Slides and Transcript
Slide 2 of 15
So tardive symptoms have a widely varying remission rate, with remission most likely in younger patients, only about 50% of the time. Tardive symptoms do not appear to become more severe in patients maintained on therapy. However, once the symptoms occur, they may persist for decades. In some cases, they may even be permanent, and this is now a finding that’s been replicated across several cohorts. And in these cases, especially, treatment is required.
References:
- Gardos, G., Casey, D. E., Cole, J. O., Perenyi, A., Kocsis, E., Arato, M., Samson, J. A., & Yeghiayan, S. K. (1994). Ten-year outcome of tardive dyskinesia. American Journal of Psychiatry, 151(6), 836-841. https://doi.org/10.1176/ajp.151.6.836
- Tarsy, D., & Baldessarini, R. J. (1984). Tardive dyskinesia. Annual Review of Medicine, 35, 605–623. https://doi.org/10.1146/annurev.me.35.020184.003133
- Rittmannsberger, H. (2008). Ten year outcome of tardive dyskinesia during continuous treatment with first generation antipsychotics. Psychiatria Danubina, 20(4), 461–465.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
Psychosis is often chronic, necessitating ongoing treatment with antipsychotics despite the tardive syndromes. And so we all know that unfortunately we continue to treat many patients with these offending medications because the psychosis is worse than the tardive syndrome in terms of its overall impact on their quality of life and function.
References:
- Caroff, S. N., Davis, V. G., Miller, D. D., Davis, S. M., Rosenheck, R. A., McEvoy, J. P., Campbell, E. C., Saltz, B. L., Riggio, S., Chakos, M. H., Swartz, M. S., Keefe, R. S., Stroup, T. S., Lieberman, J. A., & CATIE Investigators. (2011). Treatment outcomes of patients with tardive dyskinesia and chronic schizophrenia. The Journal of Clinical Psychiatry, 72(3), 295–303. https://doi.org/10.4088/JCP.09m05793yel
Slide 4 of 15
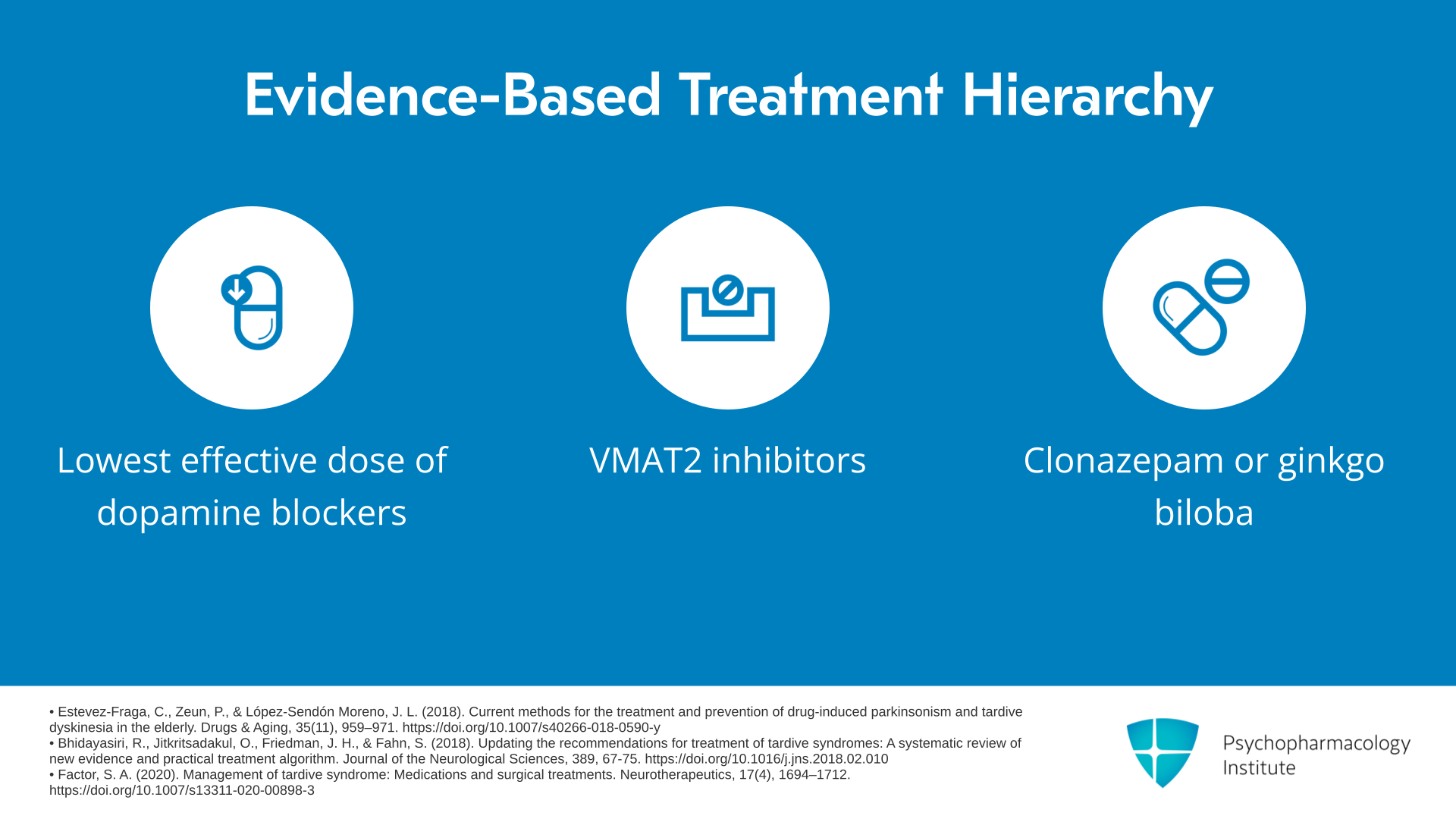
So let’s talk about a proposed treatment algorithm for tardive syndromes. When using medications known to cause tardive syndromes, because of this risk of long-term or even permanent tardive syndromes, you really want to try to use the smallest effective dose.
References:
- Estevez-Fraga, C., Zeun, P., & López-Sendón Moreno, J. L. (2018). Current methods for the treatment and prevention of drug-induced parkinsonism and tardive dyskinesia in the elderly. Drugs & Aging, 35(11), 959–971. https://doi.org/10.1007/s40266-018-0590-y
- Factor, S. A. (2020). Management of tardive syndrome: Medications and surgical treatments. Neurotherapeutics, 17(4), 1694–1712. https://doi.org/10.1007/s13311-020-00898-3
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
Now, once you recognize a tardive syndrome, there’s really insufficient evidence to know with certainty whether withdrawing or switching from typical to atypical antipsychotics will help the tardive dyskinesia, but both strategies are often tried. The evidence is not great. There is some evidence that quetiapine, and particularly clozapine, might improve tardive dyskinesia on cross-taper from the offending agent. However, this remains uncertain due to limited evidence, but it’s another strategy you might try.
References:
- Estevez-Fraga, C., Zeun, P., & López-Sendón Moreno, J. L. (2018). Current methods for the treatment and prevention of drug-induced parkinsonism and tardive dyskinesia in the elderly. Drugs & Aging, 35(11), 959–971. https://doi.org/10.1007/s40266-018-0590-y
- Bhidayasiri, R., Fahn, S., Weiner, W. J., Gronseth, G. S., Sullivan, K. L., Zesiewicz, T. A., & American Academy of Neurology. (2013). Evidence-based guideline: Treatment of tardive syndromes: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 81(5), 463-469. https://doi.org/10.1212/WNL.0b013e31829d86b6
Slide 6 of 15
For severe and disabling tardive symptoms, you might consider a second-generation VMAT2 inhibitor, so deuterated tetrabenazine and valbenazine are first line with level A evidence. So these are really your evidence-based standards when you have to treat tardive dyskinesia.
References:
- Bhidayasiri, R., Fahn, S., Weiner, W. J., Gronseth, G. S., Sullivan, K. L., Zesiewicz, T. A., & American Academy of Neurology. (2013). Evidence-based guideline: Treatment of tardive syndromes: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 81(5), 463-469. https://doi.org/10.1212/WNL.0b013e31829d86b6
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
With deuterated tetrabenazine, you’re going to start at about 6 mg twice a day, and then you can increase weekly by 6 mg per day, up to 48 mg per day. The common side effects are somnolence, diarrhea, dry mouth, and fatigue. It does carry a black box warning in Huntington’s disease, as it may increase the risk of depression and suicidal ideation. And it’s contraindicated in severely depressed or suicidal patients.
References:
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
- Anderson, K. E., Stamler, D., Davis, M. D., Factor, S. A., Hauser, R. A., Isojärvi, J., … & Fernandez, H. H. (2017). Deutetrabenazine for treatment of involuntary movements in patients with tardive dyskinesia (AIM-TD): A double-blind, randomised, placebo-controlled, phase 3 trial. The Lancet Psychiatry, 4(8), 595-604. https://doi.org/10.1016/S2215-0366(17)30236-5
Slide 8 of 15
Valbenazine, you want to start at around 40 mg daily and increase to 80 mg daily after about a week. Side effects include somnolence, QT prolongation, and parkinsonism. And then they advised that you not use this with monoamine oxidase inhibitors.
References:
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
- Hauser, R. A., Factor, S. A., Marder, S. R., Knesevich, M. A., Ramirez, P. M., Jimenez, R., … O'Brien, C. F. (2017). KINECT 3: A Phase 3 randomized, double-blind, placebo-controlled trial of valbenazine for tardive dyskinesia. American Journal of Psychiatry, 174(5), 476–484. https://doi.org/10.1176/appi.ajp.2017.16091037
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
While efficacy and incidence of adverse events are comparable, deuterated tetrabenazine must be dosed twice per day, while valbenazine is dosed just once per day. Deuterated tetrabenazine is also indicated for chorea associated with Huntington’s disease, but carries that black box warning I just mentioned for increased risk of depression and suicidal ideation. So those are some of the differences.
References:
- Bhidayasiri, R., Fahn, S., Weiner, W. J., Gronseth, G. S., Sullivan, K. L., Zesiewicz, T. A., & American Academy of Neurology. (2013). Evidence-based guideline: Treatment of tardive syndromes: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 81(5), 463-469. https://doi.org/10.1212/WNL.0b013e31829d86b6
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
Slide 10 of 15
First-generation VMAT2 inhibitor tetrabenazine has only level C evidence, meaning it’s possibly effective and has a more severe side effect profile. So, we don’t consider it first-line therapy. So you’re going to want to start with one of those second-generation VMAT2 inhibitors.
References:
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
- Ricciardi, L., Pringsheim, T., Barnes, T. R., Martino, D., Gardner, D., Remington, G., Addington, D., Morgante, F., Poole, N., Carson, A., Edwards, M., Fox, S., Lang, A., Fahn, S., & Espay, A. J. (2019). Treatment recommendations for tardive dyskinesia. Canadian Journal of Psychiatry, 64(6), 388-399. https://doi.org/10.1177/0706743719828968
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
Anticholinergics, although commonly used, lack evidence for efficacy and have significant side effects especially in the elderly. Clonazepam probably improves tardive dyskinesia. It’s got level B evidence. Ginkgo biloba probably improves tardive syndromes. It’s got level B evidence.
References:
- Bergman, H., & Soares-Weiser, K. (2018). Anticholinergic medication for antipsychotic-induced tardive dyskinesia. The Cochrane Database of Systematic Reviews, 1(1), CD000204. https://doi.org/10.1002/14651858.CD000204.pub2
- Bhidayasiri, R., Fahn, S., Weiner, W. J., Gronseth, G. S., Sullivan, K. L., Zesiewicz, T. A., & American Academy of Neurology. (2013). Evidence-based guideline: Treatment of tardive syndromes: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 81(5), 463-469. https://doi.org/10.1212/WNL.0b013e31829d86b6
Slide 12 of 15
So in cases that do not fully respond to a single agent, monotherapy, combining a second-generation VMAT2 inhibitor, for instance, with clonazepam or ginkgo biloba may be a good strategy. So if you’ve gotten partial relief, partial response, go ahead and add maybe some clonazepam or ginkgo biloba. Combination with ginkgo biloba first. Then, if it’s unsuccessful, maybe go to clonazepam. That would be going in order of risk of side effects.
References:
- Estevez-Fraga, C., Zeun, P., & López-Sendón Moreno, J. L. (2018). Current methods for the treatment and prevention of drug-induced parkinsonism and tardive dyskinesia in the elderly. Drugs & Aging, 35(11), 959–971. https://doi.org/10.1007/s40266-018-0590-y
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
Now, in terms of amantadine, it’s considered level C evidence for treating these syndromes. Focal dystonia may be treated with botulinum toxin, but there’s insufficient evidence to formally recommend but just something in outlier cases to consider. There are case studies that support deep brain stimulation with lead placement in the globus pallidus interna for severe tardive dyskinesia. Again, that’s only level C, and it’s fairly invasive.
References:
- Estevez-Fraga, C., Zeun, P., & López-Sendón Moreno, J. L. (2018). Current methods for the treatment and prevention of drug-induced parkinsonism and tardive dyskinesia in the elderly. Drugs & Aging, 35(11), 959–971. https://doi.org/10.1007/s40266-018-0590-y
- Bhidayasiri, R., Fahn, S., Weiner, W. J., Gronseth, G. S., Sullivan, K. L., Zesiewicz, T. A., & American Academy of Neurology. (2013). Evidence-based guideline: Treatment of tardive syndromes: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 81(5), 463-469. https://doi.org/10.1212/WNL.0b013e31829d86b6
Slide 14 of 15
The lowest effective dose of dopamine blocking agent is still your best first strategy. Then if you have continued symptoms that are causing distress or dysfunction, go to your second-generation VMAT2 inhibitor. Then kind of third tier best evidence is clonazepam or ginkgo biloba, followed by amantadine and GPi DBS, globus pallidus interna DBS again by anecdotal case report.
References:
- Estevez-Fraga, C., Zeun, P., & López-Sendón Moreno, J. L. (2018). Current methods for the treatment and prevention of drug-induced parkinsonism and tardive dyskinesia in the elderly. Drugs & Aging, 35(11), 959–971. https://doi.org/10.1007/s40266-018-0590-y
- Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H., & Fahn, S. (2018). Updating the recommendations for treatment of tardive syndromes: A systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences, 389, 67-75. https://doi.org/10.1016/j.jns.2018.02.010
- Factor, S. A. (2020). Management of tardive syndrome: Medications and surgical treatments. Neurotherapeutics, 17(4), 1694–1712. https://doi.org/10.1007/s13311-020-00898-3
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 15
So the key points for this section are that tardive dyskinesia may persist for years or may even be permanent, requiring treatment to minimize distress and dysfunction. The best-evidence treatment of tardive dyskinesia, lowest effective dose of the dopamine blocking agent, then if required, second-generation VMAT2 inhibitor, followed by clonazepam or ginkgo biloba, amantadine or globus pallidus interna DBS for severe tardive dyskinesia.