Slides and Transcript
Slide 1 of 17
So we’ve been talking about some of the science of the art of Psychopharmacotherapy and we’re going to continue in that vein.
At this point, we’re going to focus on where we left off which is the biogenetic theory of illness and how that affects our patients in various ways.
Slide 2 of 17
Now, a reductionistically biological theory of illness has been promoted I think in our current culture not just by drug companies who would prefer that patients see their troubles through a biomedical lens but also very well-meaning national campaigns I think intended to reduce stigma.
References:
- Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., & Link, B. G. (2010). “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry, 167(11), 1321-1330.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 17
And the evidence suggests in fact that these campaigns to really reformulate and push the idea that psychiatric illnesses are simply biomedical or biological does increase social acceptance of drug treatment. And some studies suggest it may reduce self-blame although not all studies.
References:
- Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., & Link, B. G. (2010). “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry, 167(11), 1321-1330.
- Deacon, B. J., & Baird, G. L. (2009). The chemical imbalance explanation of depression: Reducing blame at what cost? Journal of Social and Clinical Psychology, 28(4), 415-435.
Slide 4 of 17
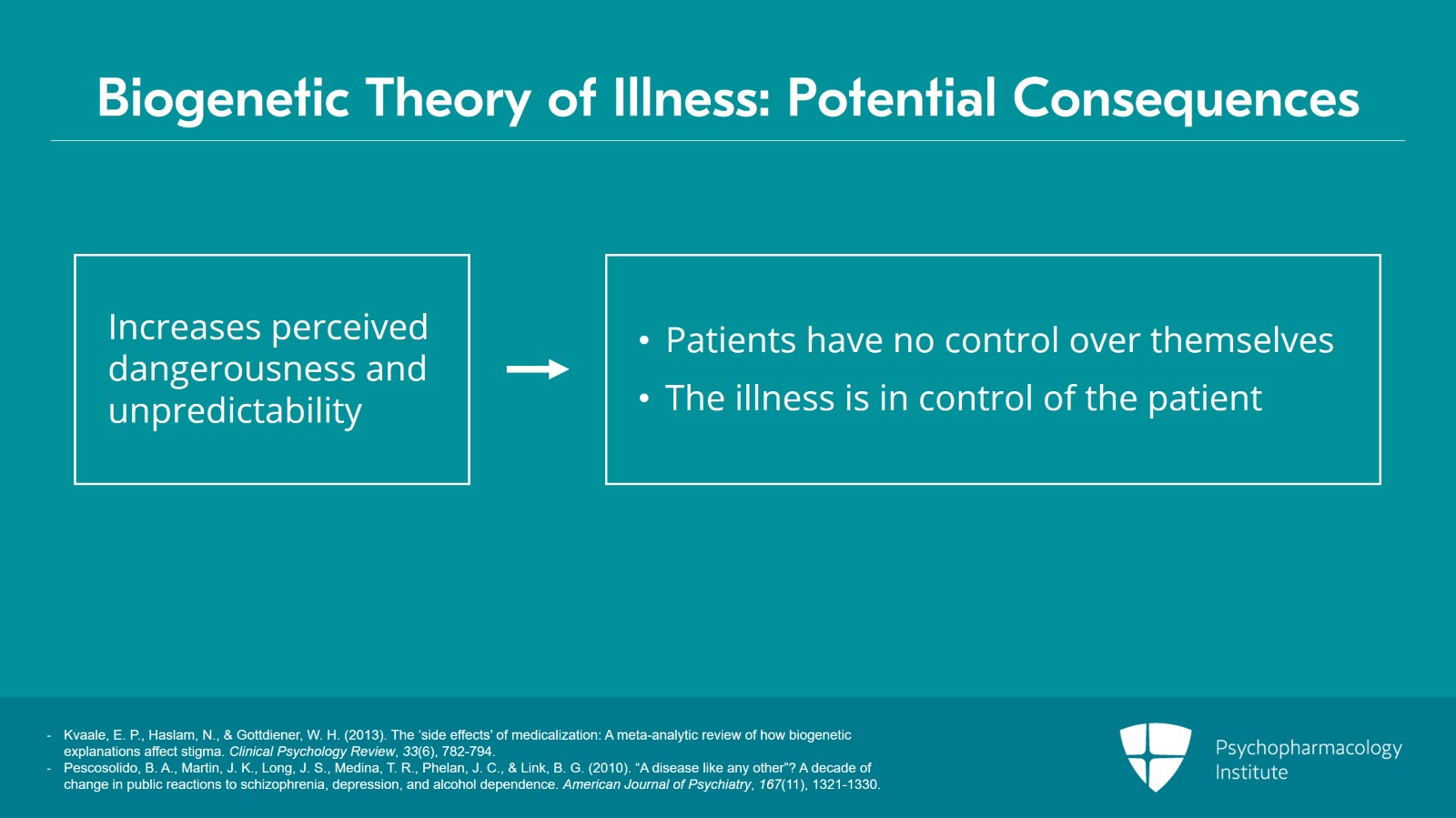
But the evidence interestingly suggests that in very important powerful ways a biogenetic theory of illness actually exacerbates stigma in many other dimensions.
So for example, people who adhere to a biomedical theory of illness are actually less willing to accept a medically ill person into one’s neighborhood, into one’s family, into one’s place of work, etc.
And so holding a biomedical theory of illness increases social distance between the person with that belief and the patient who has a psychiatric illness.
References:
- Kvaale, E. P., Haslam, N., & Gottdiener, W. H. (2013). The ‘side effects’ of medicalization: A meta-analytic review of how biogenetic explanations affect stigma. Clinical Psychology Review, 33(6), 782-794.
- Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., & Link, B. G. (2010). “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry, 167(11), 1321-1330.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 17
Biomedical theories of illness also appear to increase perceived dangerousness and unpredictability of people with psychiatric illnesses so perhaps it’s, you know, you feel like it’s biomedical so somebody has no control over it. And so they have no control over themselves and so they are more likely to act in the fantasy irrationally because the illness is in control of them and they’re not in control of themselves.
References:
- Kvaale, E. P., Haslam, N., & Gottdiener, W. H. (2013). The ‘side effects’ of medicalization: A meta-analytic review of how biogenetic explanations affect stigma. Clinical Psychology Review, 33(6), 782-794.
- Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., & Link, B. G. (2010). “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry, 167(11), 1321-1330.
Slide 6 of 17
We also know that holding a biomedical theory of illness decreases physician empathy towards patients across diagnoses of depression, schizophrenia, substance use and the more biomedical your theory is, the less likely you are to relate empathically towards your patients and we know and we’ll talk about in a bit that the degree of empathy we have for our patients also is a factor that influences treatment outcome.
References:
- Lebowitz, M. S., & Ahn, W. (2014). Effects of biological explanations for mental disorders on clinicians’ empathy. Proceedings of the National Academy of Sciences, 111(50), 17786-17790.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 17
We’ve been talking on a social level and the effects that, that belief has on a cultural level. But biomedical theory of illness also has very specific effects on the individual.
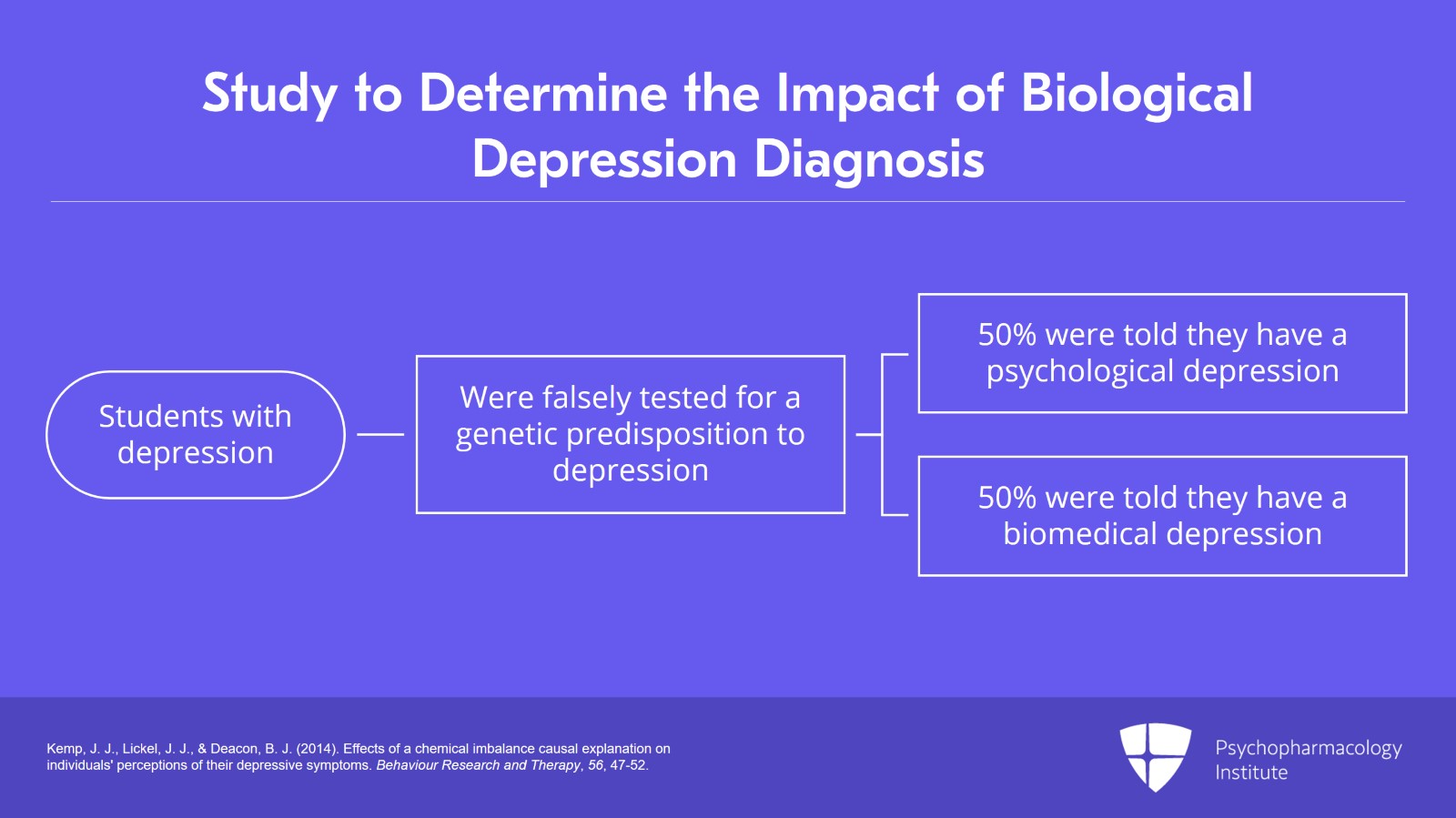
So an interesting study done by Kemp, Lickel and Deacon in 2014 took college students with a history of depression and they enrolled them in a study to determine if their depression was psychological or biological in nature.
So a researcher came in a white coat, did a cheek swab and went back to the lab to determine whether the person was genetically predetermined to have depression or not. Of course, there’s no study like this. So this was a sham condition.
And then 15 minutes later, the researcher comes back and informs the patient randomly of the nature of the depression after this cheek swab test. And so, you know, half the patients were told they had a psychological depression and half were told they had a biomedically determined depression.
References:
- Kemp, J. J., Lickel, J. J., & Deacon, B. J. (2014). Effects of a chemical imbalance causal explanation on individuals' perceptions of their depressive symptoms. Behaviour Research and Therapy, 56, 47-52.
Slide 8 of 17
And first of all, in this study, it turned out that the biogenetic theory failed to reduce self-blame but more importantly it increased prognostic pessimism which is a factor known to influence treatment outcomes. So the more likely you are to be optimistic about outcome, the more likely you are to have a good outcome and less likely you are, of course, the less likely you are to have a good outcome.
References:
- Kemp, J. J., Lickel, J. J., & Deacon, B. J. (2014). Effects of a chemical imbalance causal explanation on individuals' perceptions of their depressive symptoms. Behaviour Research and Therapy, 56, 47-52.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 17
And then, Kemp, Lickel and Deacon found this but a number of other researchers, Deacon and Baird in 2009; Lebowitz, Ahn and Nolen-Hoeksema in 2013, all found that a biomedical theory tends to decrease the patient’s optimism about treatment outcomes. It also worsens mood regulation expectancies so patients just feel there’s less I can do to manage my mood because it’s biological. And we know again that negative mood regulation, expectations also negatively influence treatment outcomes and, you know, generally decreases self-efficacy in managing depression.
References:
- Deacon, B. J., & Baird, G. L. (2009). The chemical imbalance explanation of depression: Reducing blame at what cost? Journal of Social and Clinical Psychology, 28(4), 415-435.
- Kemp, J. J., Lickel, J. J., & Deacon, B. J. (2014). Effects of a chemical imbalance causal explanation on individuals' perceptions of their depressive symptoms. Behaviour Research and Therapy, 56, 47-52.
Slide 10 of 17
So you know, this connects with what I was saying before in a previous lecture about how patients with mild-to-moderate depression have better outcomes when they have a psychosocial theory of illness rather than a biomedical theory.
References:
- Deacon, B. J., & Baird, G. L. (2009). The chemical imbalance explanation of depression: Reducing blame at what cost? Journal of Social and Clinical Psychology, 28(4), 415-435.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 17
So you know, certainly one implication of this is, you know, we have to be mindful about how we talk to our patients in ways that takes seriously the biomedical aspects of depression but continue to emphasize that there are psychosocial aspects and that the patient does have the potential to influence by their own psychology or behavior the outcome of their illness and so they’re not simply helpless in the face of some inexorable biology.
References:
- Deacon, B. J., & Baird, G. L. (2009). The chemical imbalance explanation of depression: Reducing blame at what cost? Journal of Social and Clinical Psychology, 28(4), 415-435.
- Kemp, J. J., Lickel, J. J., & Deacon, B. J. (2014). Effects of a chemical imbalance causal explanation on individuals' perceptions of their depressive symptoms. Behaviour Research and Therapy, 56, 47-52.
Slide 12 of 17
The patient’s interpersonal positions also influence medication outcomes. Particularly, this is true around social disadvantage. So we know that people from socially disadvantaged groups, people that are historically oppressed, minorities, women as well as, as people from lower socioeconomic statuses are all more likely to experience nocebo responses in relation to medications or placebos.
References:
- Hahn, R. A. (1997). The nocebo phenomenon: Concept, evidence, and implications for public health. Preventive Medicine, 26(5), 607-611.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 17
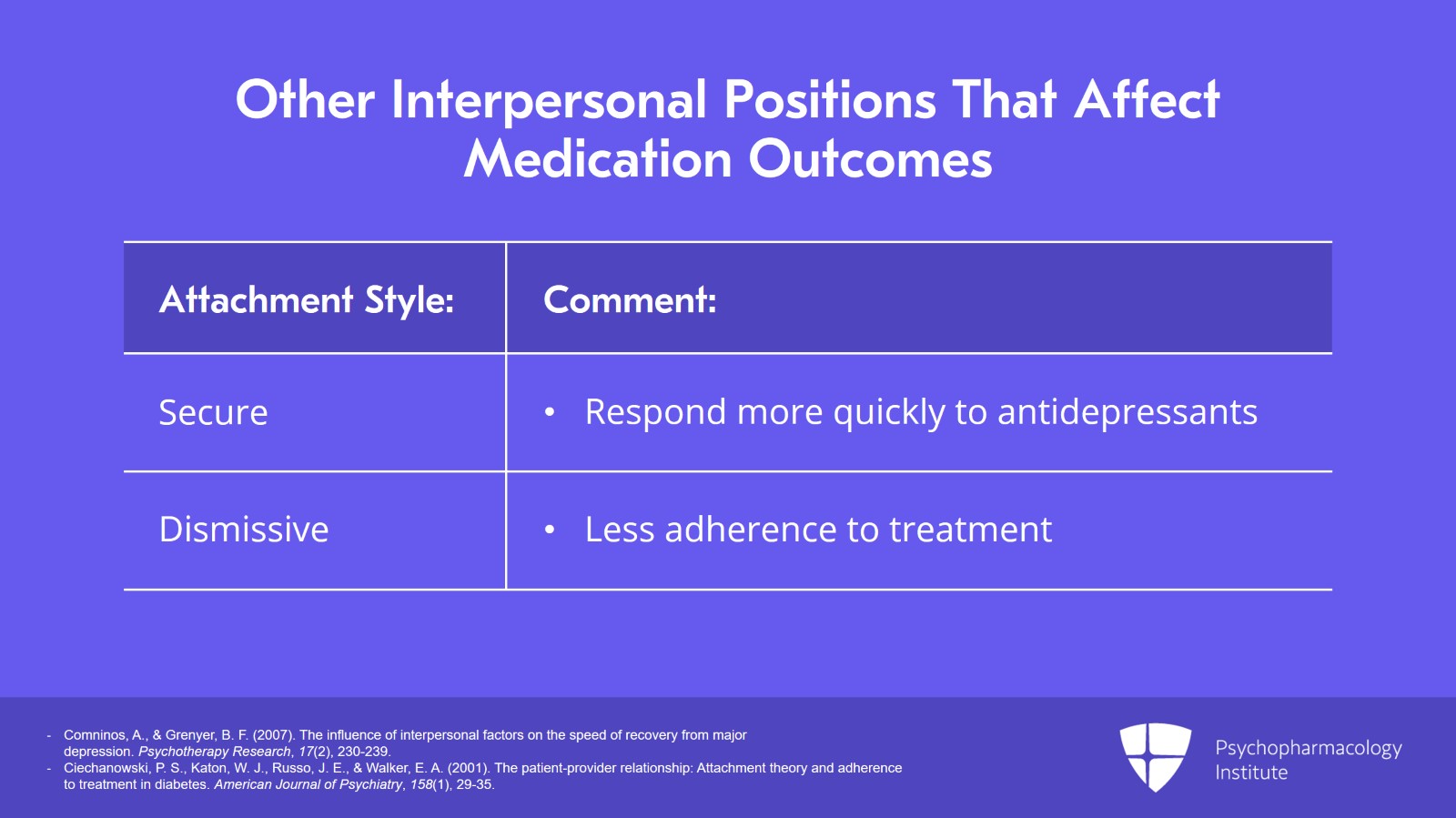
Other interpersonal positions also affect medication outcomes.
So patient’s attachment style, affects how treatments are going to work. We know that patients who have secure attachments tend to respond more quickly, for example, to antidepressants.
And attachment style also affects adherence. And you know, interesting studies from the diabetes literature suggest that dismissive attachment styles lead to, you know, less adherence to treatment and that includes taking one’s medications but also behavioral recommendations. And so patients with dismissive attachment styles tend to have much higher levels of HbA1c, higher levels of glucose in their blood. But patients with a dismissive attachment style who have physicians who are particularly good communicators do not have that same increase in hemoglobin A1c.
References:
- Comninos, A., & Grenyer, B. F. (2007). The influence of interpersonal factors on the speed of recovery from major depression. Psychotherapy Research, 17(2), 230-239.
- Ciechanowski, P. S., Katon, W. J., Russo, J. E., & Walker, E. A. (2001). The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. American Journal of Psychiatry, 158(1), 29-35.
Slide 14 of 17
So the implication being again as you’ve done your evaluation of your patient and if you have determined that they have a dismissive attachment style, which occurs in 17% of the general population and higher likely in a psychiatric population, that is a patient for whom you would think I have to be particularly mindful about having good communication because you can erase the negative effect of that personality style.
References:
- Ciechanowski, P. S., Katon, W. J., Russo, J. E., & Walker, E. A. (2001). The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. American Journal of Psychiatry, 158(1), 29-35.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 17
So to recap a few key points, first of all, while a biological theory of mental illness has been championed for some good reasons such as the effort to reduce stigma, it appears largely to have backfired, actually in many cases increasing the stigma of mental illness.
In many cases, a biogenetic theory of mental illness undermines positive outcomes negatively affecting prognosis by decreasing a sense of hope and personal efficacy and decreasing clinician empathy.
Slide 16 of 17
And biogenetic explanations really should be balanced with psychoeducation emphasizing the patient’s efficacy as agents in their own recovery.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.