Slides and Transcript
Slide 1 of 27
Welcome to the video number 2, Understanding the Relationship Between Insomnia Disorder and Major Depressive Disorder.
Slide 2 of 27
What changes occur in the sleep architecture in patients with major depressive disorder?
In terms of parameters of sleep continuity, patients with major depressive disorder report increased sleep onset latency, increased wake after sleep onset time, decreased total sleep time and decreased sleep efficiency.
For example, a person suffering with major depressive disorder and insomnia who actually slept for four hours and were in bed for a period of eight hours would have a reduced sleep efficiency of 50% only.
References:
- Chopra, Das, Doghramji (2020). Management of Sleep Disorders. (First Ed.). Oxford University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 27
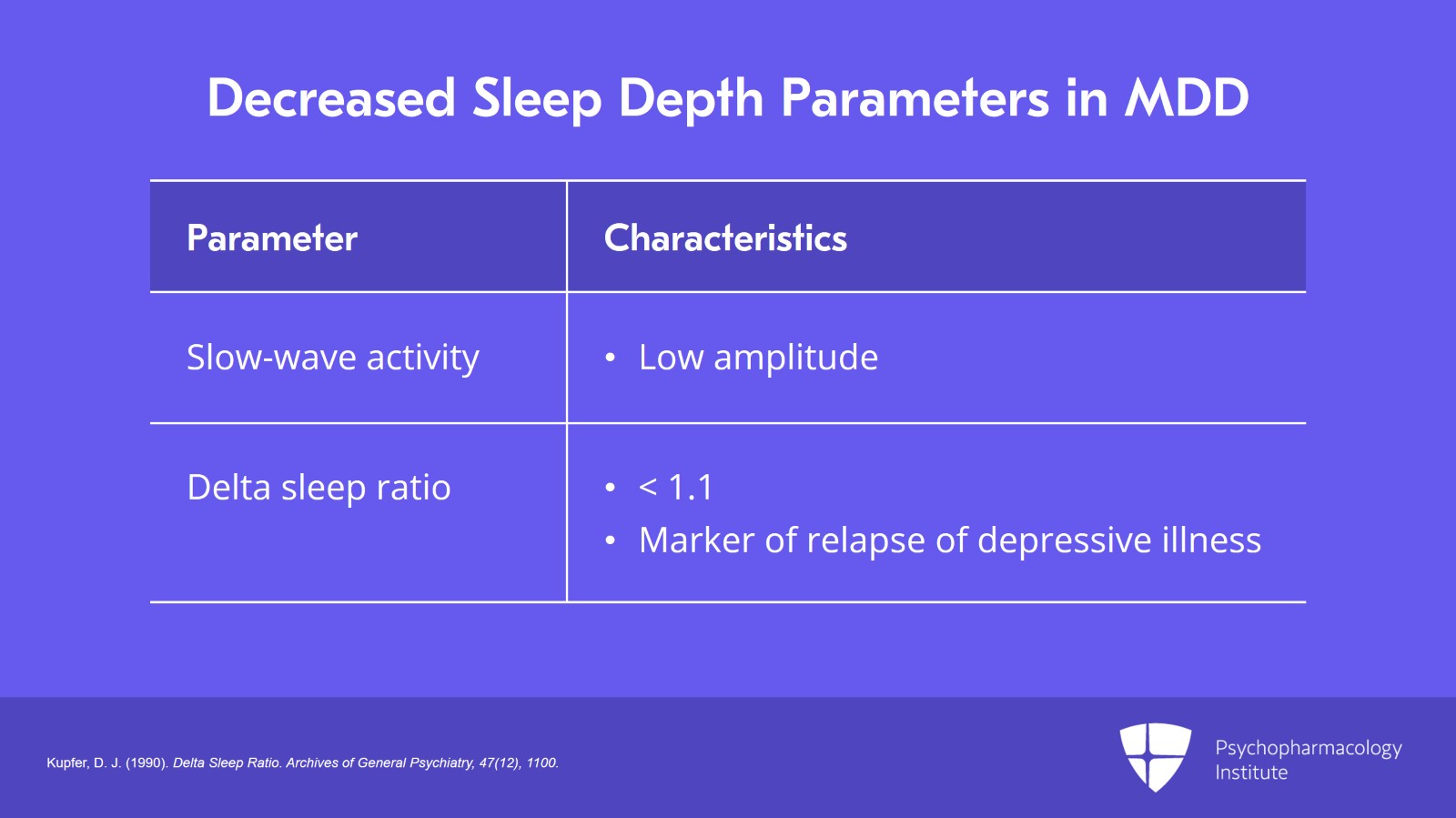
In terms of parameters of sleep depth, patients with major depressive disorder have been shown to have reduced slow-wave activity and reduced delta sleep ratio with a value less than 1.1.
Low delta sleep ratio has been identified as a marker of relapse of depressiveness in patients with major depressive disorder.
Additionally, slow waves during sleep may have a lower amplitude in patients with major depressive disorder as compared to the healthy controls.
References:
- Kupfer, D. J. (1990). Delta Sleep Ratio. Archives of General Psychiatry, 47(12), 1100.
Slide 4 of 27
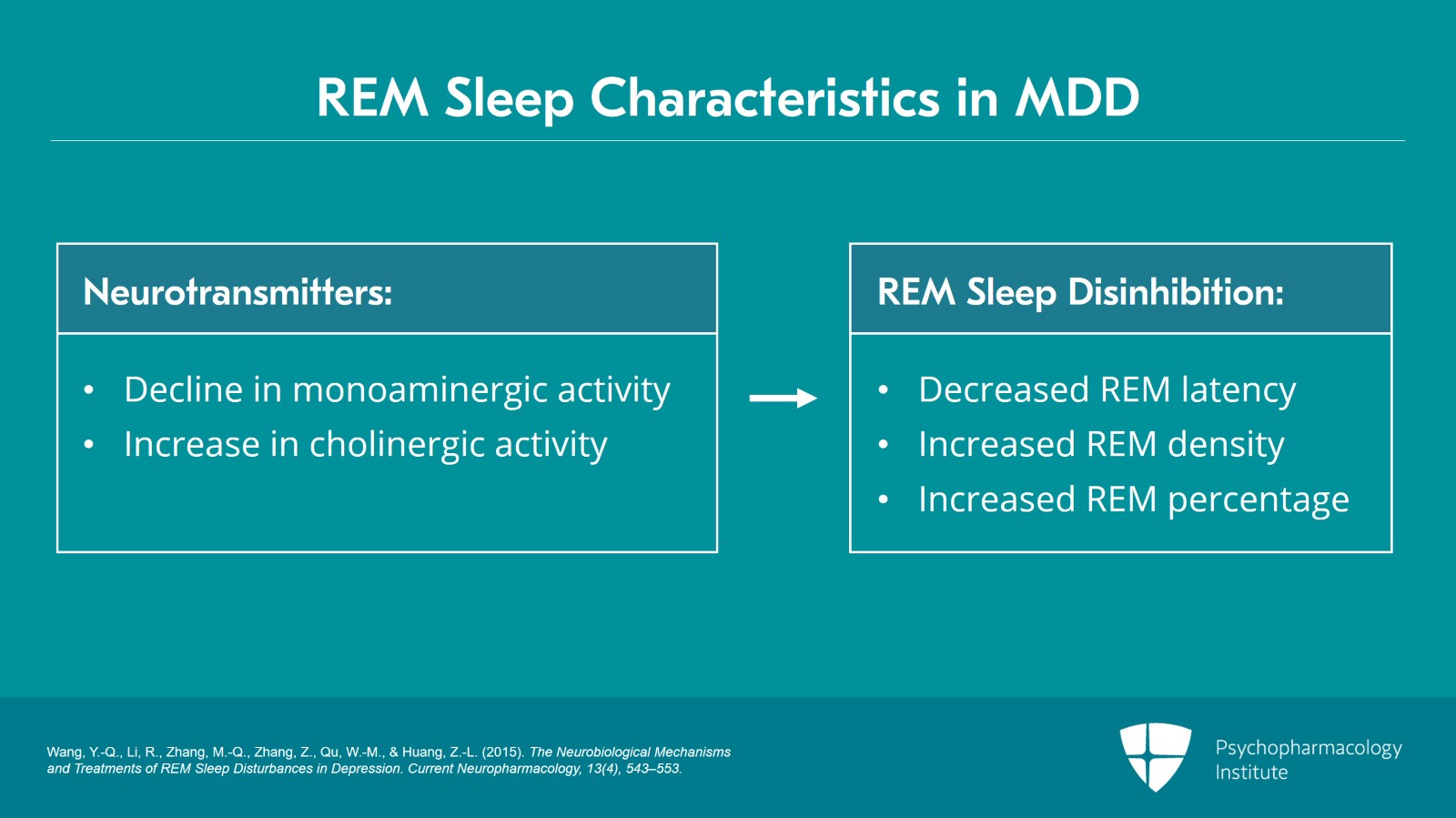
REM sleep onset is associated with a decline in monoaminergic activity and an increase in cholinergic activity. This explains REM sleep disinhibition in major depressive disorder which is characterized by monoaminergic-cholinergic imbalance with decreased monoaminergic activity and increased cholinergic activity.
Major depressive disorder is characterized by a state of REM sleep disinhibition as suggested by decreased REM latency, increased REM density and increased REM percentage.
References:
- Wang, Y.-Q., Li, R., Zhang, M.-Q., Zhang, Z., Qu, W.-M., & Huang, Z.-L. (2015). The Neurobiological Mechanisms and Treatments of REM Sleep Disturbances in Depression. Current Neuropharmacology, 13(4), 543–553.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 27
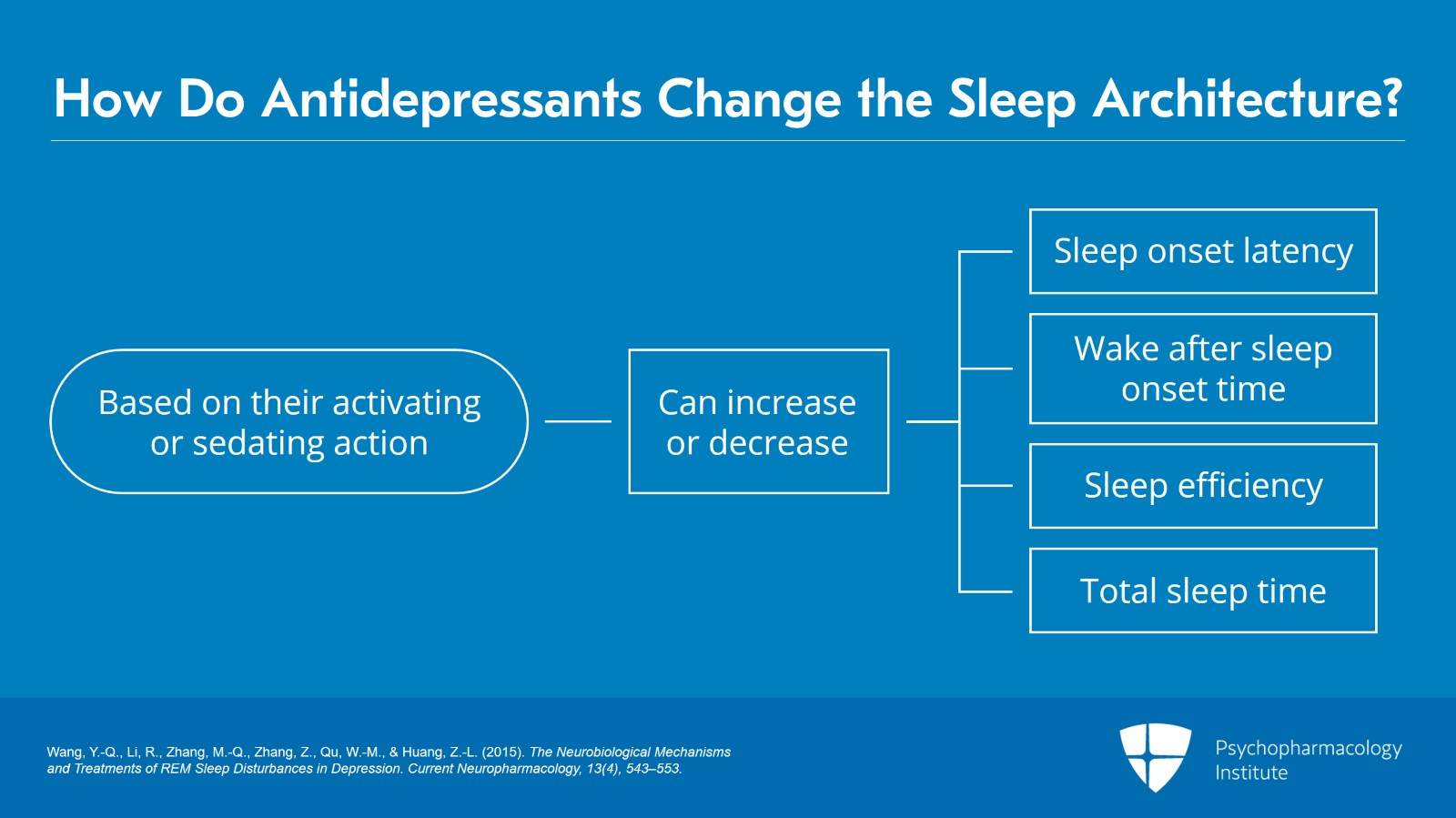
How do antidepressants change the sleep architecture?
In terms of parameters of sleep continuity based on their activating or sedating action, antidepressants can either increase or decrease sleep onset latency and wake after sleep onset time. Similarly, total sleep time and sleep efficiency can be increased or decreased based on activating or sedating actions of the antidepressants.
References:
- Wang, Y.-Q., Li, R., Zhang, M.-Q., Zhang, Z., Qu, W.-M., & Huang, Z.-L. (2015). The Neurobiological Mechanisms and Treatments of REM Sleep Disturbances in Depression. Current Neuropharmacology, 13(4), 543–553.
Slide 6 of 27
With regards to parameters of sleep depth, it is postulated that 5-HT2A and 2C receptor antagonist action of sedating antidepressants such as trazodone and mirtazapine is associated with an increase in slow-wave sleep.
References
References:
- Wichniak, A., Wierzbicka, A., Walęcka, M., & Jernajczyk, W. (2017). Effects of Antidepressants on Sleep. Current Psychiatry Reports, 19(9).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 27
In terms of REM sleep parameters, majority of the antidepressants except bupropion, trazodone and mirtazapine, tend to act as REM sleep suppressants as suggested by these medications causing an increase in REM latency, a decrease in REM density and REM duration and overall REM percentage.
References:
- Wang, Y.-Q., Li, R., Zhang, M.-Q., Zhang, Z., Qu, W.-M., & Huang, Z.-L. (2015). The Neurobiological Mechanisms and Treatments of REM Sleep Disturbances in Depression. Current Neuropharmacology, 13(4), 543–553.
Slide 8 of 27
The mechanism of REM suppression action of antidepressants is believed to be related to the reversal of monoaminergic-cholinergic imbalance which is characteristic of major depressive disorder.
The clinical consequences of REM suppression caused by antidepressants can be a change in the frequency and intensity of dreaming as well as exacerbation of intense disturbing dreams related to REM rebound upon antidepressant discontinuation.
References:
- Wichniak, A., Wierzbicka, A., Walęcka, M., & Jernajczyk, W. (2017). Effects of Antidepressants on Sleep. Current Psychiatry Reports, 19(9).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 27
There are some very important changes in the definition and diagnostic criteria for insomnia in DSM-5. Insomnia is now called as insomnia disorder and the categories of primary versus secondary insomnia have been removed. This is a very important step going forward as insomnia is now increasingly viewed as an independent disorder and not caused by psychiatric or medical disorders.
References:
- American Psychiatric Association. (2013). Cautionary statement for forensic use of DSM-5. In Diagnostic and statistical manual of mental disorders (5th ed.).
Slide 10 of 27
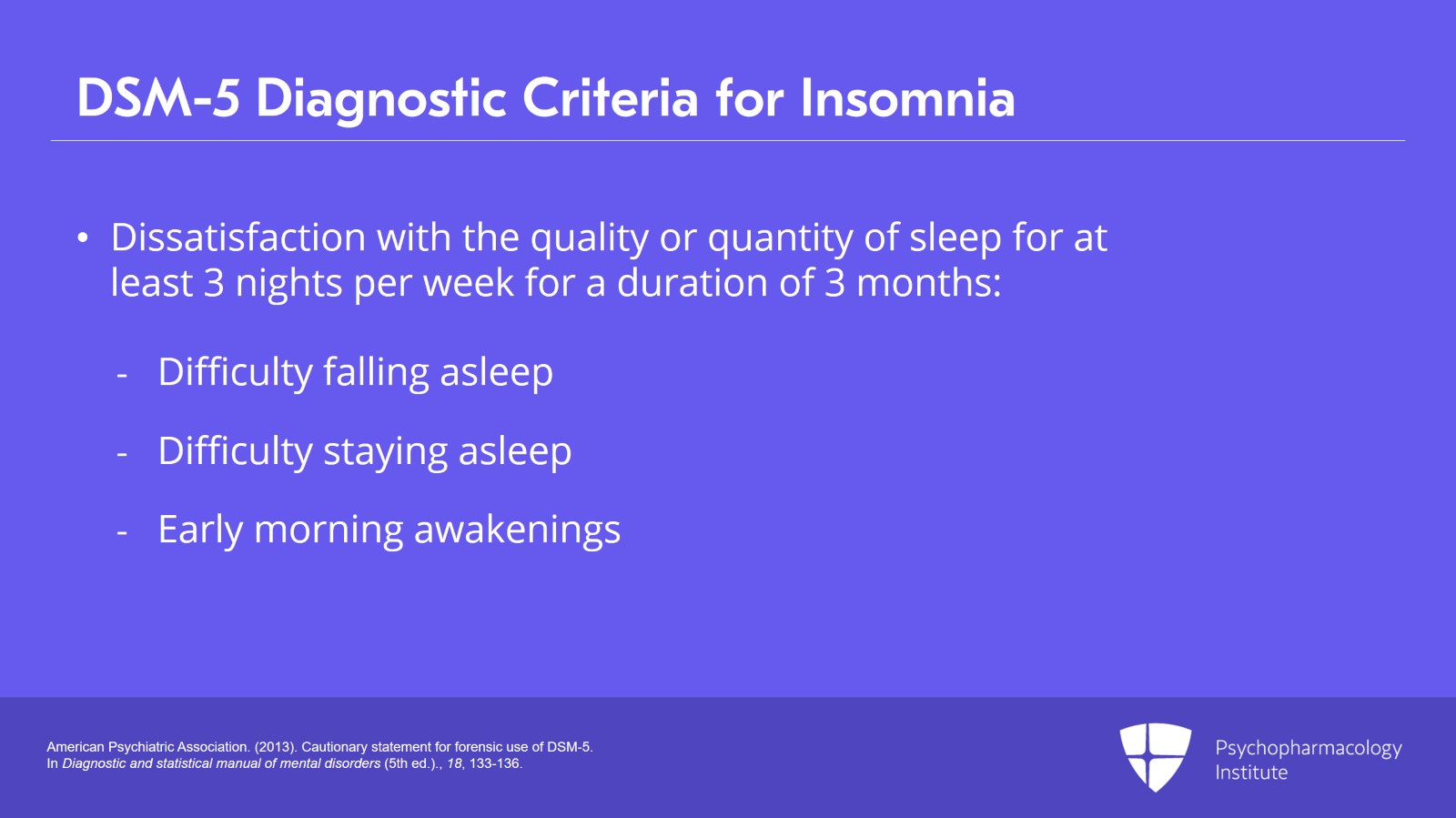
The diagnostic criteria have changed as well with changes in sleep quality and quantity that occurs at least three nights per week for a duration of three months.
The diagnostic criteria for insomnia disorder include dissatisfaction with the quality or quantity of sleep associated with one or more of the following.
These include difficulty falling asleep, difficulty staying asleep or early morning awakenings even when there is enough time for sleep and the sleep disturbance usually causes significant distress or impairment in social, occupational or other important area of functioning.
References:
- American Psychiatric Association. (2013). Cautionary statement for forensic use of DSM-5. In Diagnostic and statistical manual of mental disorders (5th ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 27
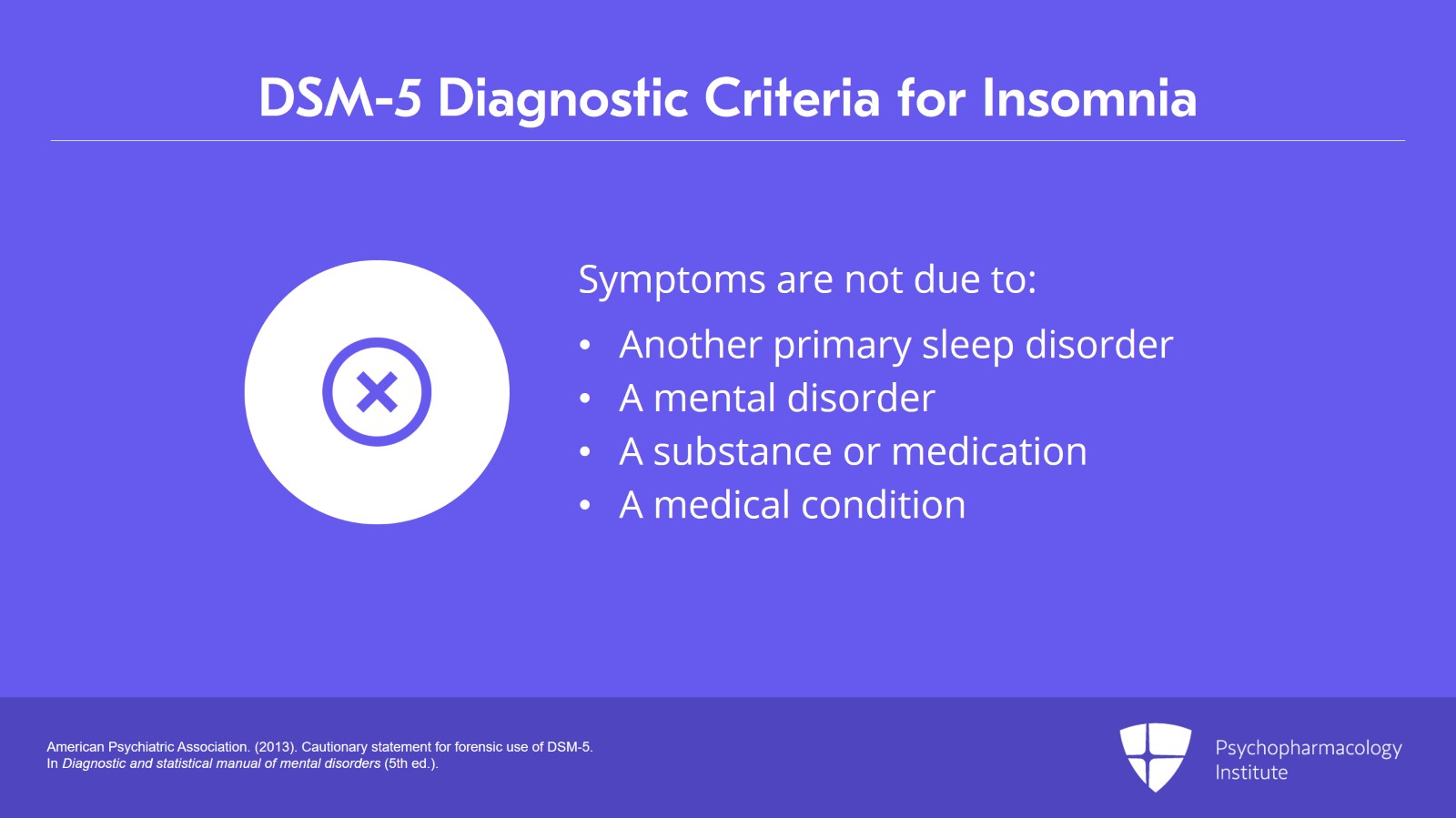
Additionally, the sleep disturbance does not occur exclusively during the course of another primary sleep disorder, mental disorder and it is not due to the direct physiological effect of substance or medication or from a general medical condition.
References:
- American Psychiatric Association. (2013). Cautionary statement for forensic use of DSM-5. In Diagnostic and statistical manual of mental disorders (5th ed.).
Slide 12 of 27
Occasional short-term insomnia lasting for a few weeks affects 30% to 50% of the general population. The prevalence of insomnia disorder in industrialized nations is estimated to be at least 5% to 10%. The prevalence of insomnia disorder is significantly higher in medically and psychiatrically ill populations as well as in females and elderly.
References:
- Riemann, D., Nissen, C., Palagini, L., Otte, A., Perlis, M. L., & Spiegelhalder, K. (2015). The neurobiology, investigation, and treatment of chronic insomnia. The Lancet Neurology, 14(5), 547–558.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 27
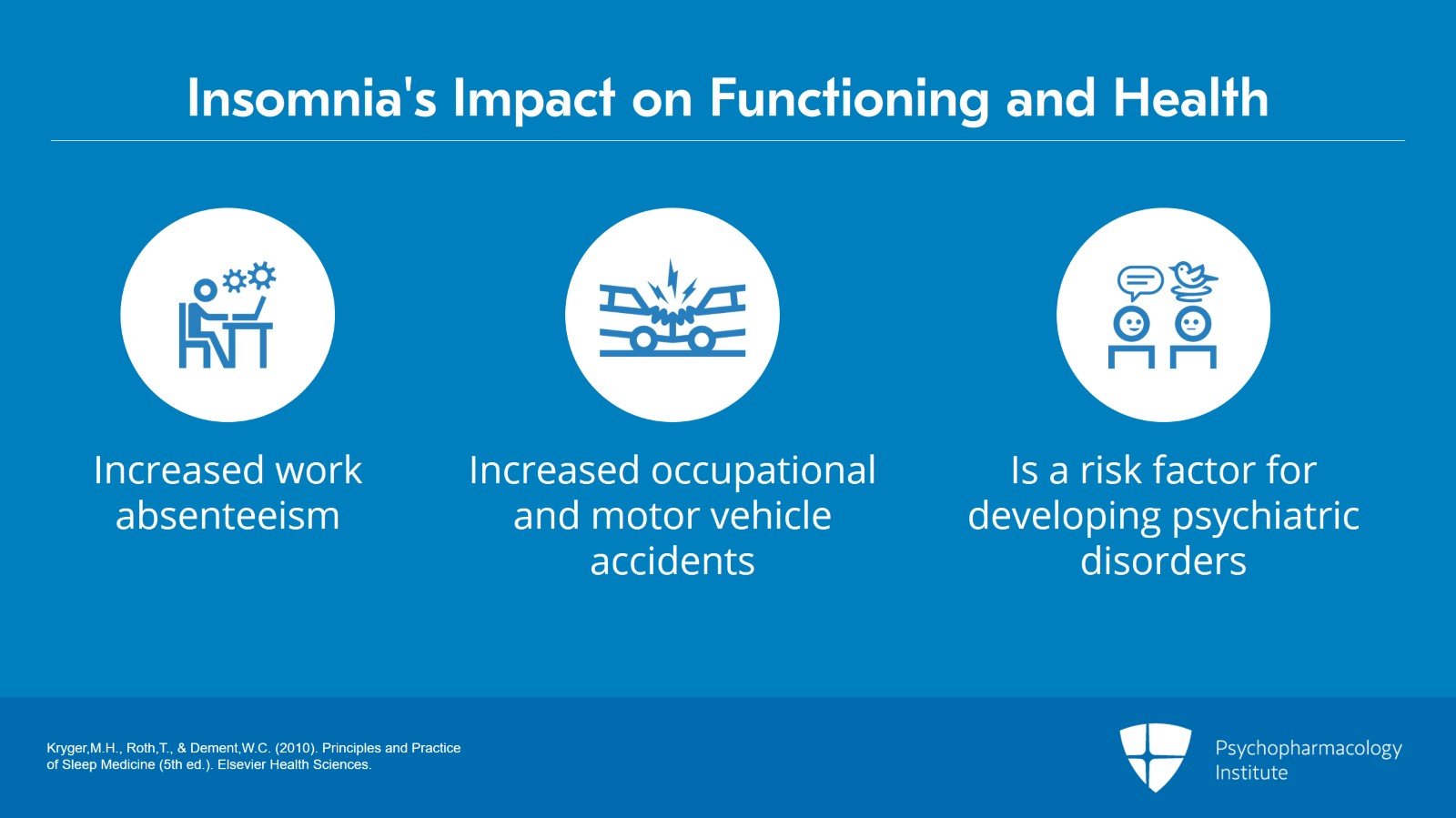
Insomnia disorder is associated with numerous adverse effects on general functioning, health and quality of life. Epidemiological studies demonstrate marked impairment in functional status among those with insomnia disorder with increased rates of work absenteeism and occupational and motor vehicle accidents have been widely reported in patients with insomnia disorder. Additionally, insomnia disorder has been identified in multiple studies as a significant risk factor for development of psychiatric disorders especially mood disorders such as major depressive disorder.
References:
- Kryger,M.H., Roth,T., & Dement,W.C. (2010). Principles and Practice of Sleep Medicine (5th ed.). Elsevier Health Sciences.
Slide 14 of 27
What are the key brain changes that underlie the neurobiology of insomnia?
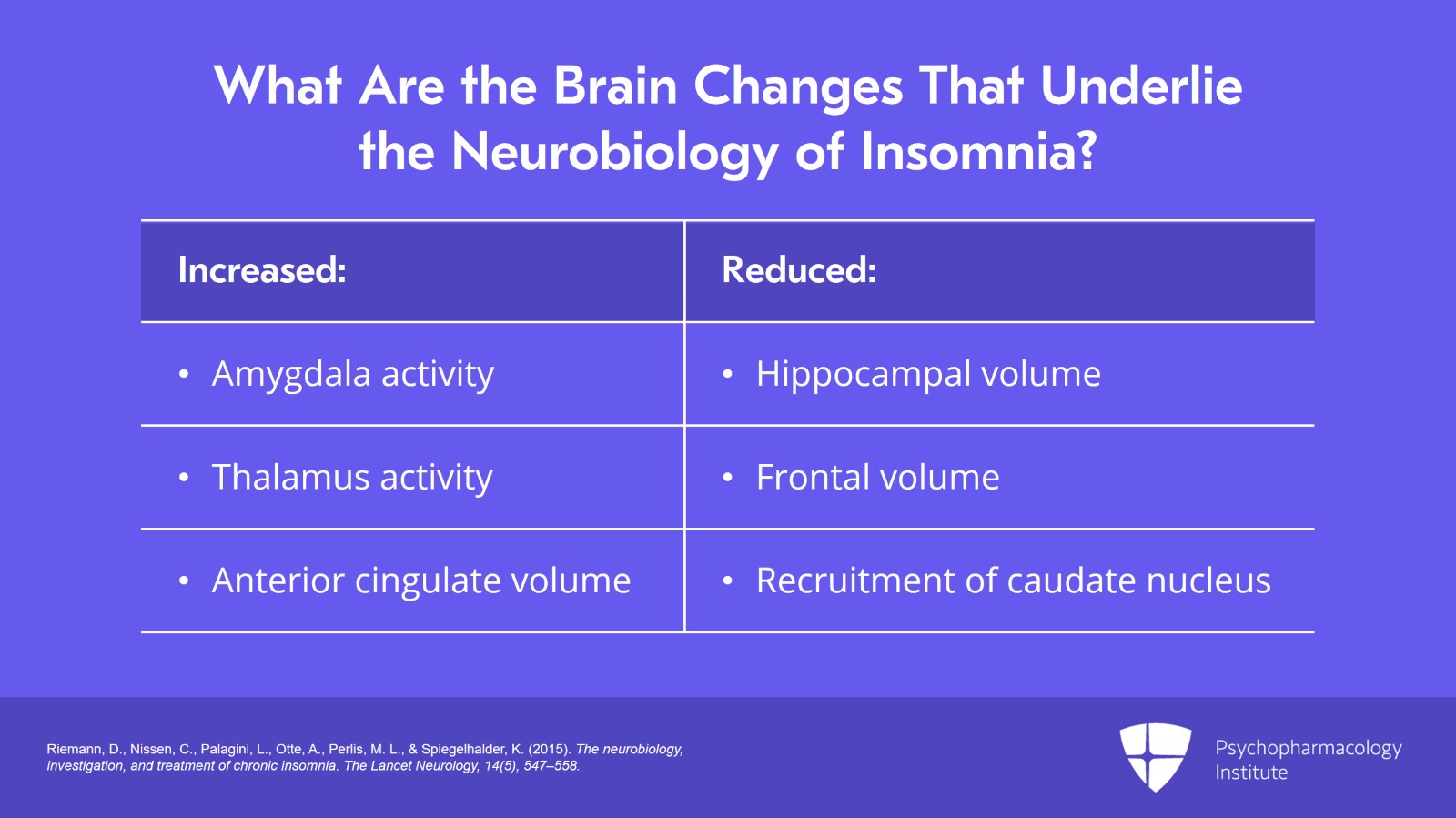
Insomnia disorder has been associated with increased activity of brain structures including amygdala and thalamus and increased anterior cingulate volume.
Additionally, reduced hippocampal volume, reduced frontal volume in task-related activity and reduced recruitment of caudate nucleus has been associated with insomnia disorder.
References:
- Riemann, D., Nissen, C., Palagini, L., Otte, A., Perlis, M. L., & Spiegelhalder, K. (2015). The neurobiology, investigation, and treatment of chronic insomnia. The Lancet Neurology, 14(5), 547–558.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 27
Not surprisingly, some of these brain structures are common neural substrates for major depressive disorder as well.
It has been demonstrated in a neuroimaging study that patients with major depressive disorder and severe insomnia symptoms were noted to have reduced cortical surface area in the frontoparietal regions.
Notably, the associations between surface area in frontoparietal cortical areas and insomnia are unique to depression as these associations were not observed among healthy or clinical control subjects with bipolar disorder.
References:
- Leerssen, J., Blanken, T. F., Pozzi, E., Jahanshad, N., Aftanas, L., Andreassen, O. A., … & Van Someren, E. J. (2020). Brain structural correlates of insomnia severity in 1053 individuals with major depressive disorder: results from the ENIGMA MDD Working Group. Translational psychiatry, 10(1), 425.
Slide 16 of 27
The scientific description of association between insomnia and major depression dates back to 1600s when Greek physicians described the co-occurrence of insomnia and depression in the Anatomy of Melancholia and later did the founder of modern psychiatry, Kraepelin in the early 1900s.
References:
- Riemann, D., Krone, L. B., Wulff, K., & Nissen, C. (2019). Sleep, insomnia, and depression. Neuropsychopharmacology.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 27
We know that an episode of depression is commonly associated with insomnia symptoms that can persist as insomnia disorder even if depression remits.
Approximately 90% of the patients with major depressive disorder present with sleep complaints and the majority of the patients present with insomnia which is characterized by difficulty initiating or maintaining sleep and early morning awakenings.
References:
- Riemann, D., Krone, L. B., Wulff, K., & Nissen, C. (2019). Sleep, insomnia, and depression. Neuropsychopharmacology.
Slide 18 of 27
On the other hand, insomnia disorder can present as a depressive episode due to overlapping symptoms of sleep disturbances, low energy levels, attention and concentration changes, irritability and mood changes. Depressive symptoms associated with insomnia disorder are usually mild to moderate in severity.
Presence of sadness, guilt, hypersomnia and change in appetite have been reported to differentiate depression from insomnia disorder.
References:
- Gupta, R., Victor, R., & Garg, S. (2019). Insomnia and depression: How much is the overlap? Indian Journal of Psychiatry, 61(6), 623.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 27
Data from large prospective studies suggest that insomnia is a risk factor for the onset of depression. Based on meta-analytic studies, as compared to those with good sleep, adult patients with insomnia are 2.6 times more likely to develop depression.
In adolescents, the risk of developing depression is four times higher in those with insomnia disorder compared to those without insomnia.
References:
- Baglioni, C., Spiegelhalder, K., Nissen, C., & Riemann, D. (2011). Clinical implications of the causal relationship between insomnia and depression: how individually tailored treatment of sleeping difficulties could prevent the onset of depression. Epma Journal, 2, 287-293.
Slide 20 of 27
It may not be all bad news as insomnia being a risk factor for development of major depression gives us an opportunity for the prevention of depression by optimally treating insomnia disorder.
References:
- Baglioni, C., Spiegelhalder, K., Nissen, C., & Riemann, D. (2011). Clinical implications of the causal relationship between insomnia and depression: how individually tailored treatment of sleeping difficulties could prevent the onset of depression. Epma Journal, 2, 287-293.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 27
What impact insomnia can have on the severity, treatment and the course of major depressive disorder.
When insomnia disorder and major depressive disorder are comorbid, we are dealing with two major mental health disorders and their associated consequences. So, the depressive symptom severity is understandably higher and the quality of life for the patients with this comorbidity has been shown to be lower as compared to those with either disorders alone.
References:
- Chopra, A., Das, P., & Doghramji, K. (2020). Management of sleep disorders in psychiatry. Oxford University Press.
Slide 22 of 27
Patients with comorbid insomnia and major depressive disorder usually don’t respond to conventional treatments as well as compared to patients with MDD only.
It has been proven by multiple lines of evidence that insomnia is a risk factor for treatment-resistant depression.
In fact, persistent insomnia is the most common residual symptom in patients with major depressive disorder and it is also considered as an important predictor of depression relapse.
References:
- Chopra, A., Das, P., & Doghramji, K. (2020). Management of sleep disorders in psychiatry. Oxford University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 27
Insomnia is the most common residual symptom following remission from major depression occurring in 44% to 51% of the treatment responders following cognitive behavioral therapy or pharmacotherapy for major depressive disorder.
Major depressive disorder patients with residual insomnia symptoms are three to six times more likely to relapse than major depressive disorder patients in full remission and relapse may occur more quickly in the presence of residual insomnia symptoms.
In other words, if we can optimally treat insomnia disorder, then we can prevent the relapse of depression.
References:
- Franzen, P. L., & Buysse, D. J. (2008). Sleep disturbances and depression: Risk relationships for subsequent depression and therapeutic implications. Dialogues in Clinical Neuroscience, 10(4), 473-481.
Slide 24 of 27
Finally, insomnia has been noted to be a modifiable risk factor for suicide attempts and completed suicides independent of the depression severity. The sleep disturbances that are associated with increased suicidality include sleep disturbances most nights of the week, short sleep duration typically less than four hours per night, presence of nightmares and early morning awakenings.
References:
- Liu, R. T., Steele, S. J., Hamilton, J. L., Do, Q. B. P., Furbish, K., Burke, T. A., … Gerlus, N. (2020). Sleep and suicide: A systematic review and meta-analysis of longitudinal studies. Clinical Psychology Review, 101895.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 25 of 27
Key points.
Major depressive disorder is associated with sleep architectural changes including decreased slow-wave activity and REM sleep disinhibition during sleep.
Reduced delta sleep ratio is considered to be a trait marker of major depressive disorder.
Insomnia disorder has a bidirectional relationship and it shares common neurobiological substrates with major depressive disorder.
Insomnia disorder has been associated with significantly high risk of developing depression across lifespan.
Slide 26 of 27
Insomnia disorder comorbid with major depressive disorder has been associated with increased depression severity, poor treatment response and increased risk of relapse of major depressive disorder.
Insomnia is a risk factor for suicide independent of major depression. Clinical features such as short sleep duration, sleep disturbance most nights during the week, nightmares and early morning awakenings have been associated with an increased suicide risk in patients with major depression.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.