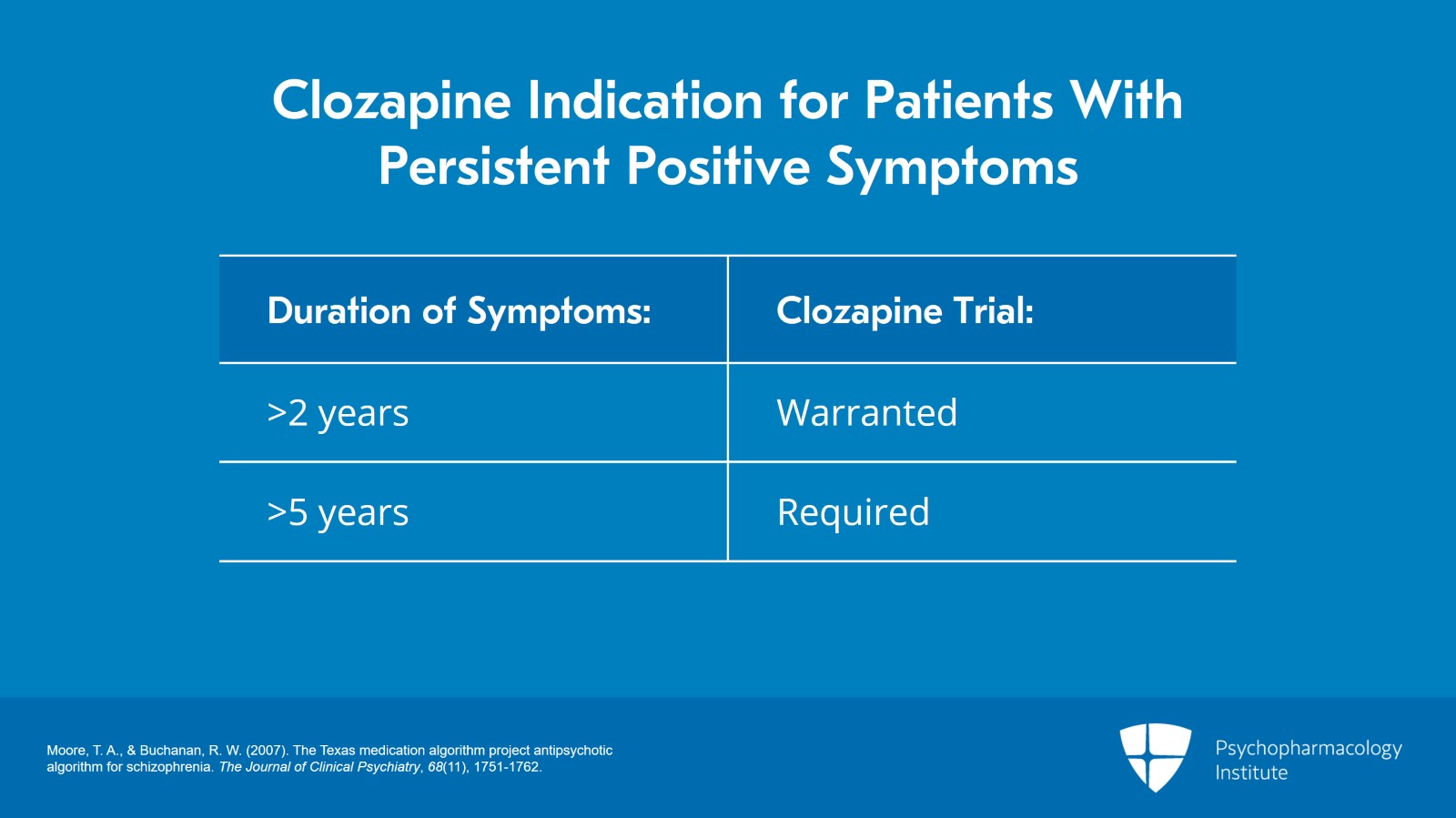
Nevertheless, if patients have persistent positive symptoms of psychosis (hallucinations and delusions) for more than two years warrants and more than five years really requires a clozapine trial. I try to instill in our psychiatry residents that it would be almost tantamount to malpractice to not at least offer a clozapine trial for a patient who has had such a degree of persistent positive symptoms.
References:
- Moore, T. A., & Buchanan, R. W. (2007). The Texas medication algorithm project antipsychotic algorithm for schizophrenia. The Journal of Clinical Psychiatry, 68(11), 1751-1762.
Slide 6 of 13
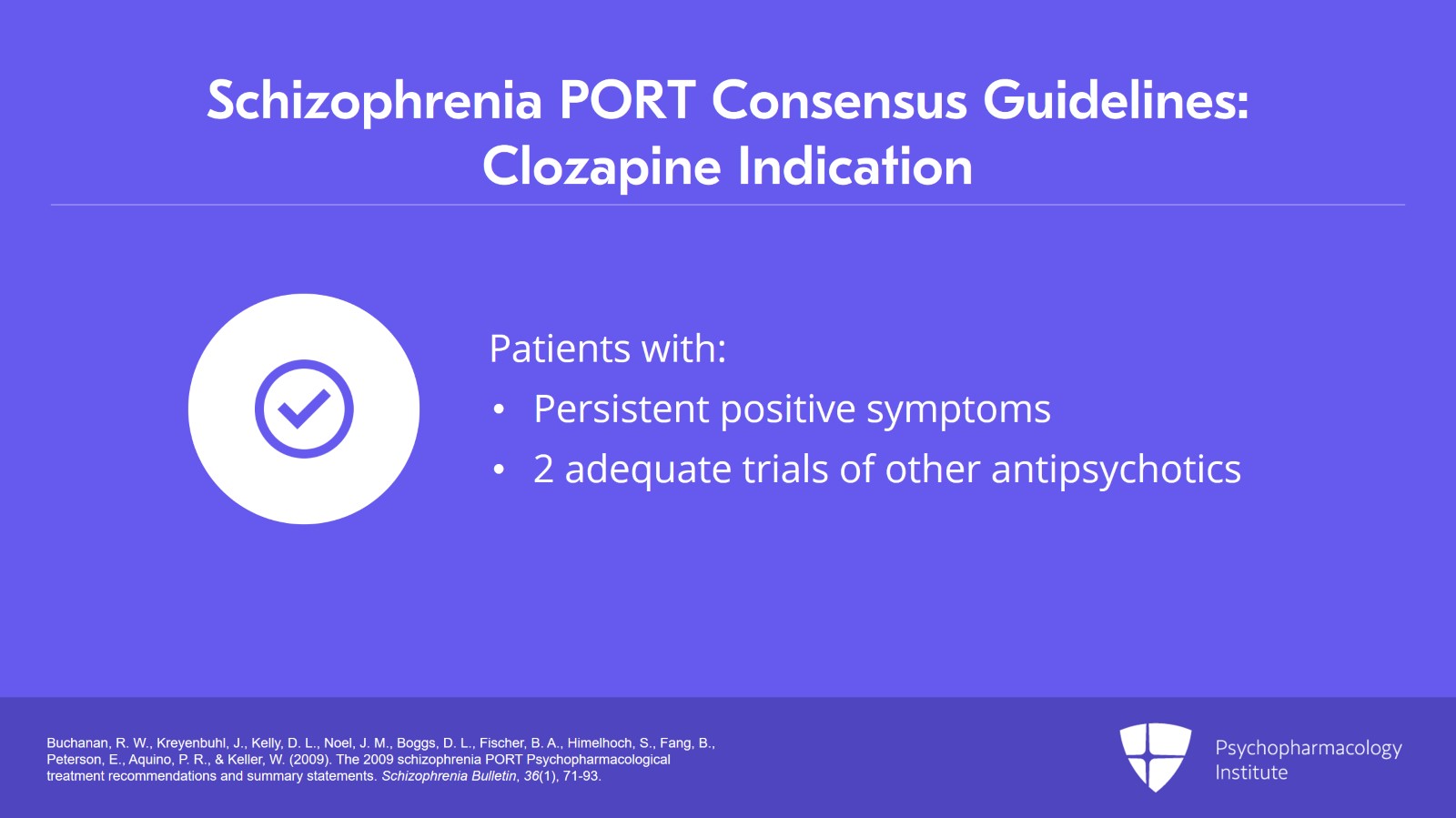
I also rely heavily on the schizophrenia PORT expert consensus guidelines. Those are the Patient Outcomes Research Team expert consensus guidelines which, very similar to the TMAP, argue that clozapine should be offered to people with schizophrenia who experience persistent and clinically significant positive symptoms after two adequate trials of other antipsychotic agents.
References:
- Buchanan, R. W., Kreyenbuhl, J., Kelly, D. L., Noel, J. M., Boggs, D. L., Fischer, B. A., Himelhoch, S., Fang, B., Peterson, E., Aquino, P. R., & Keller, W. (2009). The 2009 schizophrenia PORT Psychopharmacological treatment recommendations and summary statements. Schizophrenia Bulletin, 36(1), 71-93.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 13
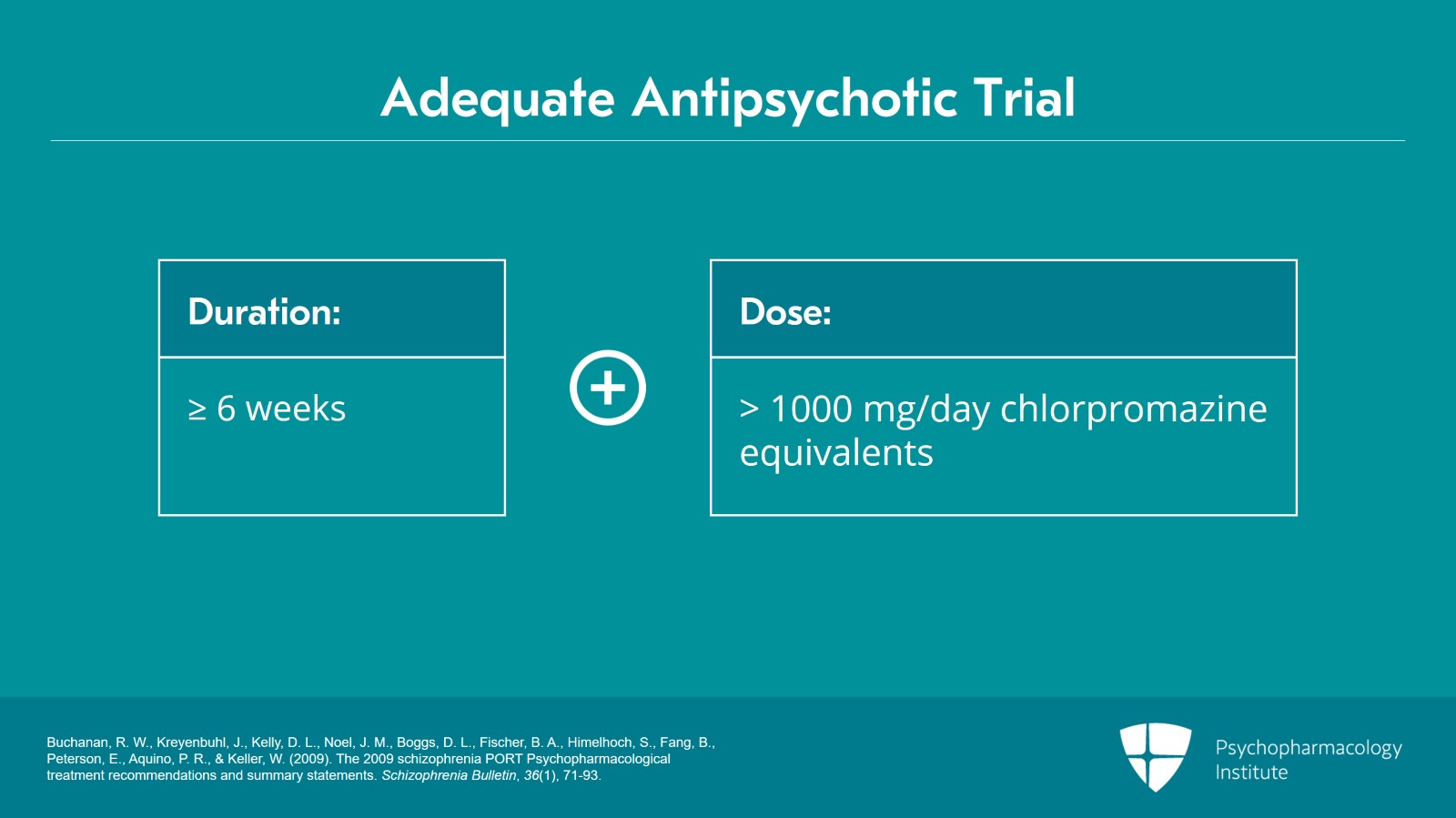
And here, I think this gets to kind of an important definition. We've been saying an adequate trial and that's often defined as at least six weeks at a dose of 1000 mg per day chlorpromazine equivalents.
References:
- Buchanan, R. W., Kreyenbuhl, J., Kelly, D. L., Noel, J. M., Boggs, D. L., Fischer, B. A., Himelhoch, S., Fang, B., Peterson, E., Aquino, P. R., & Keller, W. (2009). The 2009 schizophrenia PORT Psychopharmacological treatment recommendations and summary statements. Schizophrenia Bulletin, 36(1), 71-93.
Slide 8 of 13
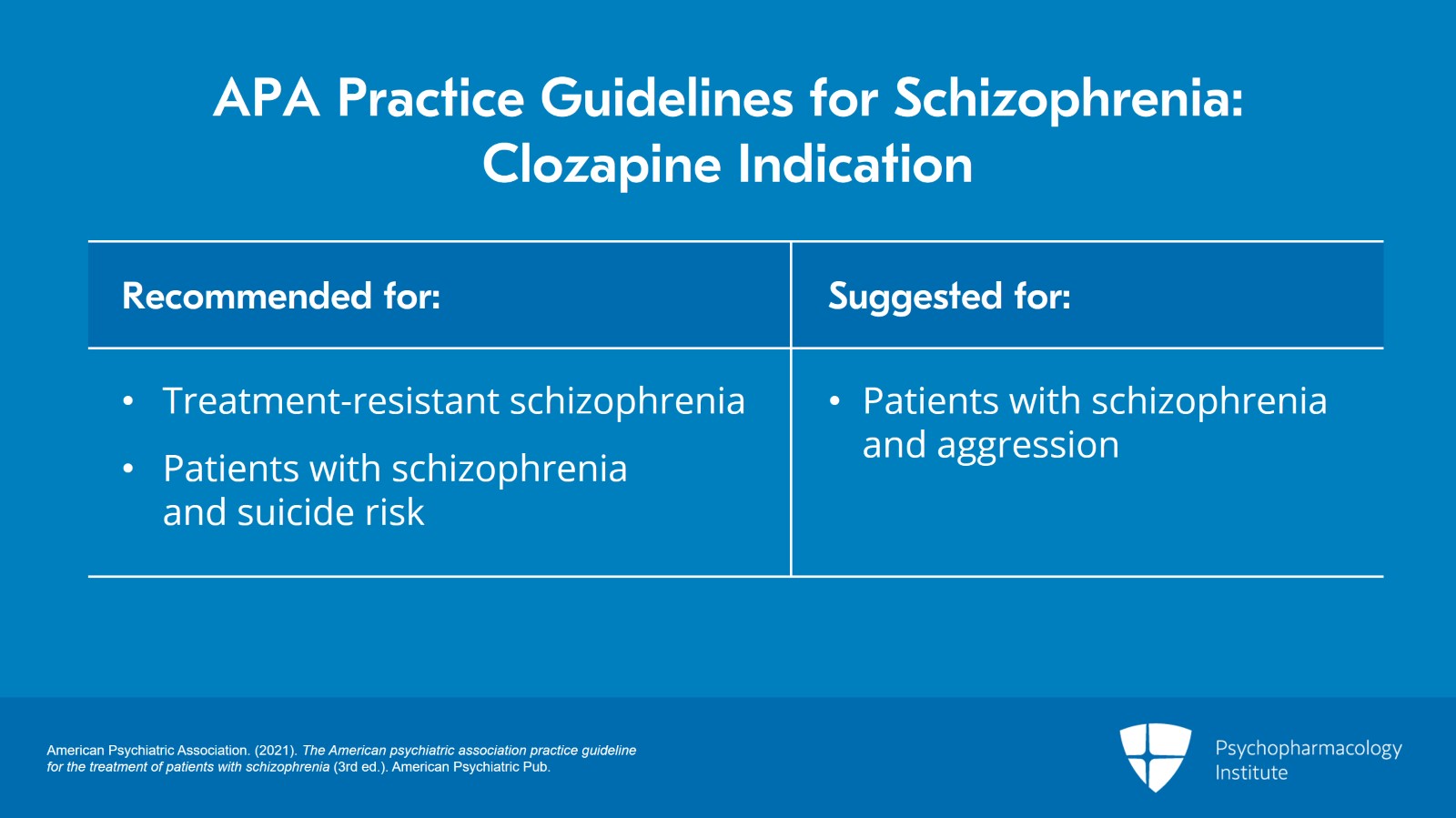
And then most recently, we have the new American Psychiatric Association practice guidelines for schizophrenia, third edition and those guidelines recommend clozapine for patients with treatment-resistant schizophrenia but also patients with schizophrenia and substantial suicide risk despite other treatments. These guidelines also suggest clozapine for patients with schizophrenia and substantial aggression risk despite other treatments.
References:
- American Psychiatric Association. (2021). The American psychiatric association practice guideline for the treatment of patients with schizophrenia (3rd ed.). American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 13
So as you can see, all of these guidelines are really hammering this point home that for schizophrenia, the gold standard for resistant illness is clozapine and that clozapine should potentially play a role in the treatment of our patients with schizophrenia who have significant risks of suicide and aggression.
References:
- Moore, T. A., & Buchanan, R. W. (2007). The Texas medication algorithm project antipsychotic algorithm for schizophrenia. The Journal of Clinical Psychiatry, 68(11), 1751-1762.
- Buchanan, R. W., Kreyenbuhl, J., Kelly, D. L., Noel, J. M., Boggs, D. L., Fischer, B. A., Himelhoch, S., Fang, B., Peterson, E., Aquino, P. R., & Keller, W. (2009). The 2009 schizophrenia PORT Psychopharmacological treatment recommendations and summary statements. Schizophrenia Bulletin, 36(1), 71-93.
Slide 10 of 13
In terms of mood disorders, clozapine is not just for patients with psychosis. There's evidence for mood disorders and there are randomized controlled trials as well as open-label studies that have shown modest evidence for mood stabilization in bipolar disorder and there are a number of case reports for improvements in psychotic major depressive disorder with clozapine.
References:
- Green, A. I., Tohen, M., Patel, J. K., Banov, M., DuRand, C., Berman, I., Chang, H., Zarate, C., Jr, Posener, J., Lee, H., Dawson, R., Richards, C., Cole, J. O., & Schatzberg, A. F. (2000). Clozapine in the treatment of refractory psychotic mania. The American Journal of Psychiatry, 157(6), 982–986.
- Jeyapaul, P., & Vieweg, R. (2006). A case study evaluating the use of clozapine in depression with psychotic features. Annals of General Psychiatry, 5(1).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 13
So in review, clozapine is recommended for patients with schizophrenia who have failed two adequate trials of other antipsychotics. The APA practice guidelines also recommend clozapine for patients with schizophrenia who are at significant risk of suicide and suggest it for patients who have substantial risk of aggression.
Slide 12 of 13
There's also modest evidence for off-label clozapine use in both bipolar disorder and psychotic depression.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.