Slides and Transcript
Slide 2 of 28
- Adler, N. E., & Page, A. E. K. (2008). Committee on psychosocial services to cancer patients/families in a community setting. In Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs.
Download PDF and other files
Slide 3 of 28
In addition to these therapeutic modalities, there will be a subset of patients that can benefit from an antidepressant, usually patients who have depression at a moderate to severe level. We want to educate patients that antidepressants are not addicting. That's one of the most common fears that patients have and one of the most common barriers to them accepting the treatment.
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 4 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
Slide 5 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 6 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
Slide 7 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 8 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
Slide 9 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
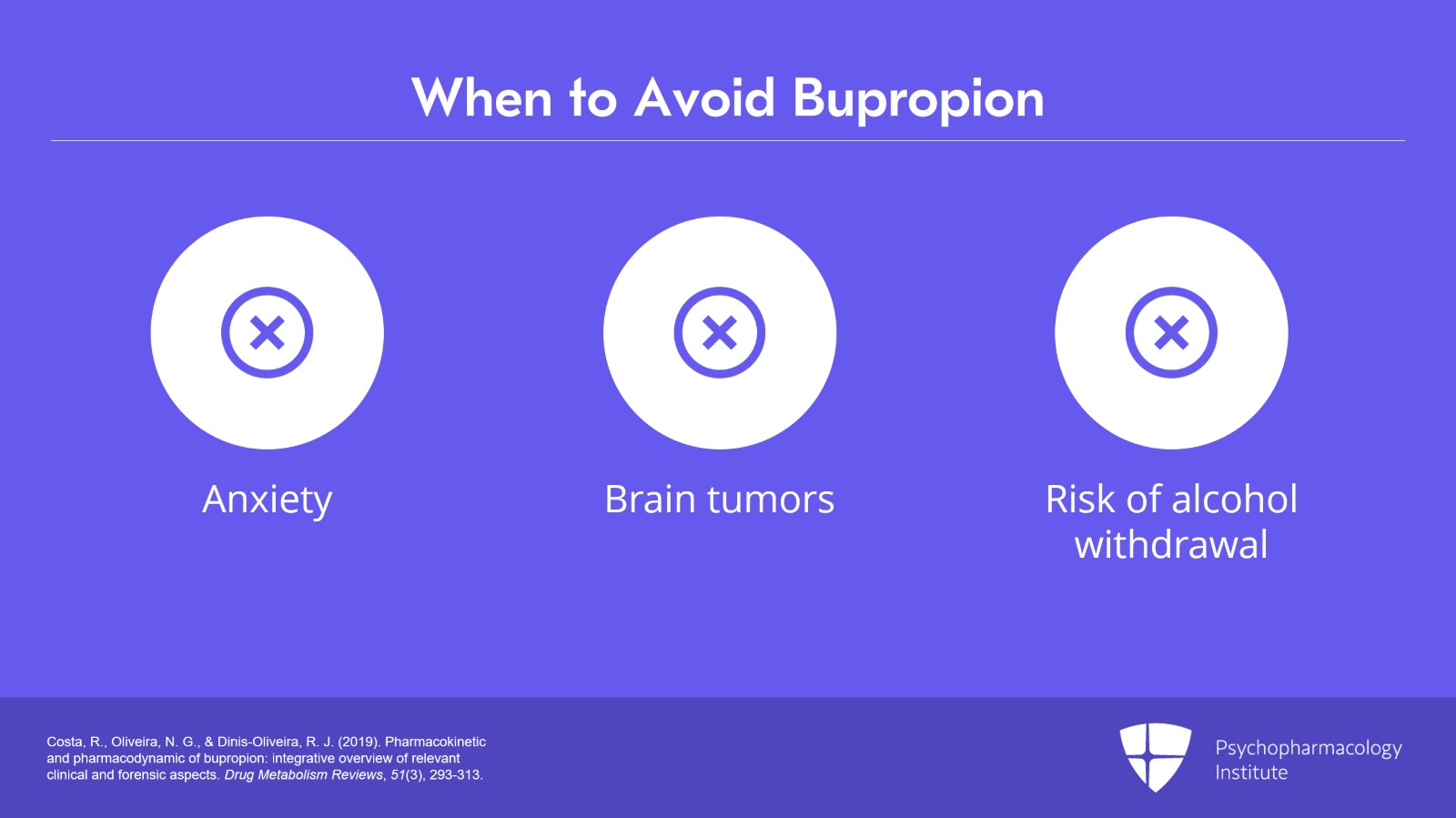
Slide 10 of 28
- Costa, R., Oliveira, N. G., & Dinis-Oliveira, R. J. (2019). Pharmacokinetic and pharmacodynamic of bupropion: integrative overview of relevant clinical and forensic aspects. Drug Metabolism Reviews, 51(3), 293-313.
Download PDF and other files
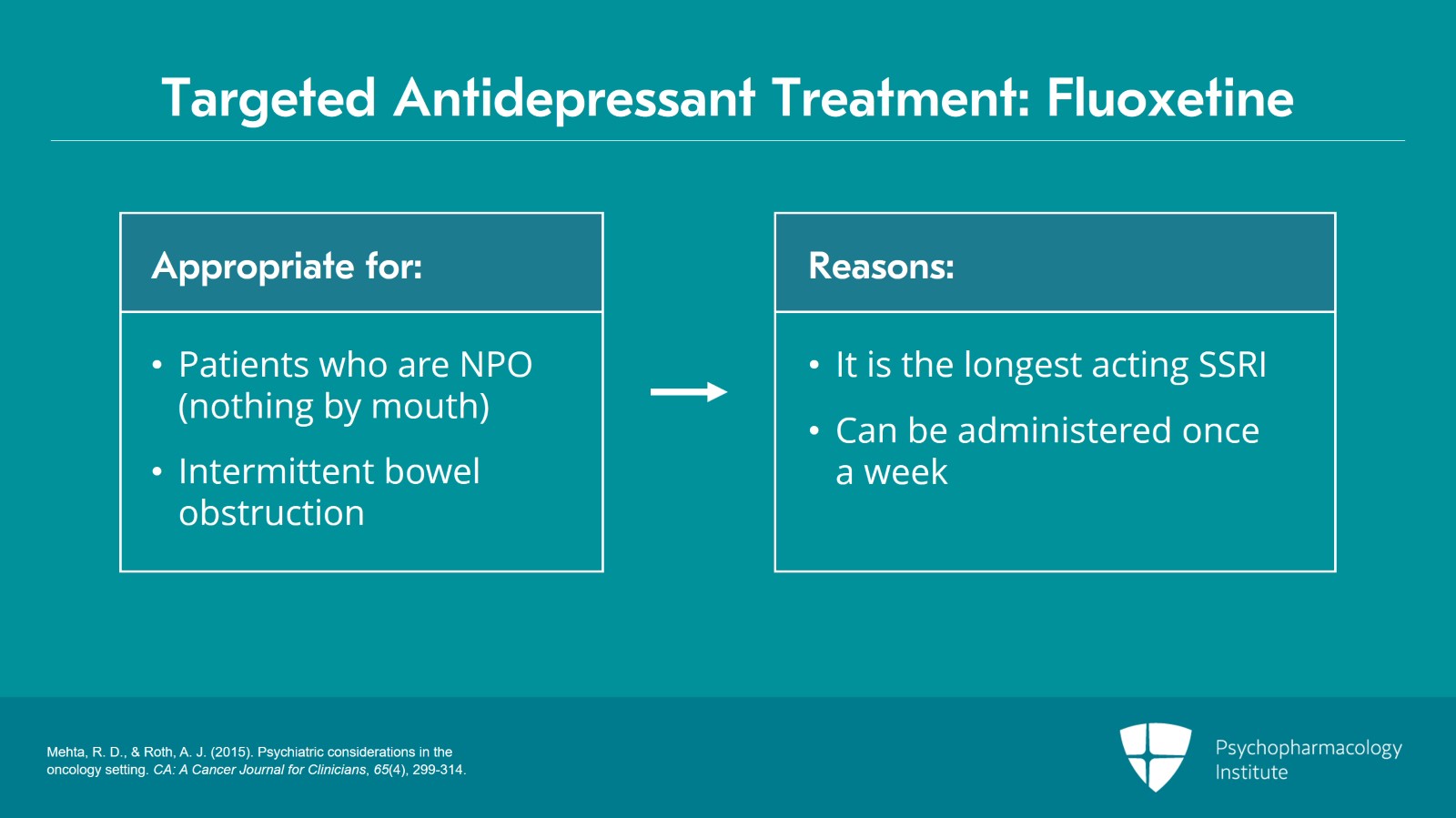
Slide 11 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
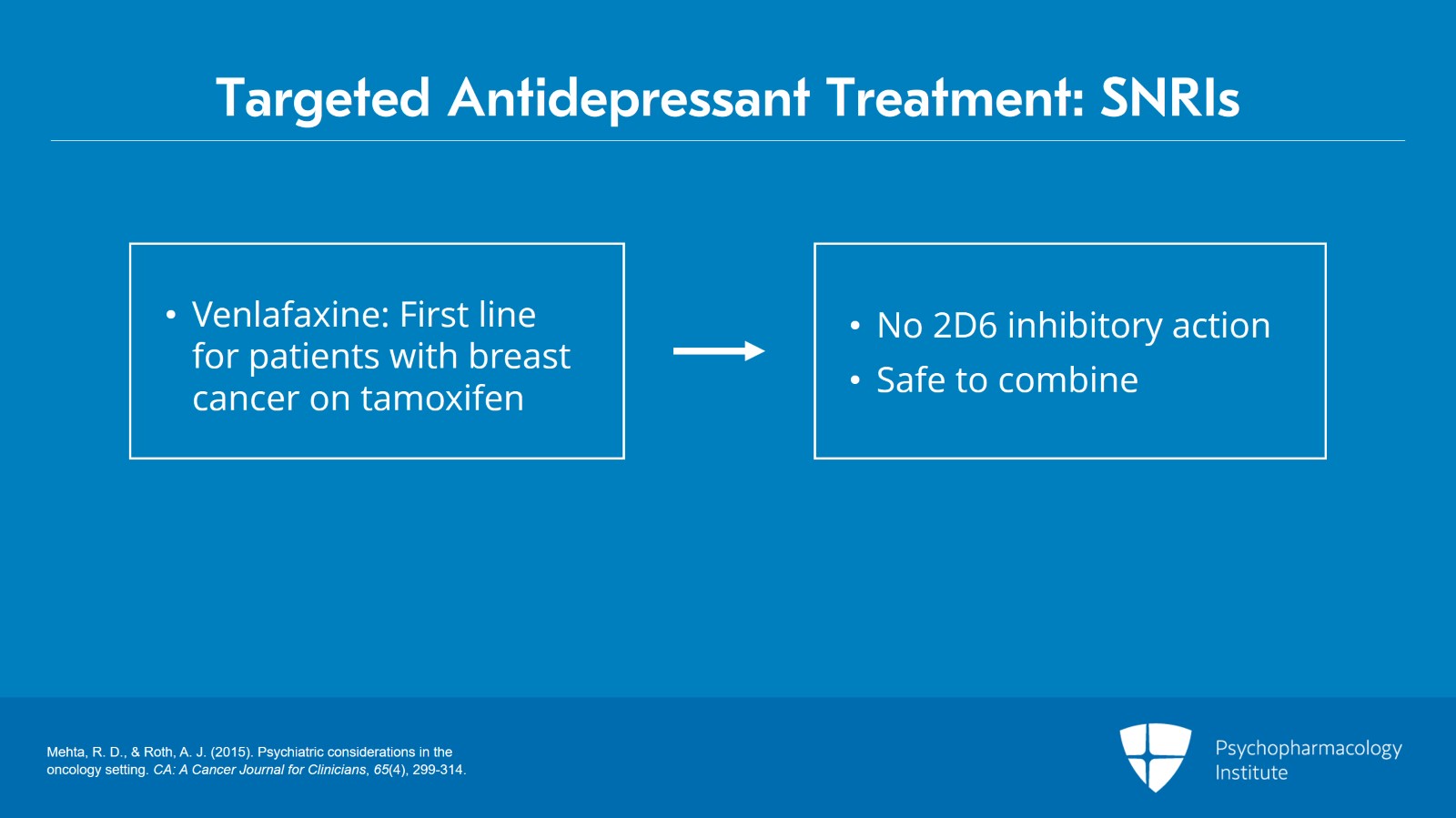
Slide 12 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
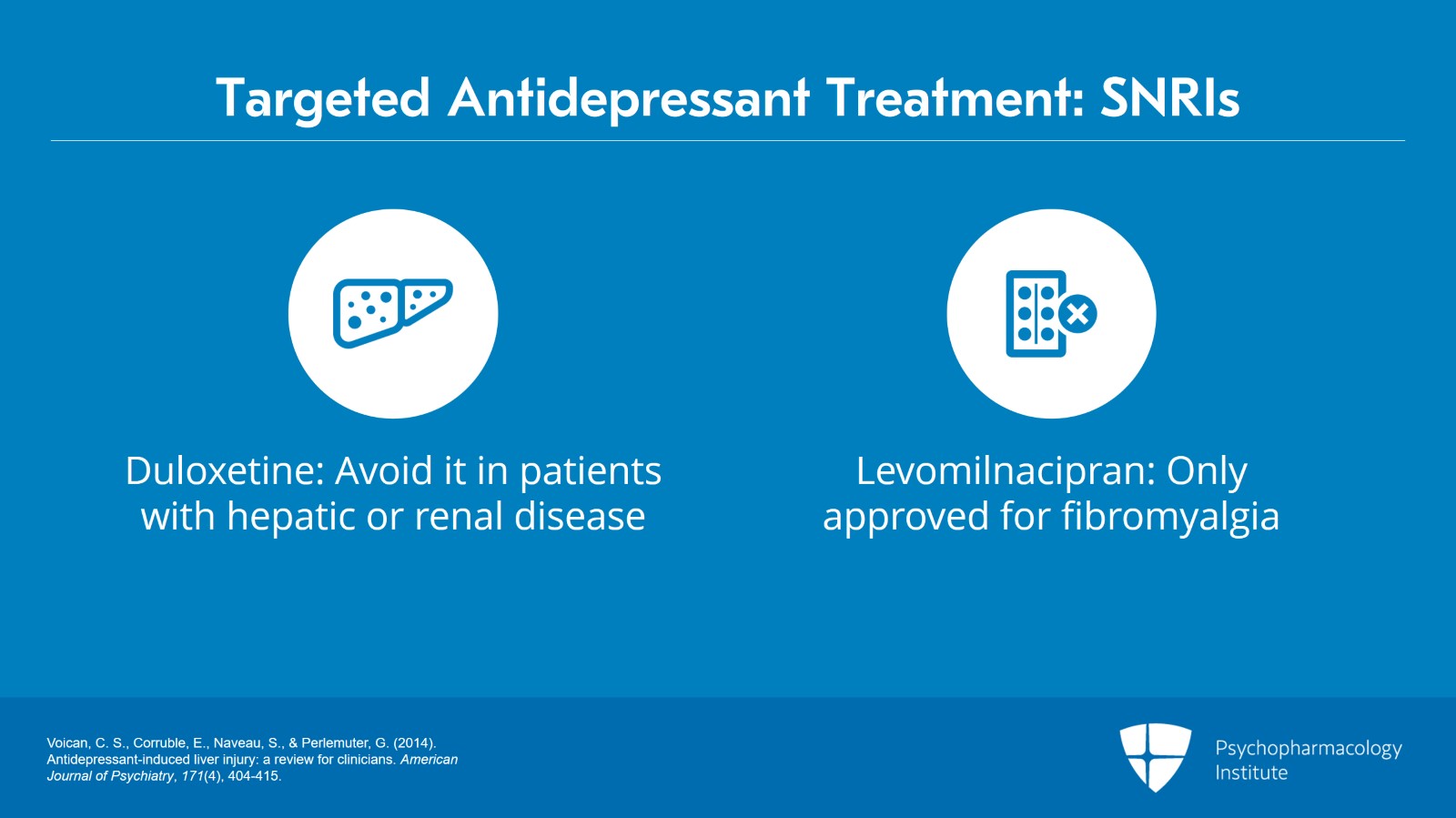
Slide 13 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 14 of 28
- Voican, C. S., Corruble, E., Naveau, S., & Perlemuter, G. (2014). Antidepressant-induced liver injury: a review for clinicians. American Journal of Psychiatry, 171(4), 404-415.
Download PDF and other files
Slide 15 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 16 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
Slide 17 of 28
- Kasper, S., Praschak-Rieder, N., Tauscher, J., & Wolf, R. (1997). A risk-benefit assessment of mirtazapine in the treatment of depression. Drug Safety, 17, 251-264.
Slide 18 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
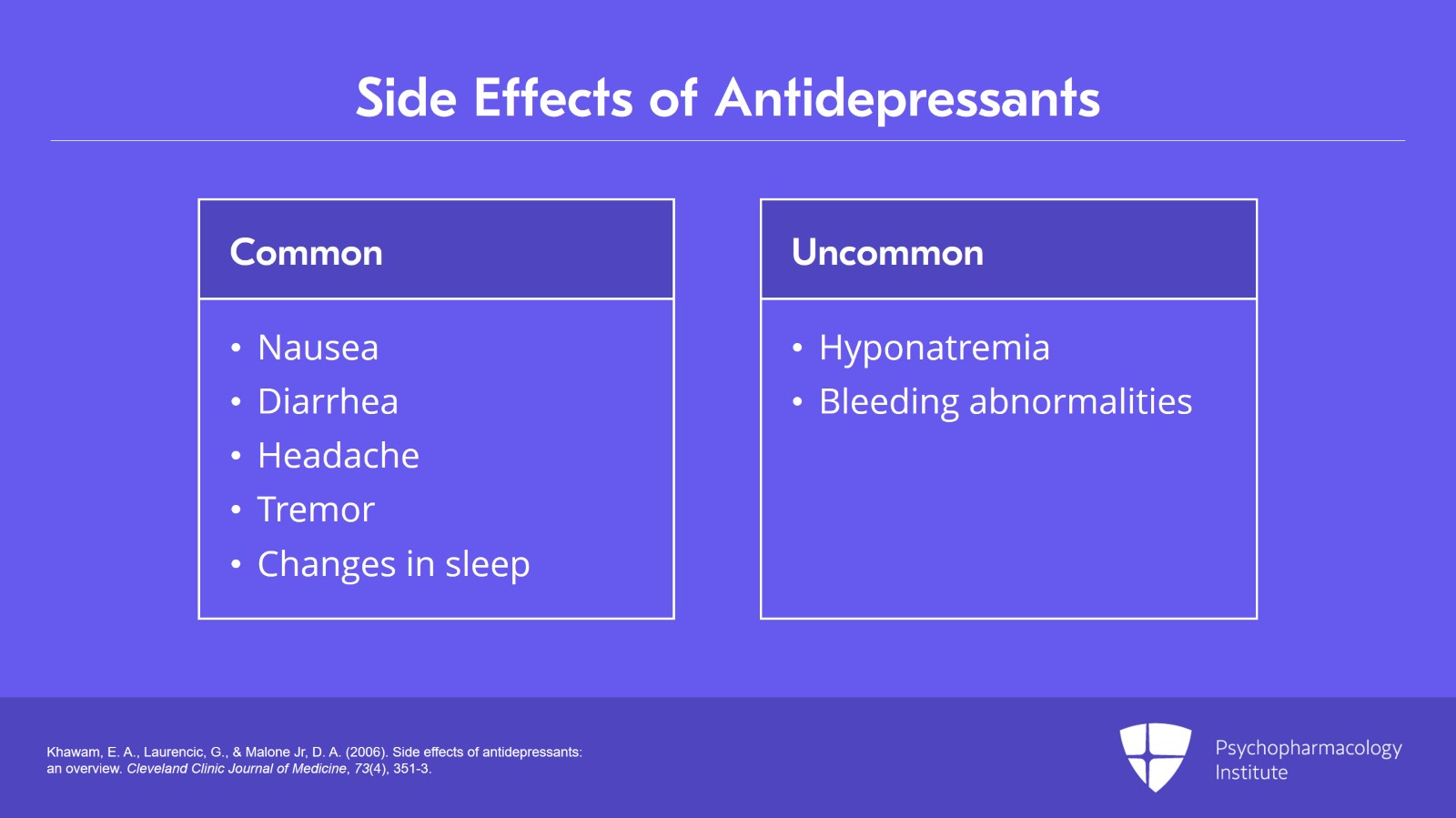
Slide 19 of 28
- Khawam, E. A., Laurencic, G., & Malone Jr, D. A. (2006). Side effects of antidepressants: an overview. Cleveland Clinic Journal of Medicine, 73(4), 351-3.
Slide 20 of 28
- Shelton, R. C. (2019). Serotonin and norepinephrine reuptake inhibitors. Antidepressants: From Biogenic Amines to New Mechanisms of Action, 145-180.
Download PDF and other files
Slide 21 of 28
- Zarowitz, B. J. (2007). Antidepressant tapering: avoiding adverse consequences of gradual dose reduction. Geriatric Nursing, 2(28), 75-79.
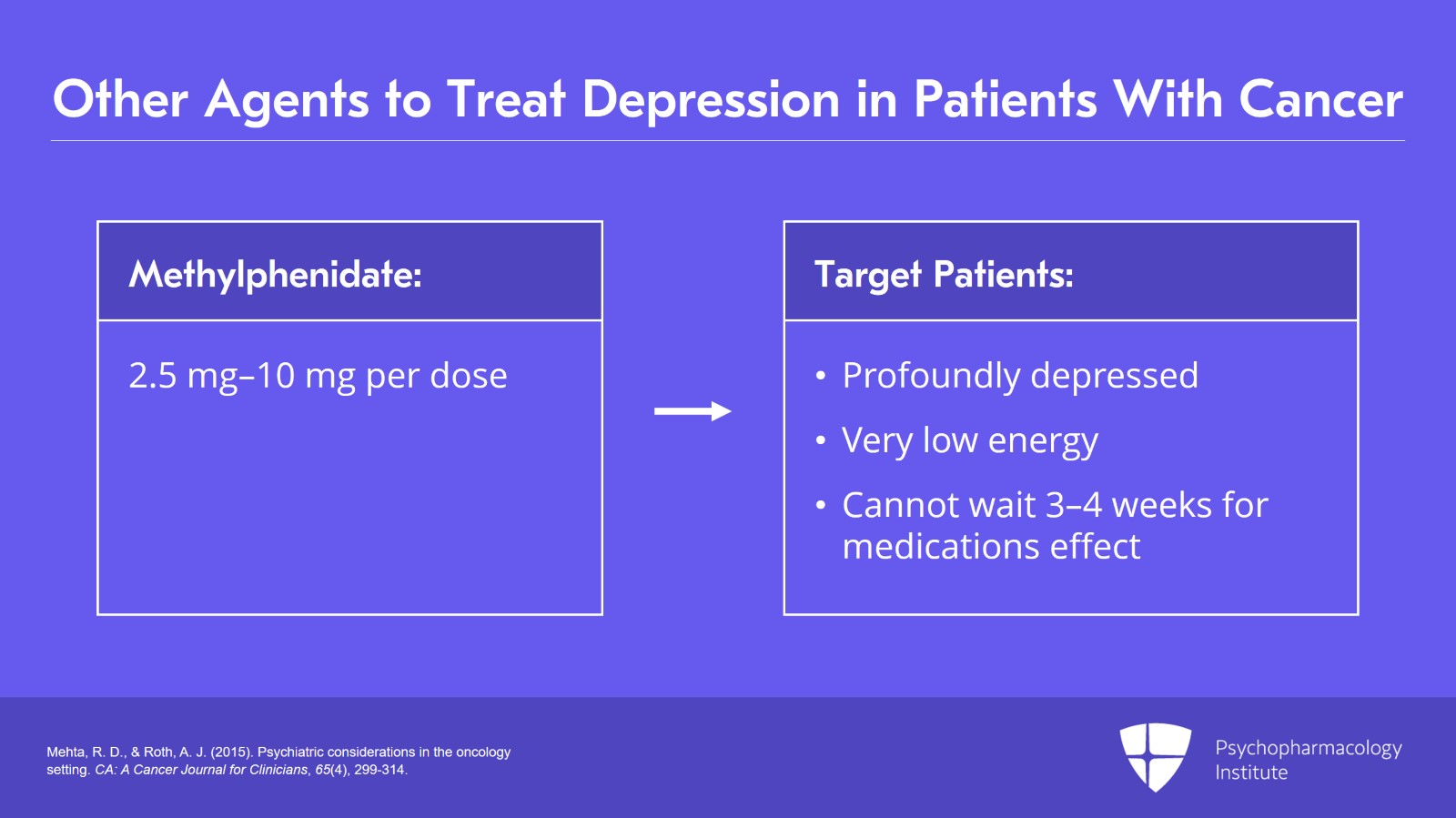
Slide 22 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
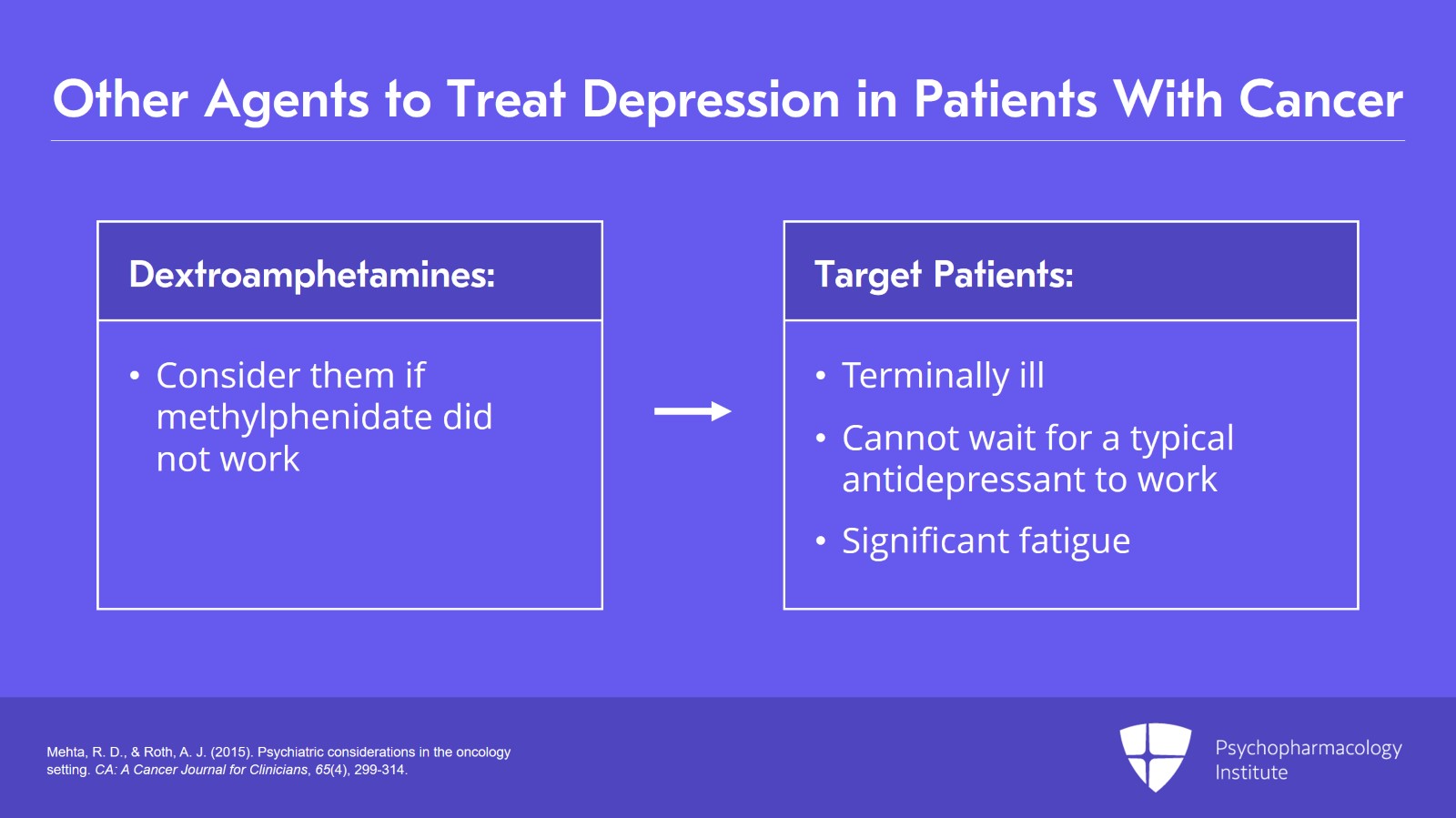
Slide 23 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 24 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Download PDF and other files
Slide 25 of 28
- Mehta, R. D., & Roth, A. J. (2015). Psychiatric considerations in the oncology setting. CA: A Cancer Journal for Clinicians, 65(4), 299-314.
Slide 26 of 28
Download PDF and other files
Slide 27 of 28
Download PDF and other files