Slides and Transcript
Slide 2 of 9
…it's important to include consideration of psychotherapy as part of the treatment plan because many of these women experience issues related to aging, to illness and of course to interpersonal difficulties. So psychotherapy should certainly be part of the armamentarium for the treatment of women with perimenopausal depression.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 9
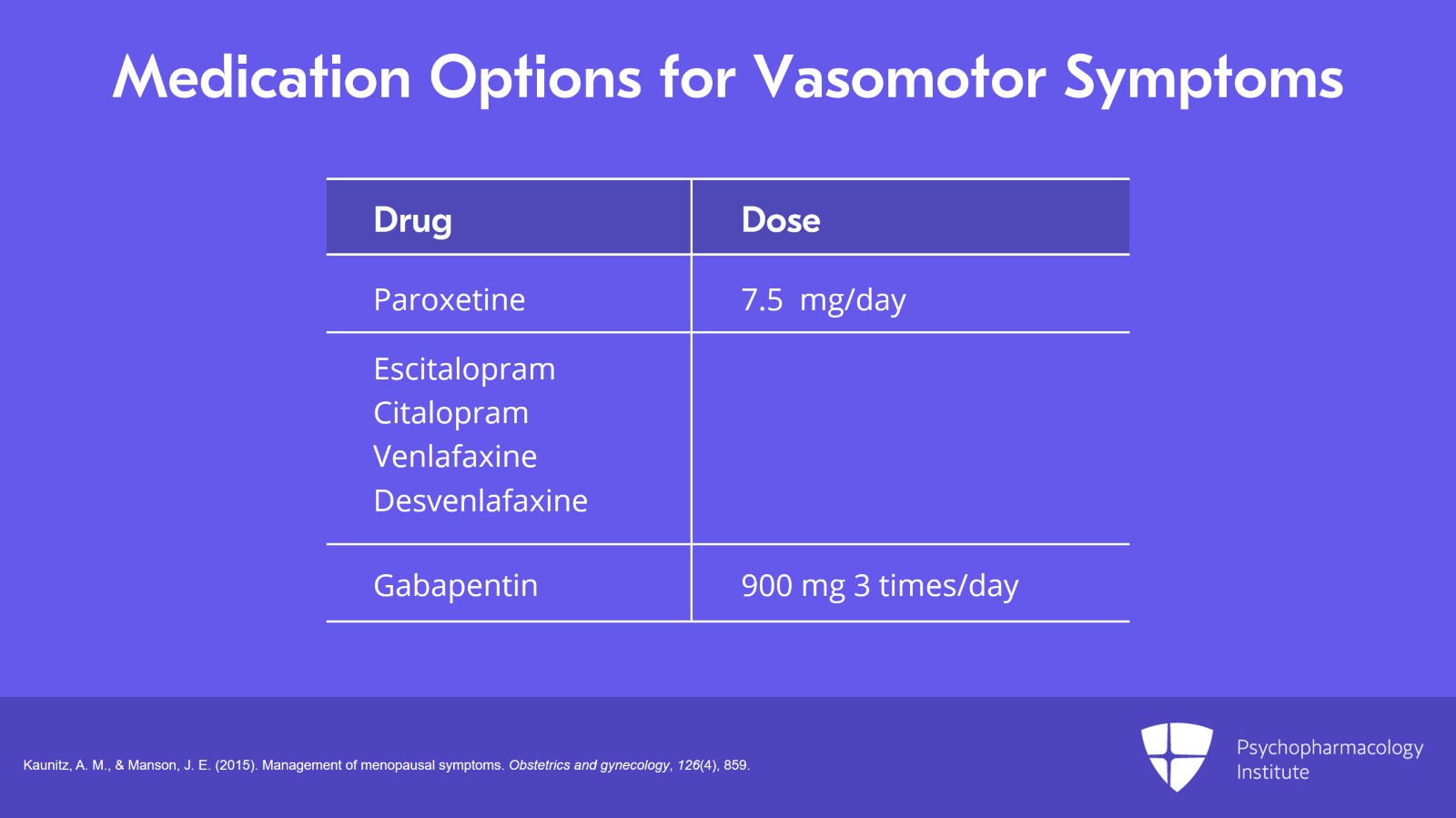
Moving on, when choosing among medication options for perimenopausal depressed women with vasomotor symptoms, a number of medications have been shown to reduce the frequency of vasomotor symptoms. Paroxetine is the only FDA-approved antidepressant at a low dose of 7.5 mg per day to treat perimenopausal vasomotor symptoms. Escitalopram, citalopram, venlafaxine, desvenlafaxine have also been shown to improve symptoms of perimenopause. And gabapentin 900 mg 3 times a day can also reduce the frequency of vasomotor symptoms in perimenopausal women.
References:
- Kaunitz, A. M., & Manson, J. E. (2015). Management of menopausal symptoms. Obstetrics and gynecology, 126(4), 859.
Slide 4 of 9
Clinical experience suggests that the choice of treatment ought to be based on first of all prior history of response to an antidepressant in those cases of women with a history of depression and possible response to either an SSRI or an SNRI. And also, choice of treatment should be based on the side effect profile of the available options.
References:
- Robakis, T., Williams, K. E., Nutkiewicz, L., & Rasgon, N. L. (2019). Hormonal contraceptives and mood: review of the literature and implications for future research. Current psychiatry reports, 21(7), 57.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 9
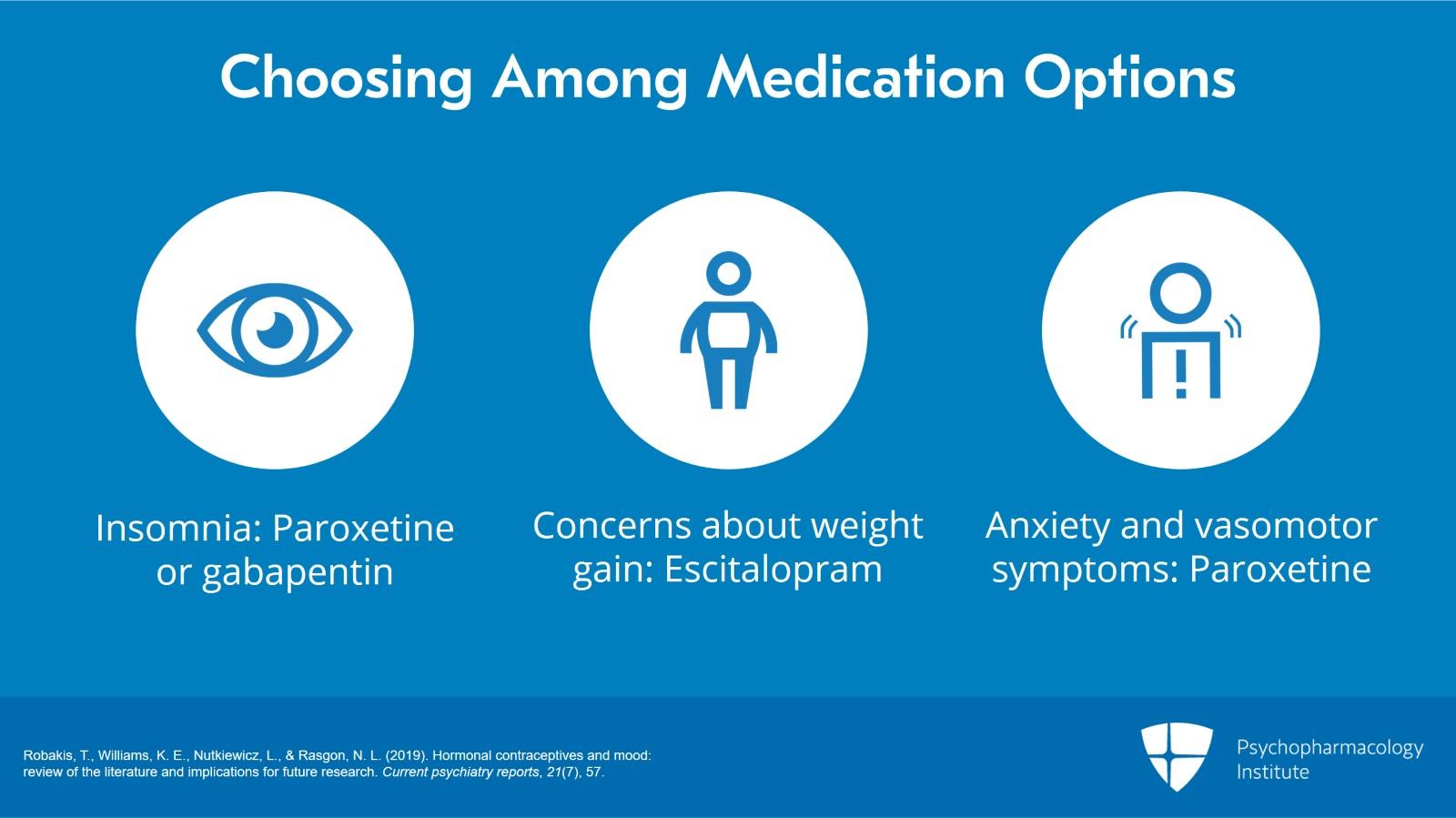
For women with insomnia, one might move towards paroxetine or gabapentin. For women with concerns about weight gain, escitalopram might be preferred. For women with anxiety associated with vasomotor symptoms, paroxetine might also be a good choice.
References:
- Robakis, T., Williams, K. E., Nutkiewicz, L., & Rasgon, N. L. (2019). Hormonal contraceptives and mood: review of the literature and implications for future research. Current psychiatry reports, 21(7), 57.
Slide 6 of 9
Moving on, one of the questions that often comes up when thinking about treatment options for perimenopausal women is what is the role of estrogen? Well, for now, antidepressants are of course still the treatment of choice for these women. When selecting which antidepressant, of course, it's best to choose a medication that treats depression and other accompanying symptoms like anxiety and somatic or pain symptoms. Still, there is emerging data regarding the use of estrogen to treat depression and I'd like to review that data with you in the next few slides.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 9
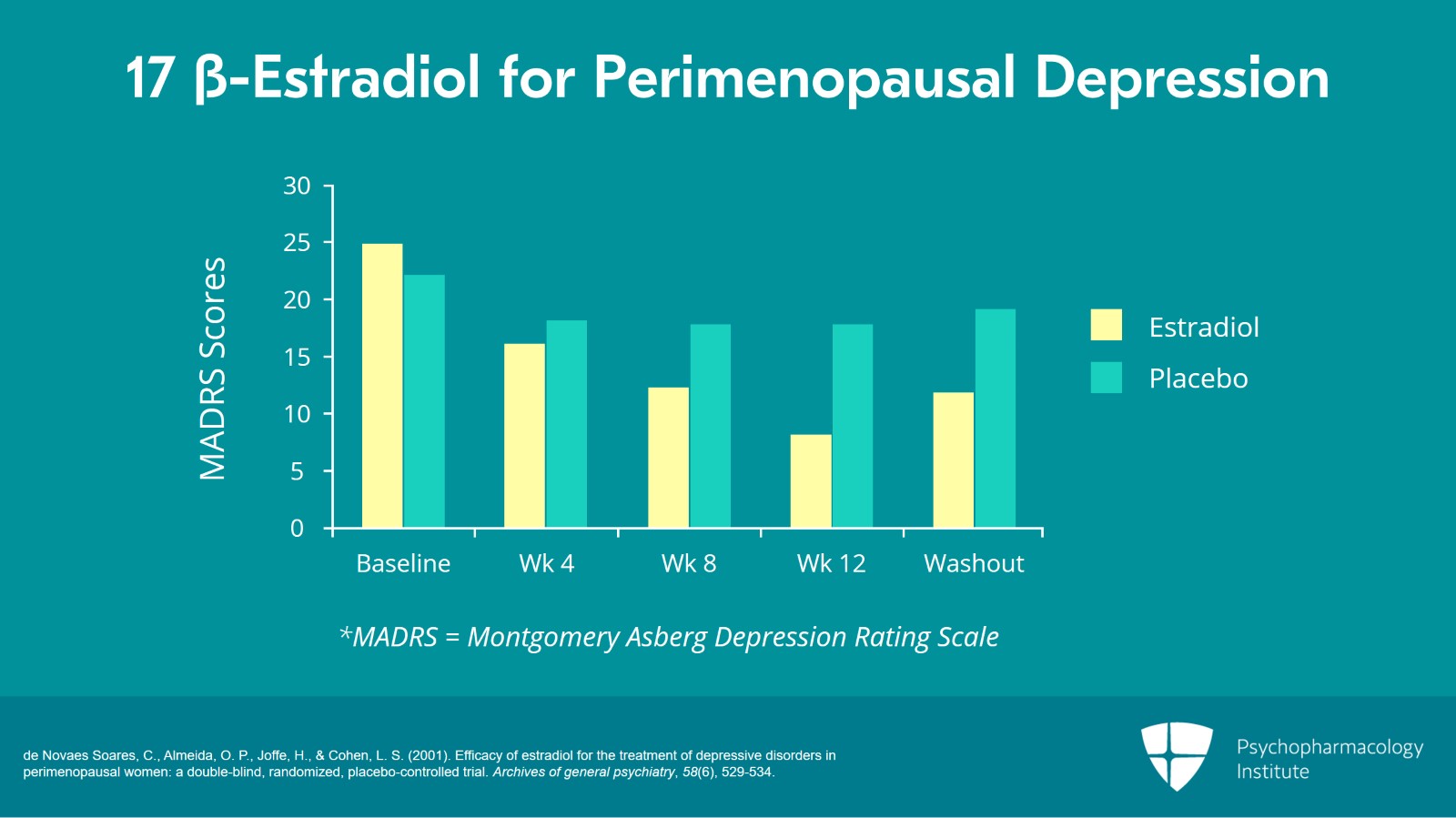
Looking at this first early preliminary studies, Suarez and his coworkers followed 50 perimenopausal women. Half of them had depressive symptoms. Some of them had major depression. Others had depressive symptoms that did not quite meet criteria for major depression. This study had two phases. The first phase was a 12-week component that involved treatment of half of the subjects with an estrogen patch while the other half were treated with a placebo patch. The second phase was a four-week washout where neither group was treated with estradiol. As you can see from the data presented in this slide looking at this graph, over the course of the 12 weeks of treatment, the women on active drug, the estrogen- or estradiol-treated women, had improved depression scores as measured by the MADRS. What is also interesting is that even after a four-week washout, those women who had been treated with estradiol in the first 12 weeks but were no longer being treated with estradiol were still less depressed than the control group. So there was some sort of a continued effect even after treatment was stopped.
References:
- de Novaes Soares, C., Almeida, O. P., Joffe, H., & Cohen, L. S. (2001). Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women: a double-blind, randomized, placebo-controlled trial. Archives of general psychiatry, 58(6), 529-534.
Slide 8 of 9
So what are our takeaway key points at this part of our presentation? First of all, at this time, antidepressants are the treatment of choice for perimenopausal women with major depression. Secondly, for women not meeting criteria for major depression, hormonal treatments may be considered to address underlying menopausal symptoms like hot flashes, insomnia, sexual disturbances and other related symptoms. All of which may be responsible for secondary depression.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.