Slides and Transcript
Slide 1 of 25
Hello, everyone. I'm David Mintz. I'm the Director of Psychiatric Education, a team leader at the Austen Riggs Center which is a tertiary care center for the treatment of patients with treatment-resistant psychiatric conditions. It's also a psychoanalytic hospital, or psychodynamic hospital, so the dynamics of patients are considered to be an important aspect of care. I'm also the former leader of the Psychotherapy Caucus of the American Psychiatric Association and so psychotherapy is an important part of the ways that I think about doing pharmacotherapy. So at this point, I think we're going to switch gears just a little bit and I think we've been talking more clinical what you do when you're sitting with a patient and we're just going to step back to the level of the evidence base behind a lot of what I've been talking about over the last videos.
Slide 2 of 25
And so we're going to start focusing on the science of the art of Psychopharmacotherapy.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 25
And it is probably important to say and it's been implied in everything I've said so far that medication outcomes, we know, are influenced by a range of psychosocial factors. This includes prescriber effects, characteristics of the pill, setting of administration which is why the gold standard of medication trials would be a multicenter placebo-controlled trial because I think we, we learned already in the 1950s and '60s that you could get fantastic results at one research site and nonsignificant results at another based on the patient population, the setting, the people. Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Slide 4 of 25
I would say nonclinical patient characteristics also influence how medications work and by nonclinical patient characteristics I mean not necessarily characteristics of the illness but things about the patient, their psychology, their coping, their psychosocial factors in which they're embedded, all of that and of course the therapeutic alliance.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 25
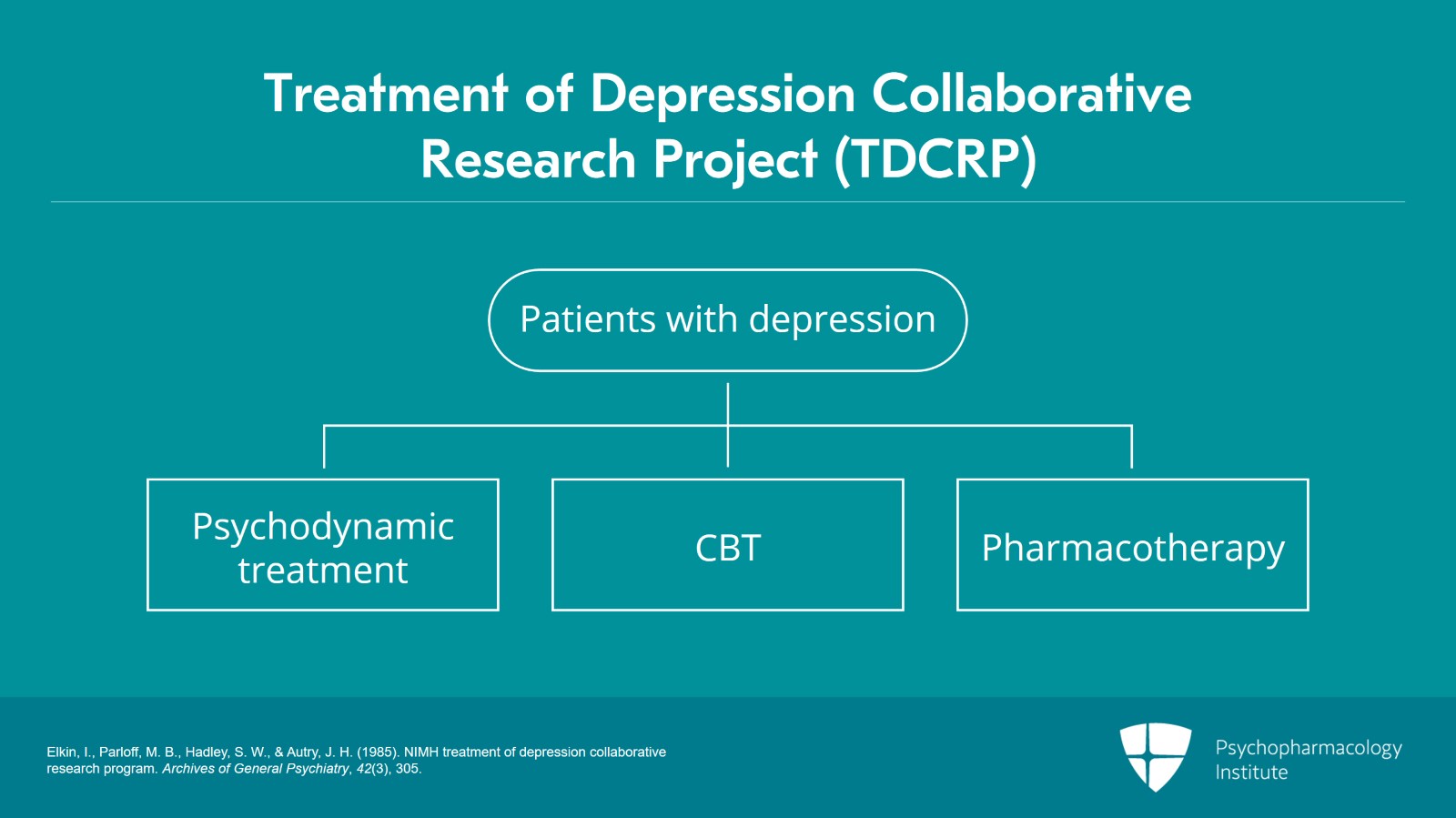
So for starters, I just want to highlight a study that I think cast this in a very clear light which is a secondary analysis of the TDCRP data. The TDCRP, the Treatment of Depression Collaborative Research Project was before STAR*D, the largest NIMH-funded, multicenter, placebo-controlled trial that had been done looking at treatments for depression. And in that study, they were comparing psychodynamic treatments or IPT, cognitive behavioral treatments and then pharmacotherapy.
References:
- Elkin, I., Parloff, M. B., Hadley, S. W., & Autry, J. H. (1985). NIMH treatment of depression collaborative research program. Archives of General Psychiatry, 42(3), 305.
Slide 6 of 25
And the basic results of that study were they were all about equally effective and the combinations of medications and psychotherapy were perhaps a little bit more effective.
References:
- Elkin, I., Parloff, M. B., Hadley, S. W., & Autry, J. H. (1985). NIMH treatment of depression collaborative research program. Archives of General Psychiatry, 42(3), 305.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 25
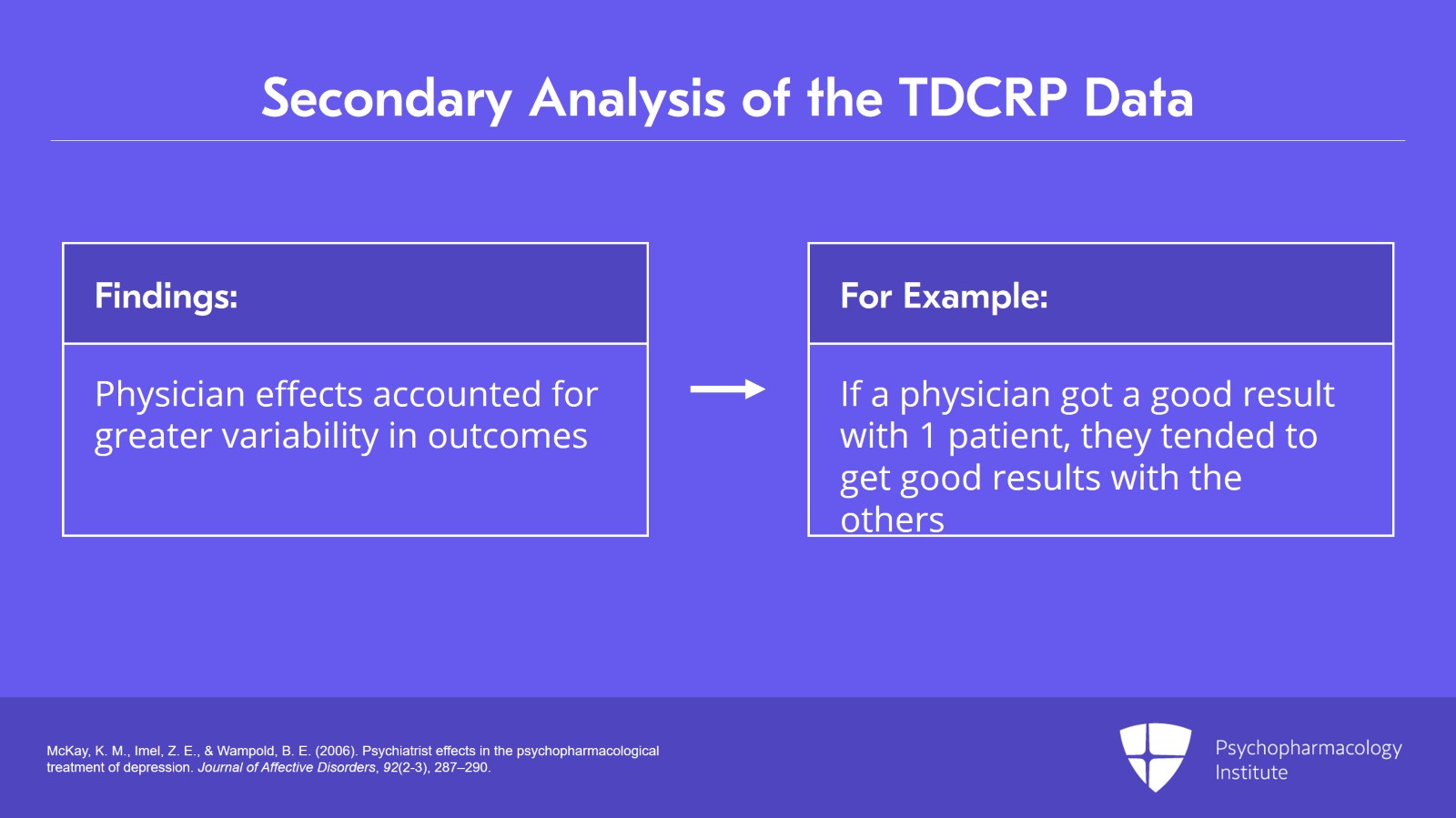
But McKay, Imel and Wampold in 2006 went back and did a secondary analysis of that data looking through the lens of the prescriber. And what they found interestingly was that physician effects accounted for greater variability in outcomes than did the medication condition itself. And so it turned out, for example, that if a physician got a good result with one patient, they tended to get good results with all the patients. And if a physician got poor results with a patient, they tended to get poor results with all the patients.
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
Slide 8 of 25
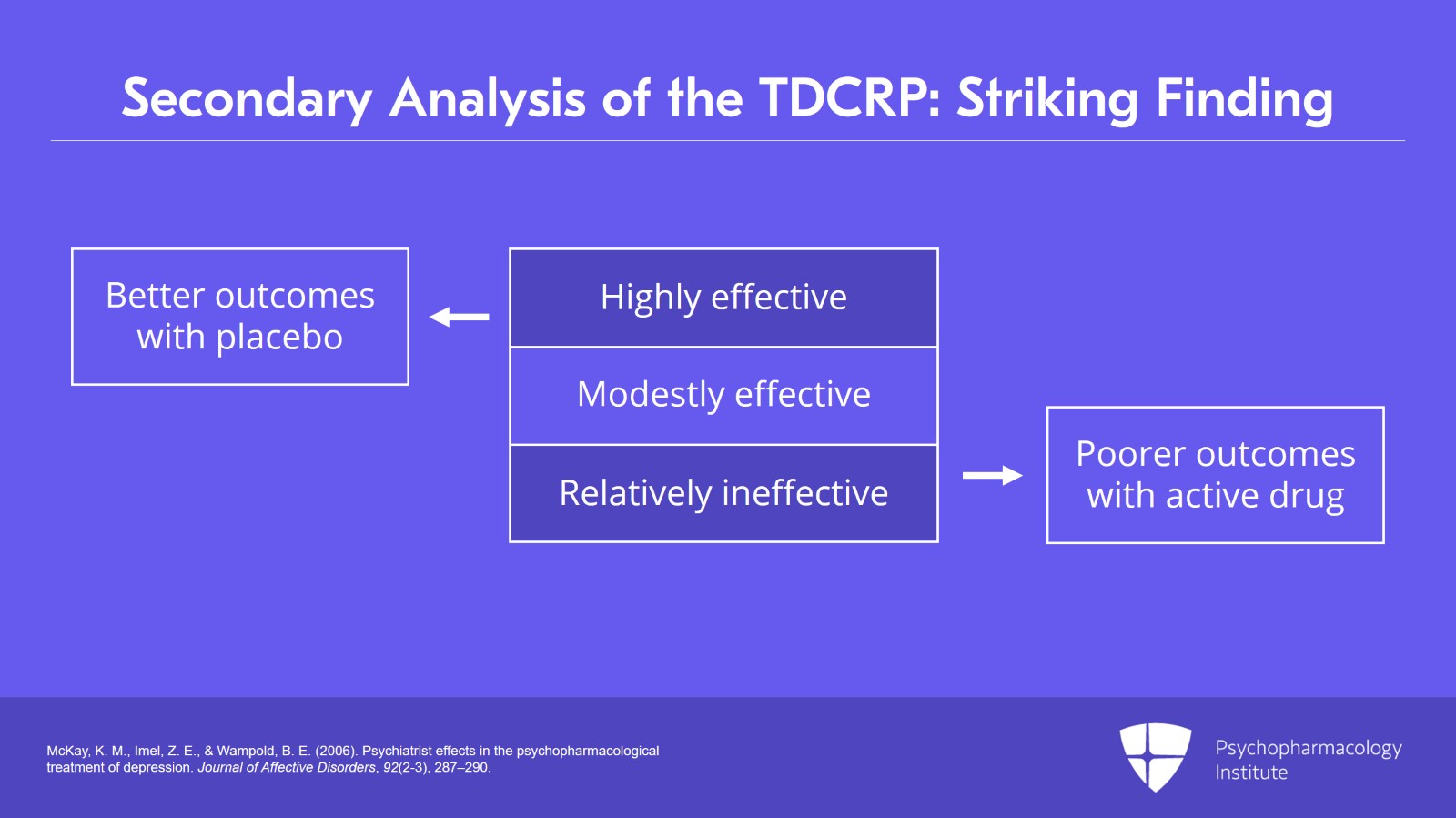
And so using the statistical technique of linear hierarchical modeling, they are able to stratify the prescribers in this study into those who were highly effective or got good results, those who were modestly effective and those who tended to be relatively ineffective in their prescribing.
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
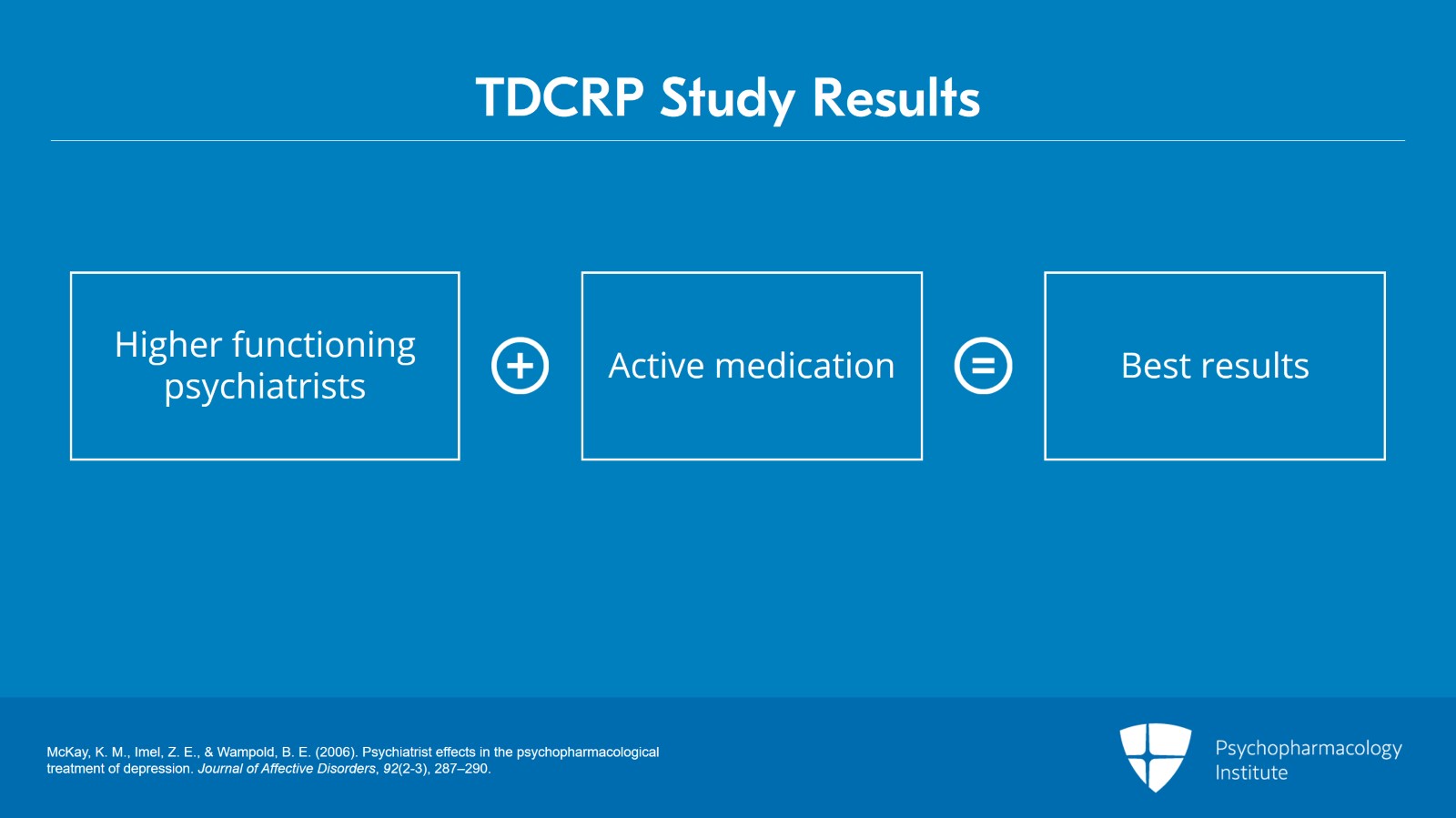
Slide 9 of 25
And of course, in terms of the study results, the effects were additive. So the psychiatrists who were rated as the higher functioning psychiatrists when they used the active medication tended to get the best results.
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
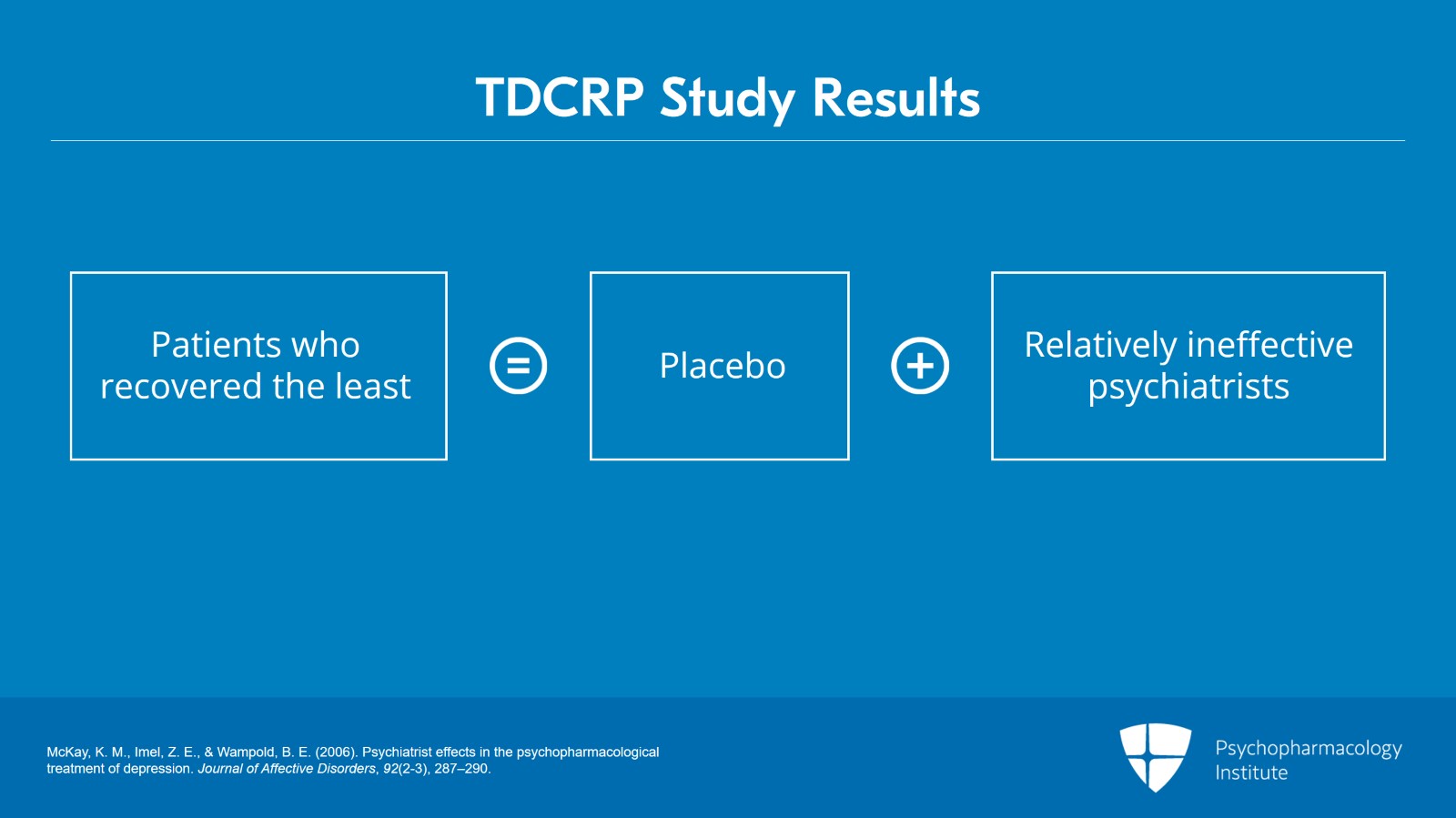
Slide 10 of 25
The patients who recovered least in the study were those who got a placebo and had the psychiatrists who were relatively ineffective.
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 25
I think the really striking finding in this study was that the top 1/3 of psychiatrists got better outcomes with placebo than the bottom third got with active drug. Just, just think for a second about what this means. The top third of psychiatrists did better giving placebo than the bottom third did prescribing an active antidepressant.
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
Slide 12 of 25
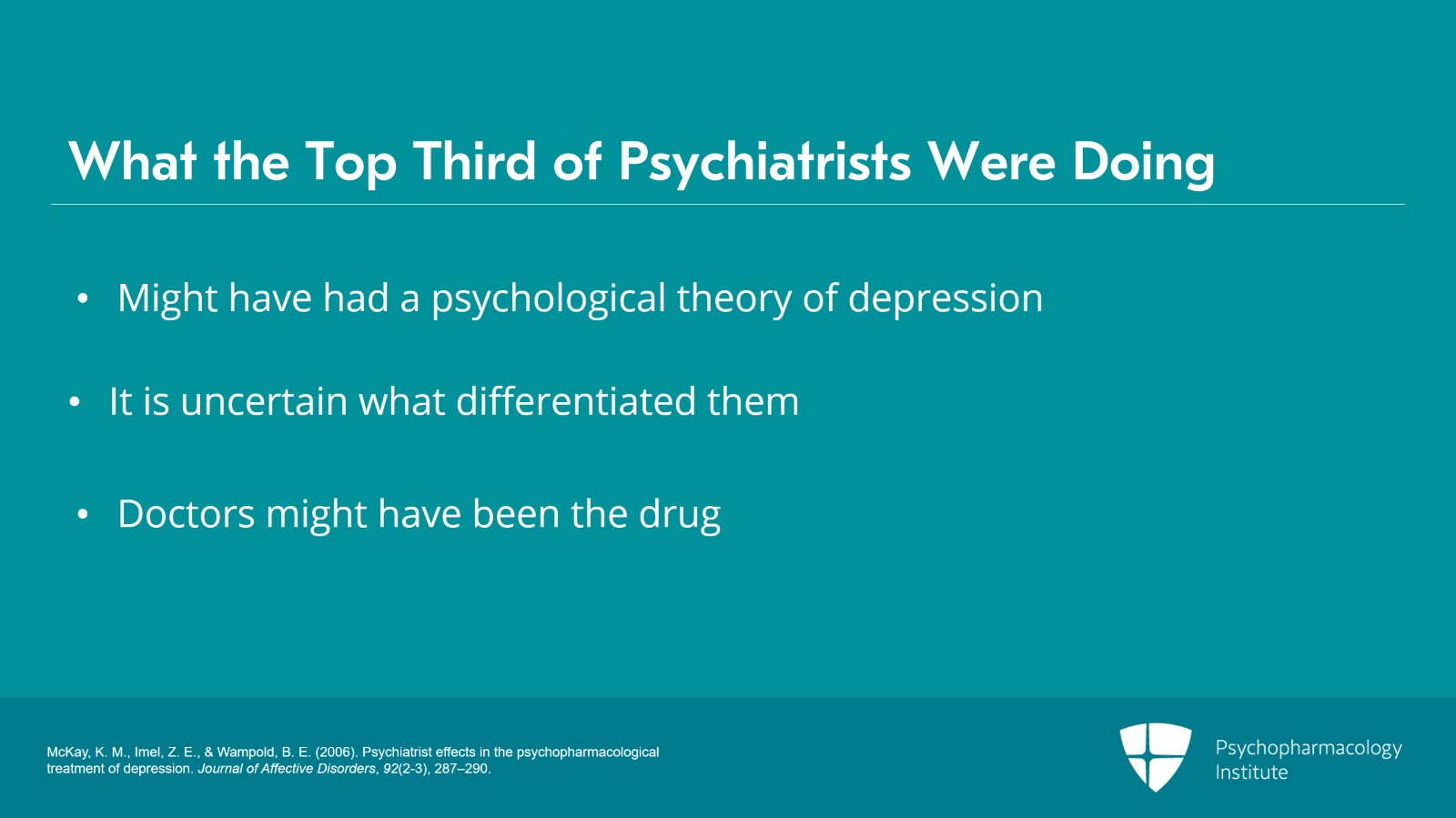
And you know, we do not actually know what those top third of psychiatrists were doing because process research is difficult and I think nobody is getting rich by doing that but there is a suggestion based on another arm of that study that suggests that the clinicians who had a psychological theory of depression seemed to get better results than those who had a purely biomedical theory of depression. Now, that was looking at all of the people in the study, the therapists, the people who were doing psychotherapy and the people who were doing medications so it wasn't broken down. So we don't know for sure that, that is the thing that differentiated the doctors but it does highlight I think what Michael Balint, the psychoanalyst who gave us the concept of patient centeredness and also I think the concept of the psychodynamic formulation when he said in 1958 “the doctor is the drug.”
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 25
And I think we need to keep in mind that our presence with the patient, the way we sit with the patient makes a huge difference.
References:
- McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of Affective Disorders, 92(2-3), 287–290.
Slide 14 of 25
The characteristics of the pill also affect outcome. So the color of the pill makes a difference. And we know in terms of placebo research red pills tend to be energizing and blue pills tend to be calming in most cases but not all cases. We know shapes of the pills, the route of administration, all affect how well our pills work and expensive pills appear also to work better. So if a patient is in the course of a study is led to believe the pill they're taking is, you know, 25 cents or like $85, if the patient thinks they're getting the more expensive pill, they tend to have a bigger response.
References:
- De Craen, A. J., Roos, P. J., De Vries, A. L., & Kleijnen, J. (1996). Effect of colour of drugs: Systematic review of perceived effect of drugs and of their effectiveness. BMJ, 313(7072), 1624-1626.
- Waber, R. L., Shiv, B., Carmon, Z., & Ariely, D. (2008). Commercial features of placebo and therapeutic efficacy. JAMA, 299(9), 1016.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 25
In terms again of the power of the psychological dimension of all of this, placebo effects are a major factor in psychiatric treatment outcomes and particularly with antidepressants. The evidence suggests that more than 3/4 of medication effects can be attributed to placebo. In a lot of published meta-analyses, it's maybe closer to 50% but those studies of course have the problem of publication bias so if the study finds that the drug is effective, it's more likely to get published and if it finds there's no difference from placebo, that study is much more likely to languish on the researchers' desk and eventually fall into the garbage can and disappear.
References:
- Kirsch, I. (2014). Antidepressants and the placebo effect. Zeitschrift für Psychologie, 222(3), 128-134.
- Khan, A., Warner, H. A., & Brown, W. A. (2000). Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials. Archives of General Psychiatry, 57(4), 311.
Slide 16 of 25
But a number of researchers have looked at a relatively unbiased sample which is the FDA drug study database. And when you're proposing a new medication, you tell the FDA, I am going to do these studies and the FDA gets all those studies whether they have a positive finding or a negative finding. So that's a relatively unbiased sample. And a number of researchers, Kirsch and Sapirstein; Khan, Warner and Brown; and Kirsch, Moore and Scoboria, all looked at this particular database. And when looking at that database for antidepressants, what they found was somewhere between 75% and 81% of drug response with antidepressants is attributable to the placebo effect.
References:
- Kirsch, I. (2014). Antidepressants and the placebo effect. Zeitschrift für Psychologie, 222(3), 128-134.
- Khan, A., Warner, H. A., & Brown, W. A. (2000). Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials. Archives of General Psychiatry, 57(4), 311.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 25
And it is really important to hold in mind that placebo does not mean imaginary. I mean, these are real effects. I mean, we know you can lower blood pressure with placebos. You can give somebody a placebo analgesic and put a myograph needle in a nerve and measure a decrease in pain transmission. So the mental factor is extremely powerful and real and persistent, and actually probably is getting bigger as people place more and more stock in pharmacotherapy.
References:
- Kirsch, I. (2014). Antidepressants and the placebo effect. Zeitschrift für Psychologie, 222(3), 128-134.
- Khan, A., Warner, H. A., & Brown, W. A. (2000). Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials. Archives of General Psychiatry, 57(4), 311.
Slide 18 of 25
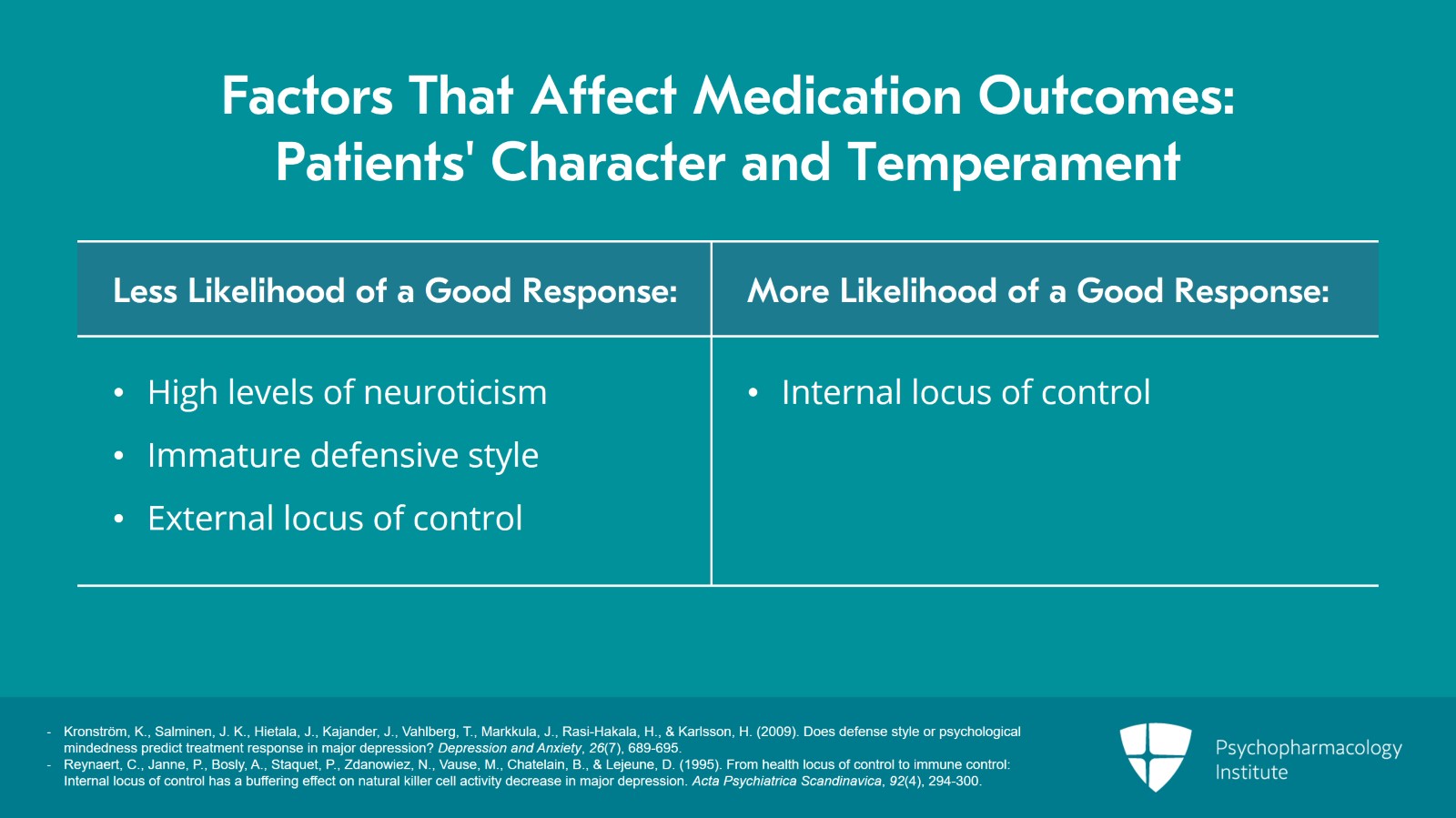
Another factor in terms of who the patient is that influences how medications are going to work is character and temperament. So we know that our patients with higher levels of neuroticism are less likely to have a good antidepressant response. Similarly, patients with immature defensive style are also less likely to have a good antidepressant response and these are patients for whom combination at least with psychotherapy is probably indicated. Patients who have an internal locus of control actually do better with antidepressants than patients who have an external locus of control.
References:
- Kronström, K., Salminen, J. K., Hietala, J., Kajander, J., Vahlberg, T., Markkula, J., Rasi-Hakala, H., & Karlsson, H. (2009). Does defense style or psychological mindedness predict treatment response in major depression? Depression and Anxiety, 26(7), 689-695.
- Reynaert, C., Janne, P., Bosly, A., Staquet, P., Zdanowiez, N., Vause, M., Chatelain, B., & Lejeune, D. (1995). From health locus of control to immune control: Internal locus of control has a buffering effect on natural killer cell activity decrease in major depression. Acta Psychiatrica Scandinavica, 92(4), 294-300.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 25
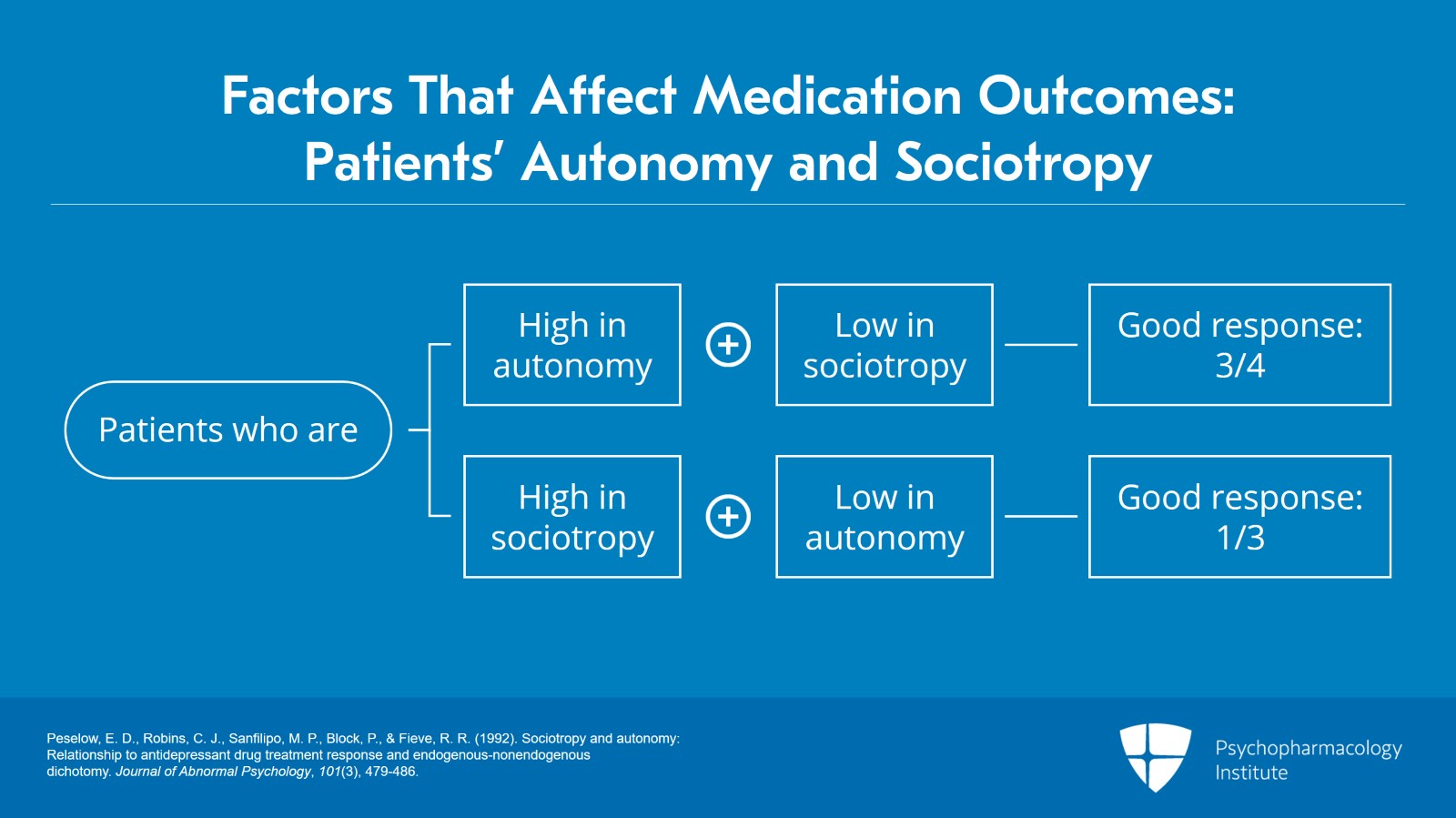
And the dimensions of autonomy and sociotropy also influence medication outcomes. So I think you understand what autonomy is, people who feel like they're self-motivated, in charge of themselves, you know, willing to go their own way. Sociotropy is a personality characteristic where people are highly attuned to their social environment, anxiously attuned. They want to please. They have a hard time disagreeing and are really quite concerned with their standing with other people. So patients who are high in autonomy and low in sociotropy have, about 3/4 of them will have a good antidepressant response. Whereas, patients who are high in sociotropy and low in autonomy, only about a third of those patients will have a good antidepressant response.
References:
- Peselow, E. D., Robins, C. J., Sanfilipo, M. P., Block, P., & Fieve, R. R. (1992). Sociotropy and autonomy: Relationship to antidepressant drug treatment response and endogenous-nonendogenous dichotomy. Journal of Abnormal Psychology, 101(3), 479-486.
Slide 20 of 25
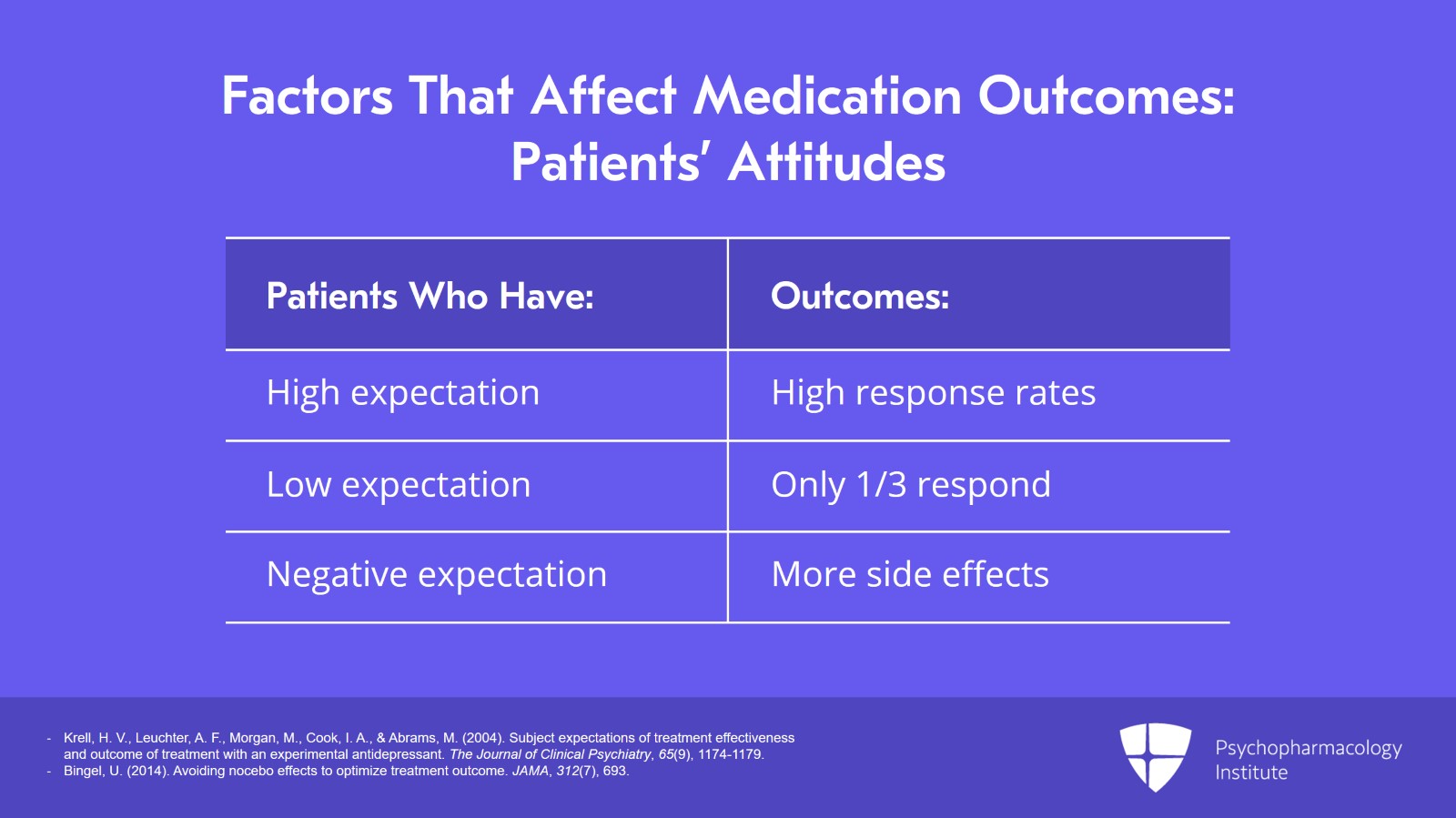
Our patients' attitudes also affect how well medications are going to work. So we know that patients who have very high expectations of treatment also have very high response rates, as much as 90% to antidepressants. Whereas, those patients who have a low expectation, only about a third of those are going to respond to antidepressants. And also, in terms of expectations, we know that negative expectations of treatment make it more likely that patients are going to experience side effects which really are in many cases nocebo responses related to the expectation of being harmed.
References:
- Krell, H. V., Leuchter, A. F., Morgan, M., Cook, I. A., & Abrams, M. (2004). Subject expectations of treatment effectiveness and outcome of treatment with an experimental antidepressant. The Journal of Clinical Psychiatry, 65(9), 1174-1179.
- Bingel, U. (2014). Avoiding nocebo effects to optimize treatment outcome. JAMA, 312(7), 693.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 25
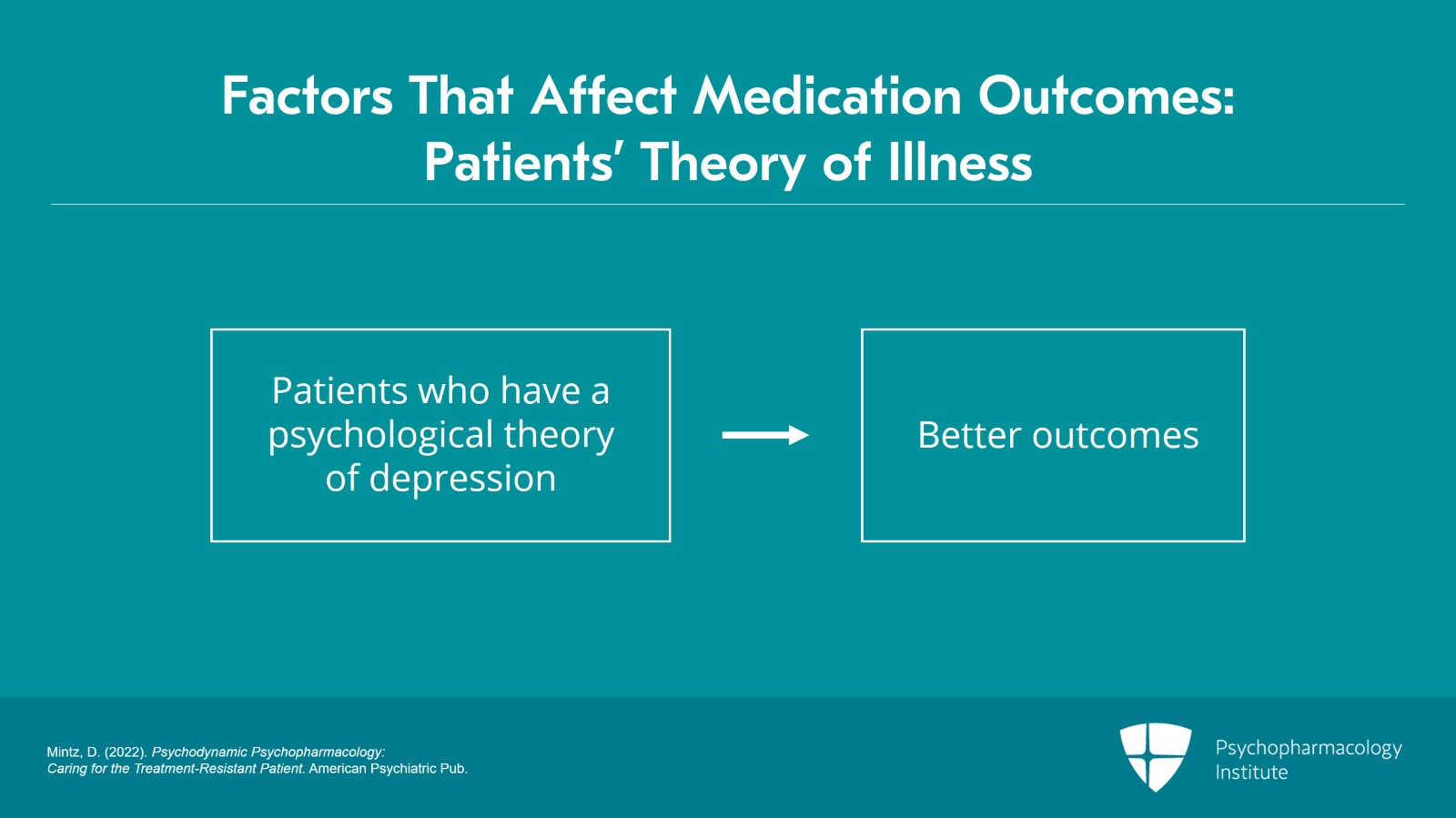
In terms of patient attitudes also, lastly, it is worth noting that the patient's theory of illness influences how their medications are going to work. So it turns out actually that patients who have a psychological theory of depression, who view their depression as nonbiologic tend actually to have better outcomes with antidepressants at least with mild-to-moderate depression. It seems like once you get into severe depression this, this demarcation does not hold. But for patients with mild-to-moderate depression, they are more likely to benefit if they see their depression as psychologic.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Slide 22 of 25
So just to reiterate, some key points: First of all, I think while Psychiatry has become increasingly focused on the provision of evidence-based treatment. In practice this is often meant to focus on the biomedical evidence base which connects medication response with particular diagnostic categories.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 25
And at the same time, there has been a general neglect of the psychosocial evidence base that I'm describing that provides guidance to the prescriber on how to prescribe rather than on what to prescribe in order to achieve optimum outcomes. In many cases actually, psychosocial factors exert a larger effect on medication outcome than does the actual medication.
Slide 24 of 25
And as we said, the person of the prescriber as well as the patient's history, temperament, attitudes and beliefs, all profoundly shape treatment outcomes and should be considered by us when we're trying to address our patients and particularly our treatment-refractory patients.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.