Slides and Transcript
Slide 1 of 20
So next, we’re going to talk in more detail about some of the patient, caregiver, and environmental factors that can underlie the development of behavioral and psychological symptoms of dementia.
Slide 2 of 20
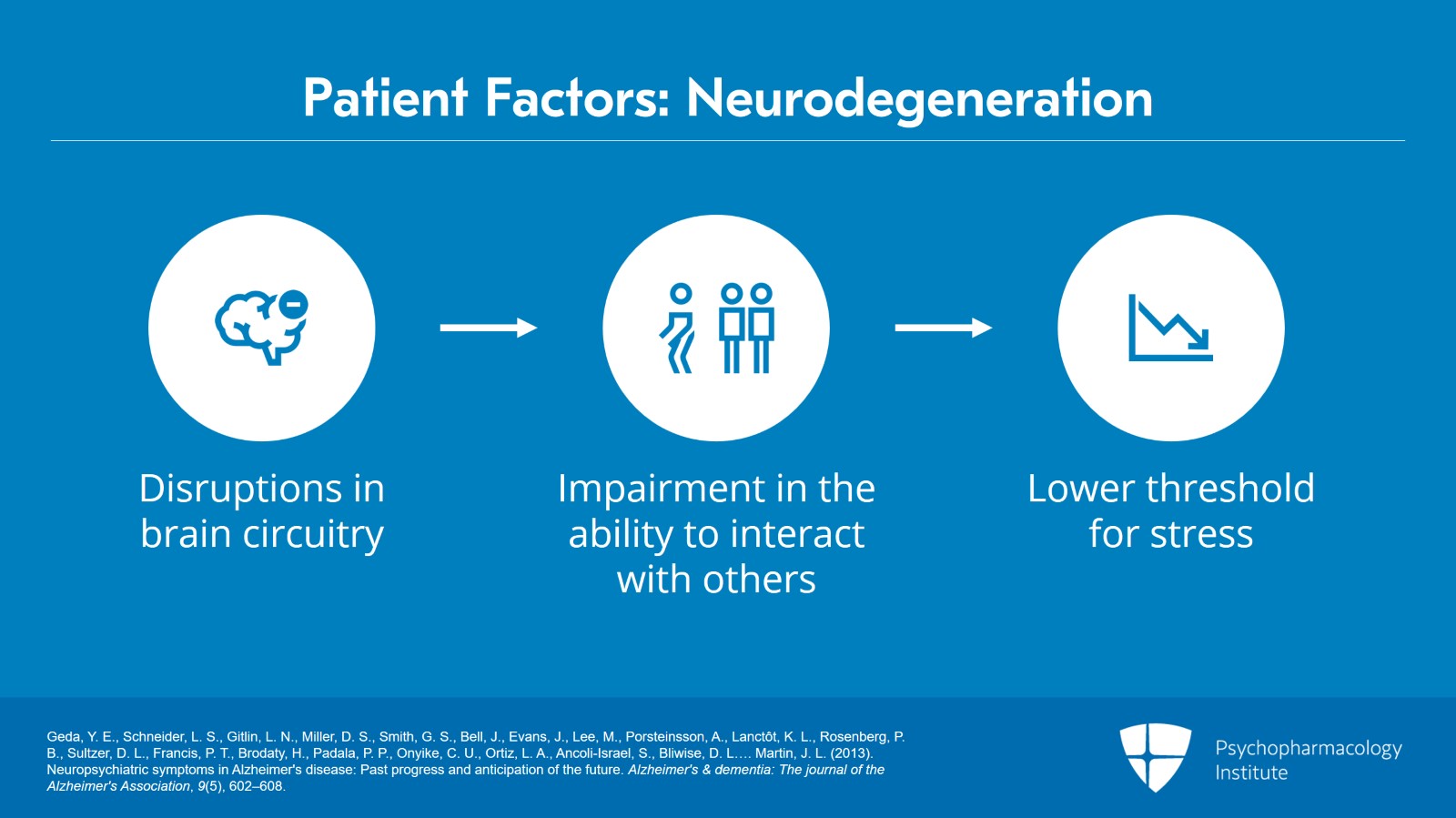
So really starting with the person with dementia. So, during and through the neurodegeneration that happens in Alzheimer’s disease and related dementia, there are disruptions and breakdown in the brain circuitry in centers of the brain that are involved in emotion and cognition. And this can really impair the ability of the person with dementia to interact with others and interact with the environment. And this can really lead to a situation where the person with dementia has a lower threshold for stress in an environment.
References:
- Geda, Y. E., Schneider, L. S., Gitlin, L. N., Miller, D. S., Smith, G. S., Bell, J., Evans, J., Lee, M., Porsteinsson, A., Lanctôt, K. L., Rosenberg, P. B., Sultzer, D. L., Francis, P. T., Brodaty, H., Padala, P. P., Onyike, C. U., Ortiz, L. A., Ancoli-Israel, S., Bliwise, D. L.… Martin, J. L. (2013). Neuropsychiatric symptoms in Alzheimer's disease: Past progress and anticipation of the future. Alzheimer's & dementia: The journal of the Alzheimer's Association, 9(5), 602–608.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 20
There are also other person with dementia factors to consider. So acute medical issues can often be the underlying trigger or cause for behavioral disturbance. And studies with community dwelling older adults with dementia have found that over a third of patients who are experiencing new behavioral disturbances have some undetected medical illness associated with these behaviors.
And that can include things like infections, like a urinary tract infection or pneumonia. It can include other lab abnormalities like hypothyroidism or anemia or pain or constipation can often be a cause of these behavioral disturbances.
References:
- Hodgson, N. A., Gitlin, L. N., Winter, L., & Czekanski, K. (2011). Undiagnosed illness and neuropsychiatric behaviors in community residing older adults with dementia. Alzheimer disease and Associated Disorders, 25(2), 109–115.
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 4 of 20
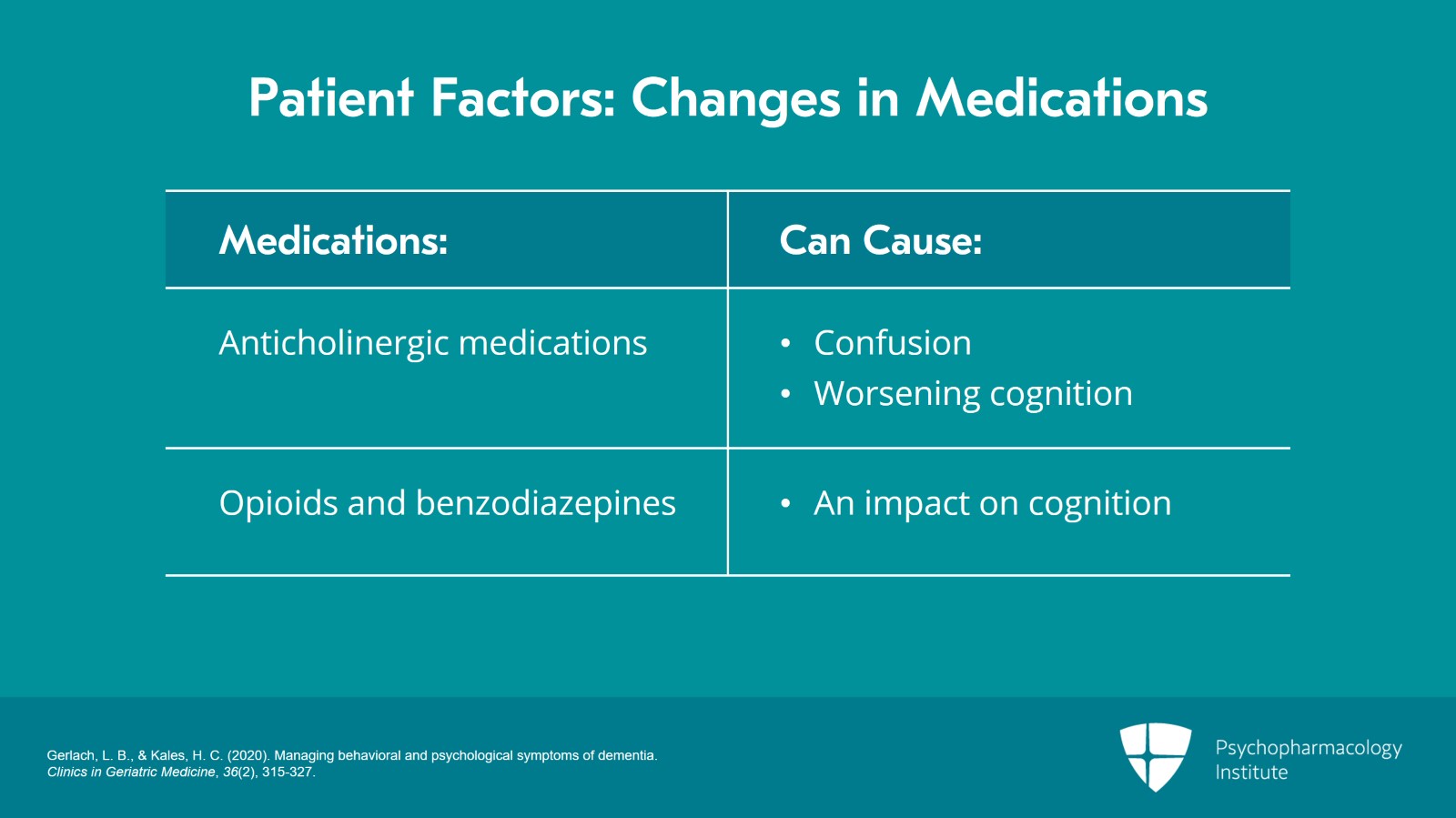
Also, it’s important to think about any recent changes or new medications that have been added.
So anticholinergic medications are notorious for causing confusion or worsening cognition in older adults. So thinking about, has a patient recently been started on diphenhydramine or other highly anticholinergic medications?
Medications like opioids or benzodiazepines can also have impact on cognition which can sometimes lead to some of these behaviors.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 20
And then also thinking about pain.
So as patients with dementia lose the ability to communicate pain, we have to think and look for nonverbal signs of pain or discomfort, so grimacing, guarding.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 6 of 20
There was an interesting study done by researcher Husebo who looked at empirically treating patients with dementia with the British version of acetaminophen.
So, these were the patients with dementia who were not reporting pain and just gave them acetaminophen and found that there were significant reductions in behavioral disturbances in dementia.
So important to assess for and look for nonverbal signs of pain as well.
References:
- Husebo, B. S., Ballard, C., Sandvik, R., Nilsen, O. B., & Aarsland, D. (2011). Efficacy of treating pain to reduce behavioural disturbances in residents of nursing homes with dementia: Cluster randomised clinical trial. BMJ, 343,d4065-d4065.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 20
Other things to think about with the person with dementia is that the person with dementia brings themselves with the diagnosis and meaning that premorbid personality traits, history of psychiatric illness, previous traumas, these things can still persist even as a patient has memory loss and cognitive impairment.
And sometimes, these longstanding patterns can sometimes be worsened or amplified by loss of an ability to have this top-down inhibition.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 8 of 20
It’s also important to remember that behaviors are a form of communication and behaviors can be expressions of unmet needs or goals and those can include physical goals, those can include psychological goals, emotional goals, or social goals.
And as patients with dementia may lose the ability to communicate their needs verbally, we really need to have a trial and error approach to try to learn what these behaviors might be representing. Is the patient thirsty? Are they hungry? Are they having a difficulty with toileting? Are they under-stimulated?
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 20
Next, we think about caregiver factors.
And so as I mentioned before, we know that dementia caregivers as compared to caregivers of other chronic medical conditions have higher levels of stress and lower levels of well-being and physical health compared to other types of caregivers.
We also know that caregivers of patients with dementia also have higher rates of depression and anxiety.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 10 of 20
We know that these types of behavioral disturbances in dementia can often be triggered or exacerbated when a caregiver is stressed or depressed.
And there has been some research to show that negative communication styles can often be a trigger or sometimes amplify these behaviors, so things like anger, screaming, and negative affect.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 20
So if we think back to the case of Frank and Dot, when Dot is stressed, she may communicate with Frank in a way that is kind of angry or frustrated and that can sometimes exacerbate or trigger these behaviors.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 12 of 20
Often, there can also be a mismatch of the expectations of the person with dementia and their dementia stage. And caregivers can often feel that patients are “doing this on purpose” and so it can be very helpful to provide some education to caregivers about the patient’s level of ability, what they can and can’t do, and to help them better understand that and match the activities or things that they’re expecting from the person with dementia to their level and abilities.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 20
So, a colleague of mine talks about this concept of the broken brain. And this can be helpful sometimes in explaining to caregivers that some of these changes that they’re seeing are due to the underlying dementia and are not volitional or being done to frustrate the caregiver. And that can be helpful in discussing with caregivers.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 14 of 20
Next, we think about environmental factors. And the environment really consists of different interacting layers.
So there can be the physical objects, so the items that are in the home. It can include the tasks that compose the activities of daily living. Our environment can also include our social groups as well as our culture and values and beliefs related to care in the home.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 20
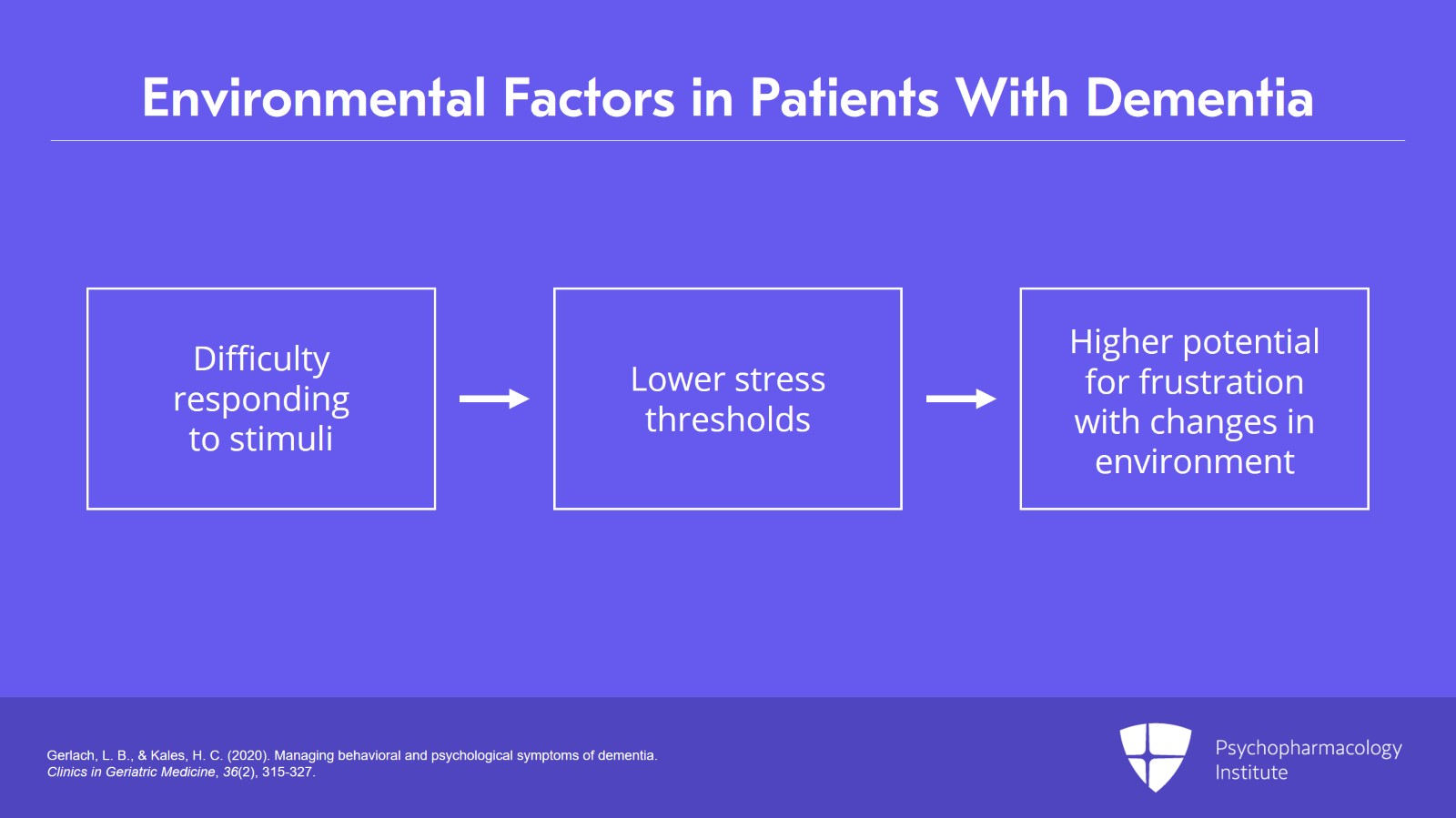
And as we’ve talked about, persons with dementia often have difficulty processing and responding to stimuli in the environment. And so patients can have lower thresholds and a higher potential for levels of frustration especially in places where there are changes in their environment.
And I think a lot of us can think about clinical situations where a patient who has dementia is admitted to the hospital. This is a very disorienting environment for them, and we see an amplification of these behaviors. Or a patient is moved from their home to a nursing facility. Sometimes, you can see an increase in behaviors with this change in environment.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 16 of 20
Lastly, environmental factors can include addressing both over- and under-stimulation in the environment, establishing routines, and optimizing the environment to the capabilities of the person with dementia.
References:
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 20
So our key points.
So patient, caregiver, and environmental factors can all contribute to the development of behavioral and psychological symptoms of dementia.
Person with dementia factors, that can include disruptions in brain circuitry that regulate emotion and that can also include underlying medical issues, amplification of premorbid personality traits, or previous psychiatric history.
Slide 18 of 20
And as patients with dementia lose the ability to communicate their needs verbally, these behaviors can represent unmet needs.
Caregiver factors can include negative communication styles such as anger, irritability, a mismatch of expectations for the person with dementia as well as caregiver burden.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 20
Lastly, environmental factors can include addressing both over- and under-stimulation in the environment, establishing routines, and optimizing the environment to the capabilities of the person with dementia.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.