Slides and Transcript
Slide 2 of 28
The selection of a particular treatment approach has to be carefully assessed for each individual case taking into account a number of factors—tic symptom severity, the level of functional impairment, severity of comorbid medical and psychiatric conditions, the child's age at presentation.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 28
The duration of illness, adequacy and efficacy of other treatment strategies, tolerability of single or combined treatments.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 4 of 28
And when establishing the treatment hierarchy, one should begin with the most impairing condition and that may not be the tic.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 28
Treatment optimization for tic disorders. If the comorbid disorder has a more significant impact on overall quality of life than the tic symptoms, the treatment of comorbid psychiatric conditions such as ADHD, OCD, anxiety disorders, or mood disorders may in fact take precedence.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 6 of 28
Once baseline characteristics of tic severity and functional impairment have been established, a collaborative approach towards choosing the appropriate treatment modality needs to be undertaken with the patient and family to determine the necessity and intensity of intervention needed.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 28
Remember that many patients with tic disorders don't need any treatment at all. Reassurance is sufficient.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 8 of 28
Behavior therapy treatment optimization. A standard course of behavior therapy is usually between seven to 14 sessions. That being said, the required number of sessions will vary depending on number of bothersome tics and the patient's parents' ability to master and implement the behavioral strategies.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 28
Compliance with out-of-session homework and between-session practice assignments including practicing behavioral strategies, making modifications to school and practicing talking about tics, these are all very important aspects of treatment that can impact therapeutic outcome and should be emphasized to patients and their families early during treatment.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 10 of 28
Pharmacotherapy. Pharmacologic treatment for tic disorders should be considered only when behavioral interventions fail or aren't available, that is a lack of access, you can't find a therapist who's trained in treating tics, patient factors such as cognitions, willingness to participate or when patients exhibit severe violent tics that need treatment.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 28
Before starting treatment with medication, clinicians need to explain the purpose, set a realistic goal to reduce the severity and frequency of tics to the extent that they no longer bother the patient or cause significant problems.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 12 of 28
The selection of a particular pharmacologic treatment for tics requires a cautious analysis of the risks, benefits including consideration of medication side effect profile, potential interactions with concomitant medications, and comorbidity.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 28
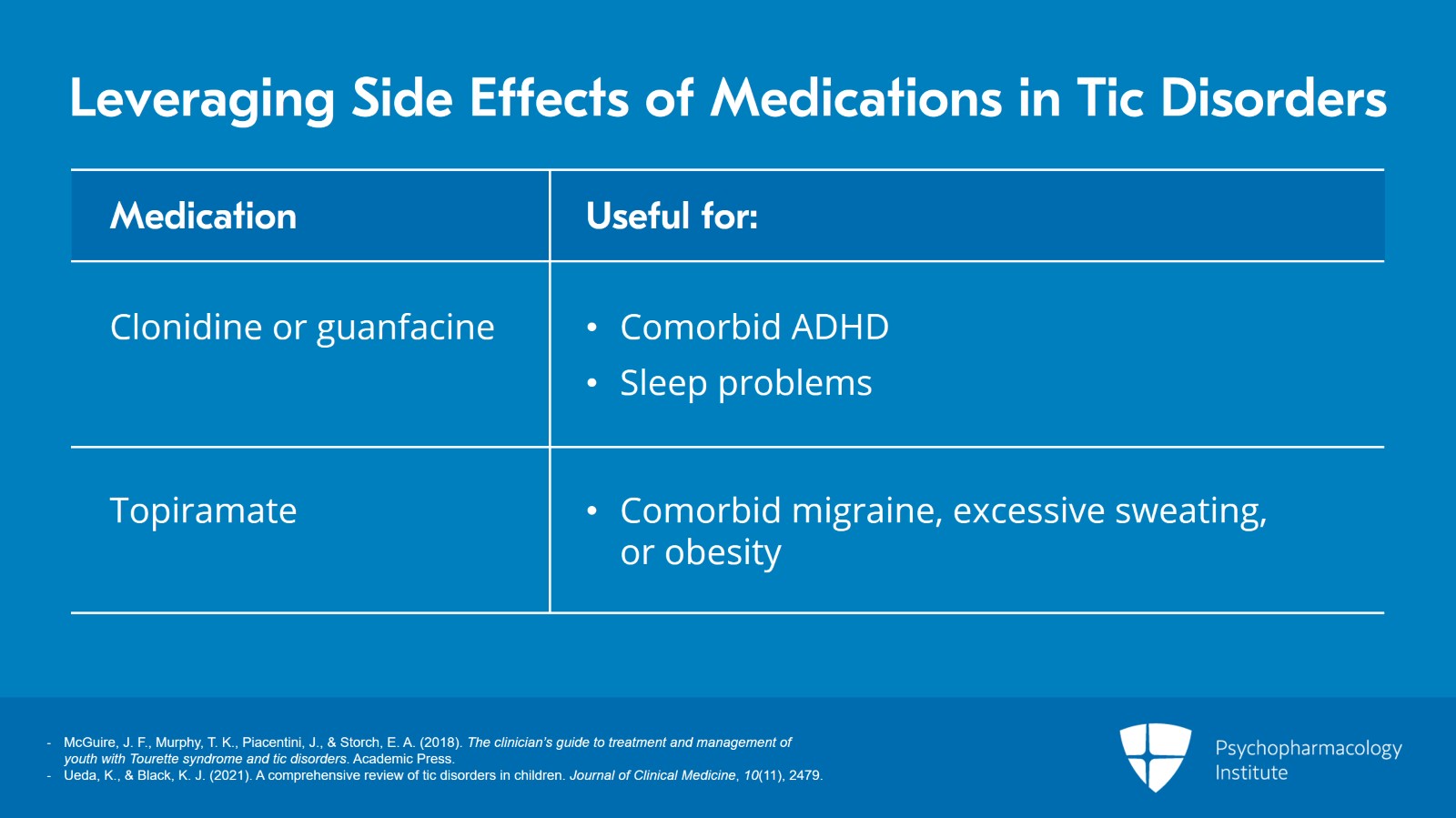
Additional factors have to be considered. Those are cost, the insurance coverage, the ease of administration, leveraging side effects such as sedation or areas where you can treat co-occurring problems.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 14 of 28
Using clonidine or guanfacine for tics with comorbid ADHD. Taking advantage of sedating side effects to administer it nighttime for youth who have trouble falling asleep. Using topiramate for youth with comorbid migraine, excessive sweating, or obesity. These are all critical considerations.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 28
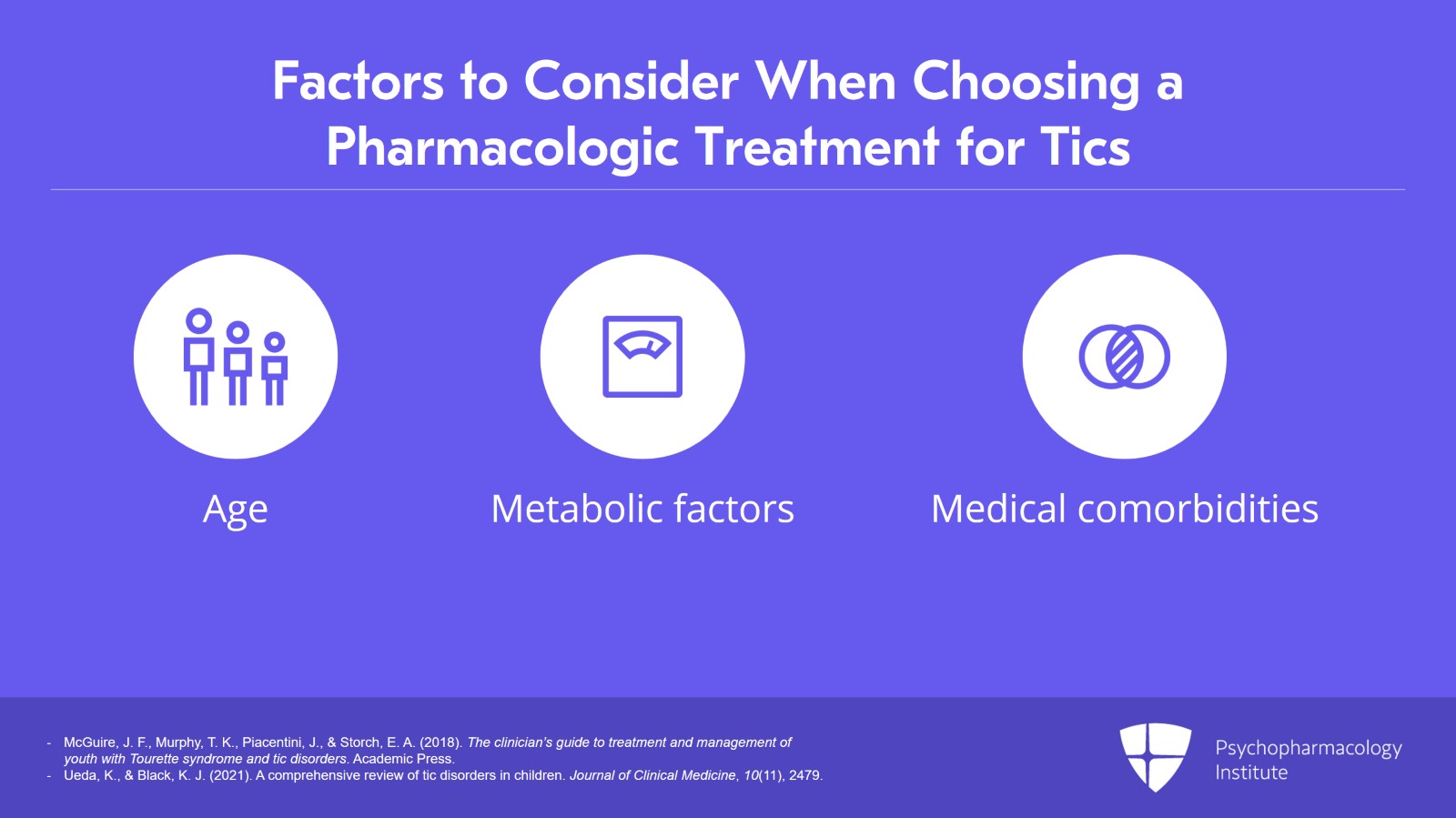
The patient age, weight, metabolic factors and medical comorbidity, liver, kidney or other concurrent medical disease also are critically important.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 16 of 28
Adverse effects often lead to discontinuation of treatment or treatment adherence which can be poor limiting the opportunity to reach optimal dose and response. And here is where the doctor-patient relationship is so critical because if your patient and the family aren't telling you about side effects or concerns and they're not taking the medication regularly that can impact response or lack thereof.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 28
Asking patients about common and rare but serious adverse effects at each follow-up assessment provides an opportunity to monitor the issue.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 18 of 28
And as a rule, medicines are started on a low dose with gradual titration until an effective dose is reached. Adjustments in medication dosing must also take into account the waxing and waning nature of tics so that inadvertent escalation of medication dosage doesn't occur unless truly warranted. Considerable harm happens when a medicine is increased too rapidly because there's concern that there's not enough benefit. All too often, I've seen more good medicines ruined by escalating the dose too rapidly. In children and adolescents, you can't go wrong if you start low, go slow, possibly end up high but give the child or adolescent time to become tolerant to the medicine.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 28
Physicians should discuss weaning patients off medicines once symptoms subside so that tics are no longer disruptive.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 20 of 28
Discontinuing the medicine. There are many guidelines for the management of tic disorders over the short term. The problem is recommendations for long-term medication management are lacking. Current guidance suggests that dose reduction should be considered on an annual basis if tics are stable. And when considering a discontinuation trial, effort should be made to optimize chances of success by pairing the trial with a period with low tic-inducing social environmental factors, minimal life stressors, and regular and adequate amounts of sleep.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 28
Encouraging the patient to focus on the importance of their resilience and their strength rather than on tics being a defining factor of their identity is also incredibly helpful for decreasing the salience of residual and lingering tics. So we're empowering our patient, the children, and of course their parents.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 22 of 28
Treatment resistance. A number of patients respond only partially to treatment and will continue to experience some degree of tic-related impairment and distress.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 28
For those patients who fail to respond to initial treatment, it's critical to conduct a thorough assessment and reassessment, solicit feedback from the youth and their families to identify issues which may be preventing treatment response and determine whether any aspects of treatment should be re-emphasized, revisited. Should the diagnosis be revisited? Are they accurate? Are they complete?
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.23
Slide 24 of 28
Children who are unable to engage with HRT or CBIT can benefit from alternative aspects of behavioral therapy and particularly utilizing function-based assessment and intervention related to triggers and consequences for tics may provide additional therapeutic benefits.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 25 of 28
Clinicians also need to focus on areas that can improve overall quality of life even if they don't directly decrease tic frequency or impact tic severity as well as patient adherence to behavioral intervention and compliance with medicine. You can have the best medicine in the world but if your patient isn't taking the medicine it's not going to help. And similarly with a behavioral intervention, if your patient isn't motivated or the family isn't motivated to do the behavioral interventions, they can't work if they're not attempted.
References:
- McGuire, J. F., Murphy, T. K., Piacentini, J., & Storch, E. A. (2018). The clinician’s guide to treatment and management of youth with Tourette syndrome and tic disorders. Academic Press.
Slide 26 of 28
Key points. Treatment of comorbid psychiatric conditions such as ADHD, OCD, non-OCD anxiety, mood disorders not uncommonly take precedence in treatment of tic disorders, especially if the comorbid disorder has a more significant impact on overall quality of life than the tic symptoms. Adjustments in medication dosing must take the waxing and waning nature of tics into consideration to avoid unnecessary escalation of medication dosage especially if it's not warranted.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 27 of 28
And there are very limited data regarding long-term treatment of tic disorders with current guidelines recommending that dose reduction be considered on an annual basis if the tics are stable.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.