Slides and Transcript
Slide 1 of 10
Okay. Next, we’ll talk about treatment strategies for postpartum bipolar disorder and psychosis.
Slide 2 of 10
So specifically regarding acute treatment for postpartum psychosis, the appropriate context is generally the inpatient hospitalization setting. It’s important to rule out medical conditions like thyroid or other potential contributing factors. And length of stay generally depends on clinical condition. There have actually been a few studies of the treatment of postpartum psychosis because it is rare and has been difficult to study. But it’s really variable in terms of how quickly women recover from postpartum psychosis. Many women will need to stop breastfeeding either based on treatment that they received with mood stabilizers or because of being on a hospital unit where in general babies are not able to be with the mother. So in many countries, there are mother-baby units. In the US, we have very few mother-baby inpatient hospital units. The primary pharmacotherapy for the treatment of postpartum psychosis is a mood stabilizer and/or an antipsychotic. So many of the newer antipsychotics have been demonstrated to also be important potential treatments as mood stabilizers. And then medications for anxiety, insomnia and agitation are also used as needed.
References:
- Bergink, V., & Kushner, S. A. (2014). Postpartum psychosis. In Psychopharmacology and Pregnancy (pp. 139-149). Springer, Berlin, Heidelberg.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
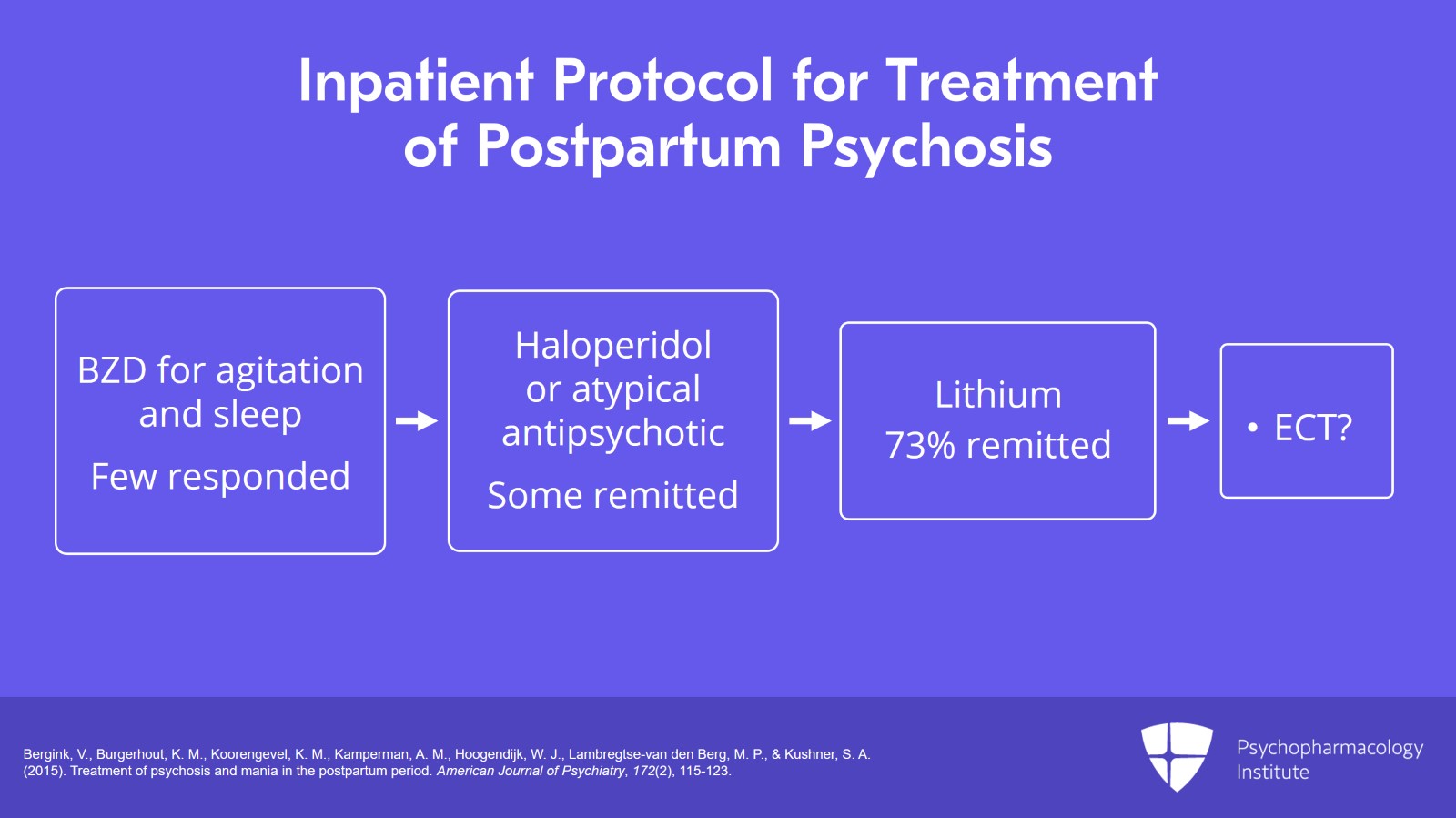
So while there have not been a lot of studies, there was one study by Bergink, et al. from Europe looking at an inpatient protocol for the sequential use of different treatments for postpartum psychosis. What they did for step 1 is provide patients with a benzodiazepine for agitation and sleep and found that very few patients got better with just that. The next step was an antipsychotic medication where a fraction of the patients did remit with just an antipsychotic medication, either haloperidol or an atypical. Step 3 in their algorithm was lithium. And the great majority of women, 73%, remitted while treated with lithium. And it turns out that lithium appears to play a special role in terms of postpartum psychosis which can often present similar to a manic state. But women with postpartum psychosis seem particularly responsive to lithium. So very often, the clinical care will be lithium plus an antipsychotic medication. The investigators also considered ECT in the algorithm although none of their patients in the study got to that step because they generally got better with pharmacotherapy.
References:
- Bergink, V., Burgerhout, K. M., Koorengevel, K. M., Kamperman, A. M., Hoogendijk, W. J., Lambregtse-van den Berg, M. P., & Kushner, S. A. (2015). Treatment of psychosis and mania in the postpartum period. American Journal of Psychiatry, 172(2), 115-123.
Slide 4 of 10
Now, what we don’t really know and don’t have adequate study is about the long-term treatment of postpartum psychosis. So it’s not clear based on the literature how long women should receive pharmacotherapy particularly if they’ve only had a circumscribed episode of postpartum psychosis. So for many women who do experience postpartum psychosis, they experience a postpartum psychosis in the context of having a psychiatric disorder like bipolar disorder. And in that case, the bipolar disorder would be treated as bipolar disorder with ongoing pharmacotherapy. The standard recommendation is that women be continued on medications for six to 12 months after the experience of a postpartum psychotic episode.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
Now, mood stabilizers in breastfeeding is a very important topic. So we talked earlier about antidepressants in breastfeeding. And antidepressants in general as a class are considered compatible with breastfeeding. So with the mood stabilizers, we have a class of medications that include the atypical antipsychotics, lamotrigine, lithium and valproic acid. And as we talked about earlier, valproic acid is associated with a very high risk of birth defects and also neurodevelopmental problems in babies. So we typically avoid valproic acid completely in women of reproductive age, reproductive potential. So we would not consider starting valproic acid in the postpartum. However, many women will receive treatment with lithium in the postpartum. And of all the medications that we use, it is the one known to have the most potential complications during breastfeeding. So there have been case reports of toxicity in babies with high serum blood levels of lithium. And at one point, it was contraindicated by the American Academy of Pediatrics in breastfeeding. So in general, we discourage women from breastfeeding on lithium although occasionally some women do. It’s not something that we recommend. There was one study looking at mom-baby pairs to try and determine under what conditions women who are using lithium could breastfeed in a safe manner. And from that study, it was determined that if babies are going to have careful monitoring including lithium blood levels, monitoring of thyroid hormones and renal labs that it may be reasonable. If mom is doing well on a simple regimen of lithium therapy, it may be reasonable to breastfeed provided the pediatrician is comfortable and the monitoring is in place. So again, we discourage women from breastfeeding while using lithium but occasionally some women would like to do so. And if they are going to do so, then we recommend very careful monitoring of lithium levels in the baby, thyroid function tests, renal tests and make sure that the pediatrician is involved in the plan. Now, with atypical antipsychotics, we typically do not have a lot of information about their use in breastfeeding. They’re not thought to be contraindicated but it’s more of an unknown. If women are on the medication during pregnancy and continuing it, we consider the fact that the baby has already been exposed and the amount of exposure is probably much lower in breastfeeding than it would be during pregnancy. So we don’t discourage women who are on atypicals from breastfeeding. Lamotrigine has also been assessed in mom-baby pairs and appears reasonable for use while breastfeeding.
References:
- Fortinguerra, F., Clavenna, A., & Bonati, M. (2009). Psychotropic drug use during breastfeeding: a review of the evidence. Pediatrics, 124(4), e547-e556.
- Pacchiarotti, I., Leon-Caballero, J., Murru, A., Verdolini, N., Furio, M. A., Pancheri, C., … & Montes, J. M. (2016). Mood stabilizers and antipsychotics during breastfeeding: focus on bipolar disorder. European Neuropsychopharmacology, 26(10), 1562-1578.
Slide 6 of 10
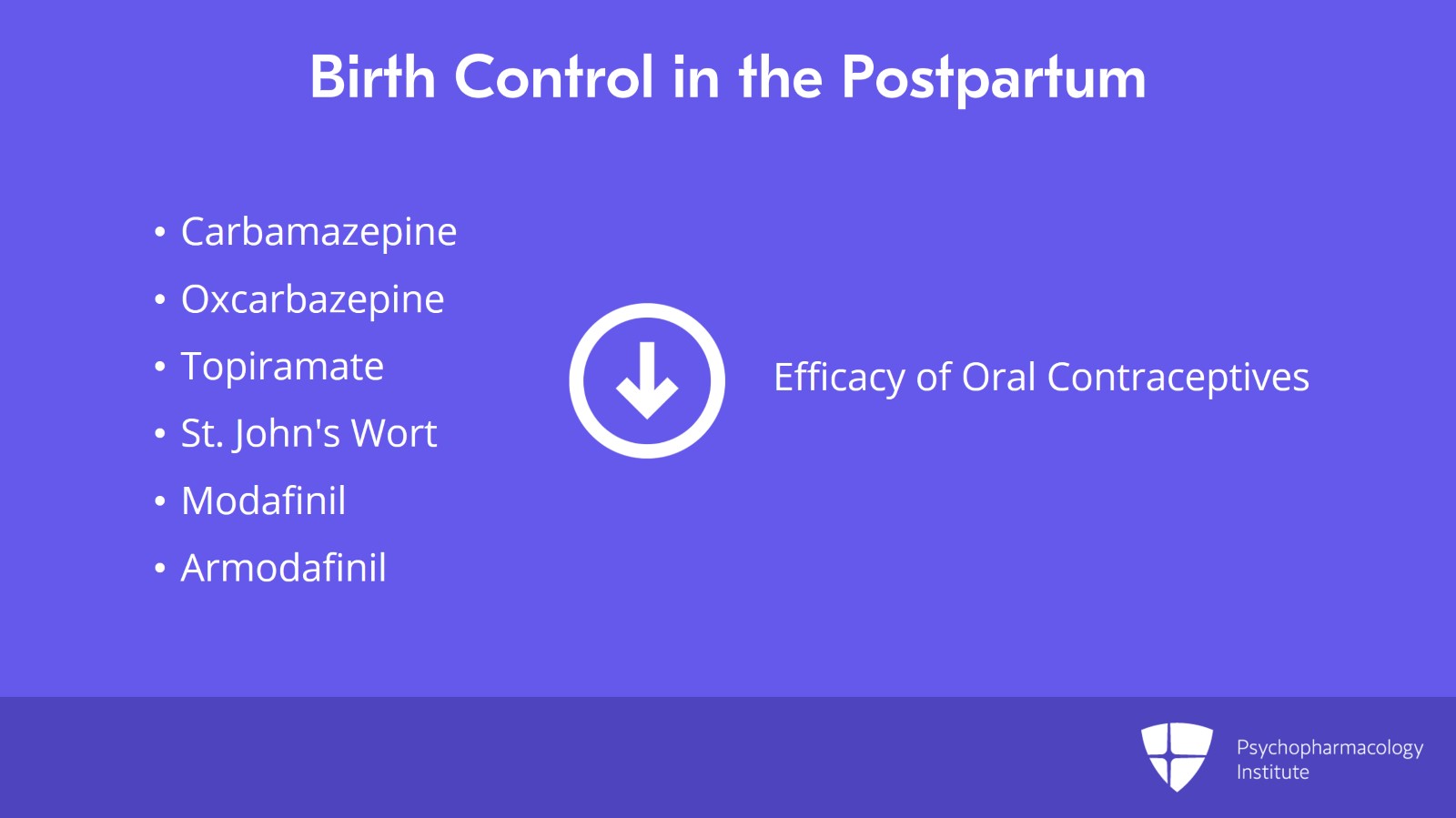
Now, also in the postpartum, we want to think about how to avoid a next pregnancy until it’s wanted. And so we start talking to women about methods of birth control that they’re going to be using, make sure that they’ve thought about that ahead of time. And we also want to consider potential interactions of psychiatric medications with oral contraceptive pills. So some medications used for psychiatric disorders will decrease the efficacy of oral contraceptive pills and those include carbamazepine, oxcarbazepine, topiramate, St. John’s wort, modafinil and armodafinil.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
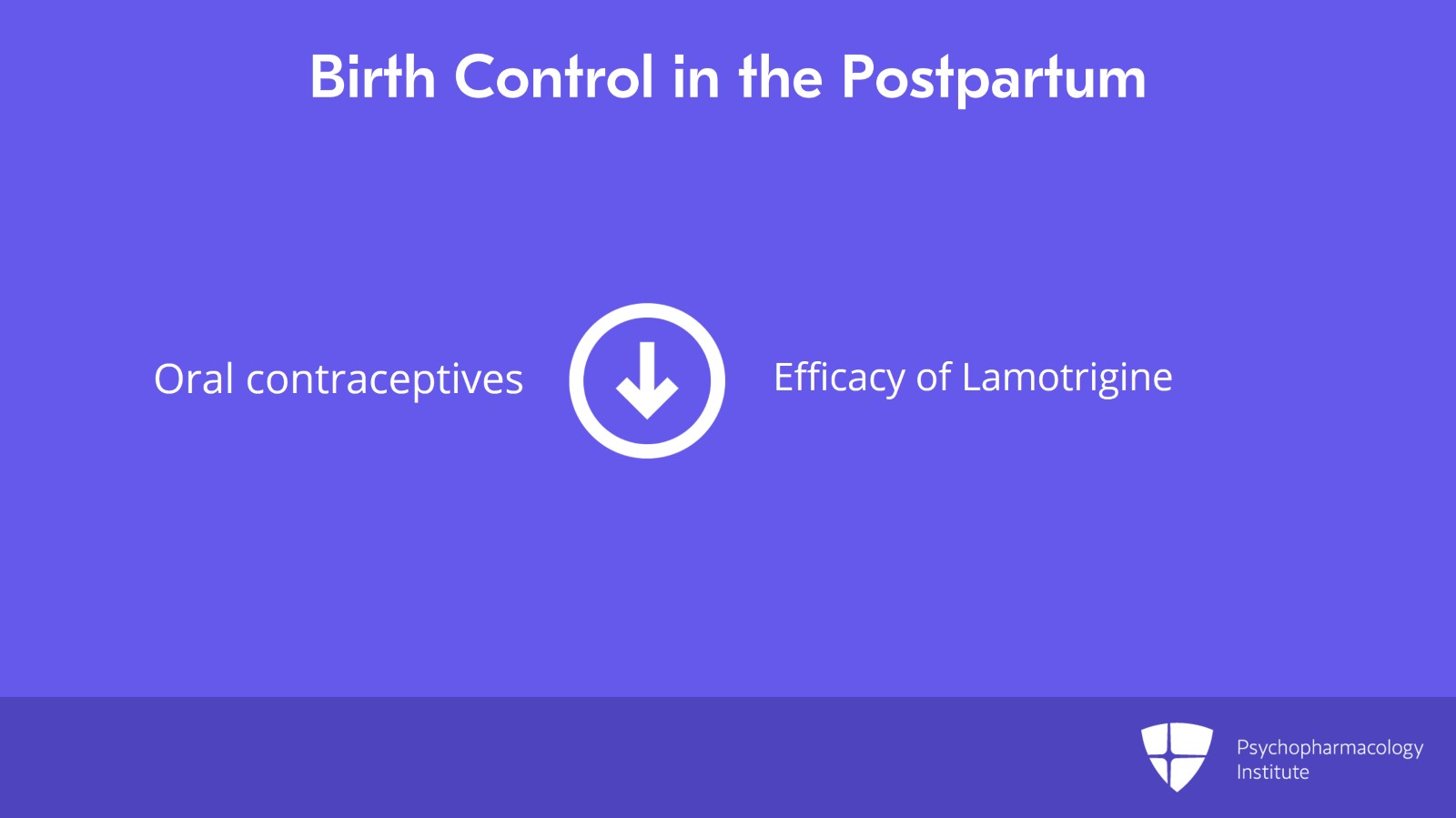
There is a different relationship of interaction between lamotrigine and oral contraceptive pills where starting an oral contraceptive pill can decrease the blood level of lamotrigine. So there may need to be an adjustment in lamotrigine dosing if oral contraceptives are started.
Slide 8 of 10
So key points. Valproic acid is highly teratogenic and associated with longer term neurodevelopmental problems in babies. And because the risk is so high, we discourage its use in women of reproductive potential, so in girls and women of reproductive age. Now, lithium has been associated with an increased risk of cardiovascular defects particularly Ebstein’s anomaly with first trimester exposure, yet the absolute risk is small. So the actual numbers of women affected are small. And so if a woman is particularly responsive to lithium treatment, it may be appropriate for her to continue the medication throughout pregnancy. For women who respond well to lithium and are on it during pregnancy, we generally do not recommend that they breastfeed. So while lithium use during breastfeeding is not recommended, it actually remains one of the few medications where it would warrant this concern.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
And what we also discourage is women switching mood stabilizers in the postpartum. So if a woman is doing well on lithium and has been responsive to it, we do not encourage women to switch to something else specifically for breastfeeding. But we talk to the woman about not breastfeeding so that she can maintain her mental health So while lithium use during breastfeeding is not recommended, it actually remains one of the few medications where it would warrant this concern.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.