Slides and Transcript
Slide 1 of 21
In choosing which medication to start and how to go about this, individual patient characteristics and needs will help determine which medication is best.
Slide 2 of 21
All patients considering treatment for their opioid use disorder should be educated about the effectiveness, risks, and benefits of each of the three medications, also the options of treatment without medications and no treatment.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 21
In choosing which medication to start and how to go about this, you should consider a previous response. Did they have a good benefit with the medication before? Side effects, pain. For example, would they be better served with the full opioid agonist? Use of other substances. For example, naltrexone treats alcohol use disorder. Or if they're using benzodiazepines that are prescribed, buprenorphine may be safer than methadone.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
Slide 4 of 21
Occupation is also important. Some safety sensitive positions, consider naltrexone, injectable naltrexone more than a mu-opioid agonist or partial agonist. If somebody is pregnant, then we might recommend buprenorphine or methadone more. If they're currently using opioids that they cannot take off, for example, for pain or for other reasons, then we may consider not using injectable naltrexone. Access is also very important. Is it reasonable for them to be able to go to an opioid treatment program or is office-based treatment better for them? And of course, patient preference is also important.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
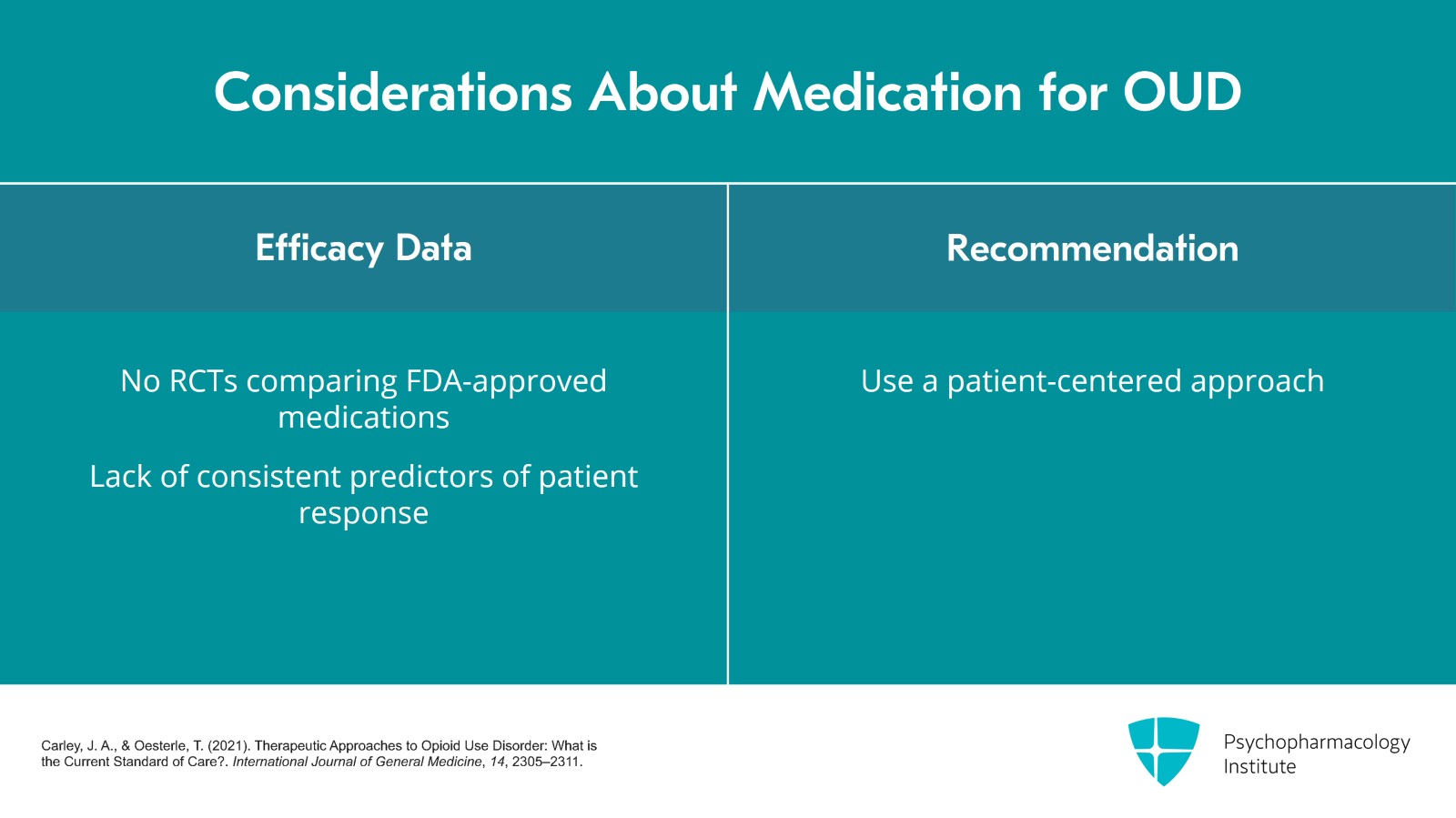
Slide 5 of 21
In terms of efficacy data, as of now, there's no RCT or randomized controlled trial comparing all three FDA-approved medications. So we can't say this medication is definitively better than that medication. There's also no consistent predictor of response and secondary data analysis. Therefore, it's really important to use a patient-centered method to get them the care that they need.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
Slide 6 of 21
In a meta-analysis of 31 trials with over 5000 patients and high to moderate quality studies, there was good evidence that buprenorphine retains patients better than placebo at all doses. There is high quality evidence that flexible buprenorphine dosing was less effective than methadone in retaining patients. For those retained, moderate evidence showed no difference in suppression of opioid use by buprenorphine versus methadone.
References:
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 21
Ultimately, the choice of the two medications has to do with each person's personal circumstance and needs. If somebody is still using opioids, has pain, has access to a methadone clinic or has done well on methadone, it may be a good option.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
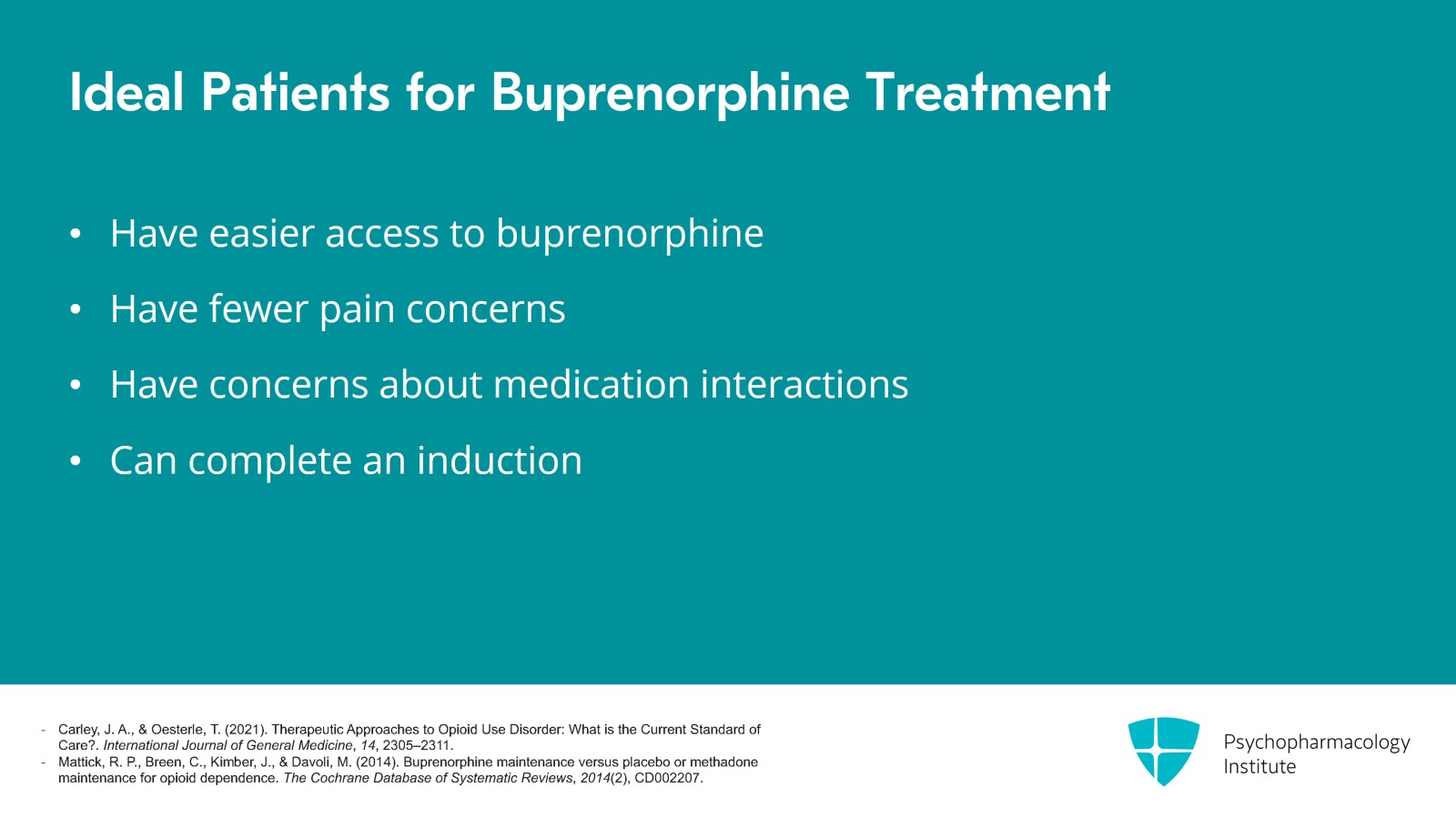
Slide 8 of 21
For those who have easier access to buprenorphine, have less pain concerns, have concern of many of the medication interactions and are able to complete an induction, buprenorphine may be a better option.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 21
Ultimately, the medication that is most likely to be the best medication for a patient is the one that they are most likely to take.
References:
- Carley, J. A., & Oesterle, T. (2021). Therapeutic Approaches to Opioid Use Disorder: What is the Current Standard of Care?. International Journal of General Medicine, 14, 2305–2311.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2014(2), CD002207.
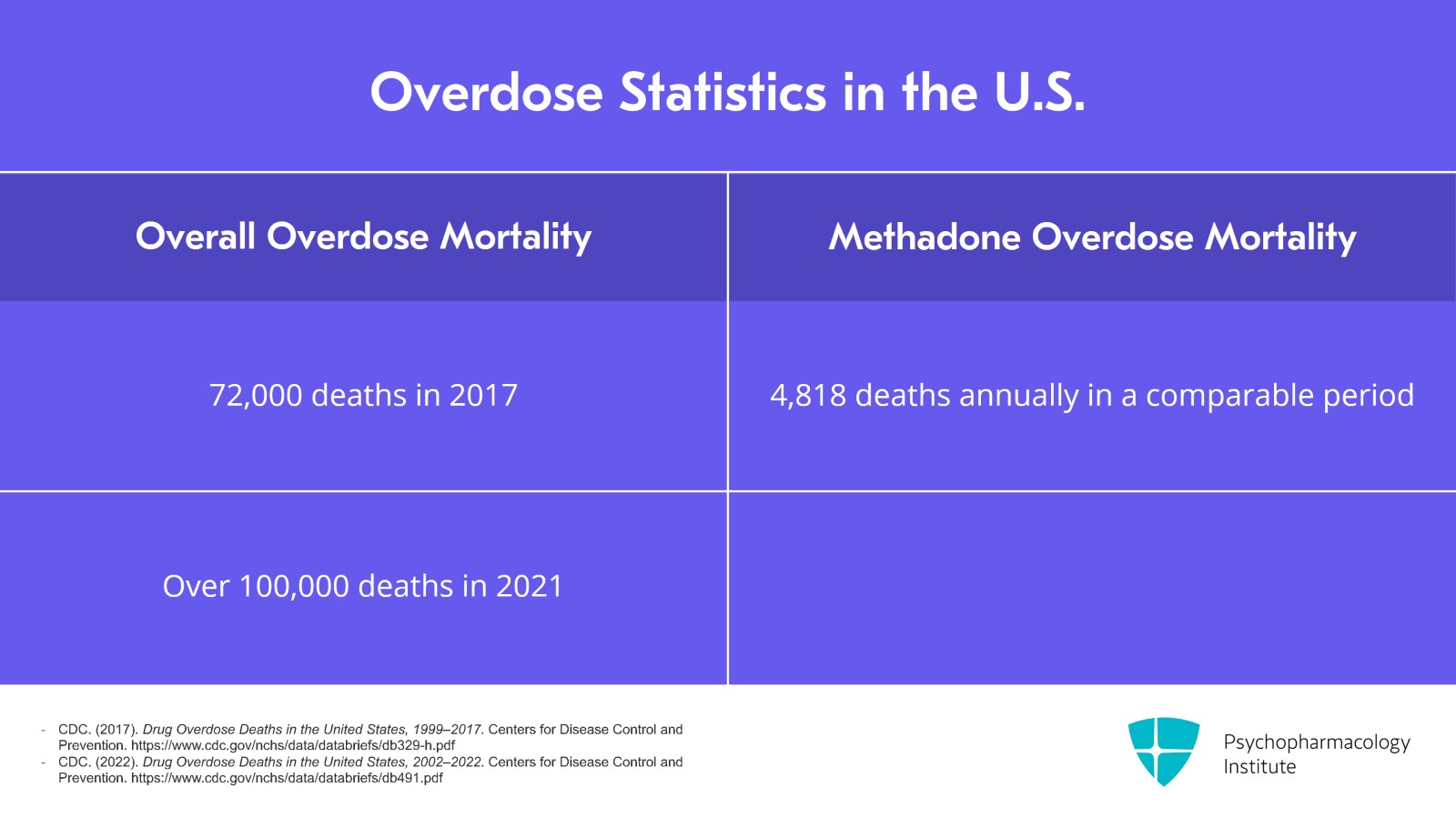
Slide 10 of 21
A concern around starting one of the medications may have to do with overdose risk. There have been 72,000 overdose deaths in 2017 and over 100,000 in 2021 and most of these involve opioids. In terms of US methadone mortality, 4818 annually in a comparable time period. Really, this is 3% prescriptions and 30% mortality.
References:
- CDC. (2017). Drug Overdose Deaths in the United States, 1999–2017. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/databriefs/db329-h.pdf
- CDC. (2022). Drug Overdose Deaths in the United States, 2002–2022. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/databriefs/db491.pdf
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
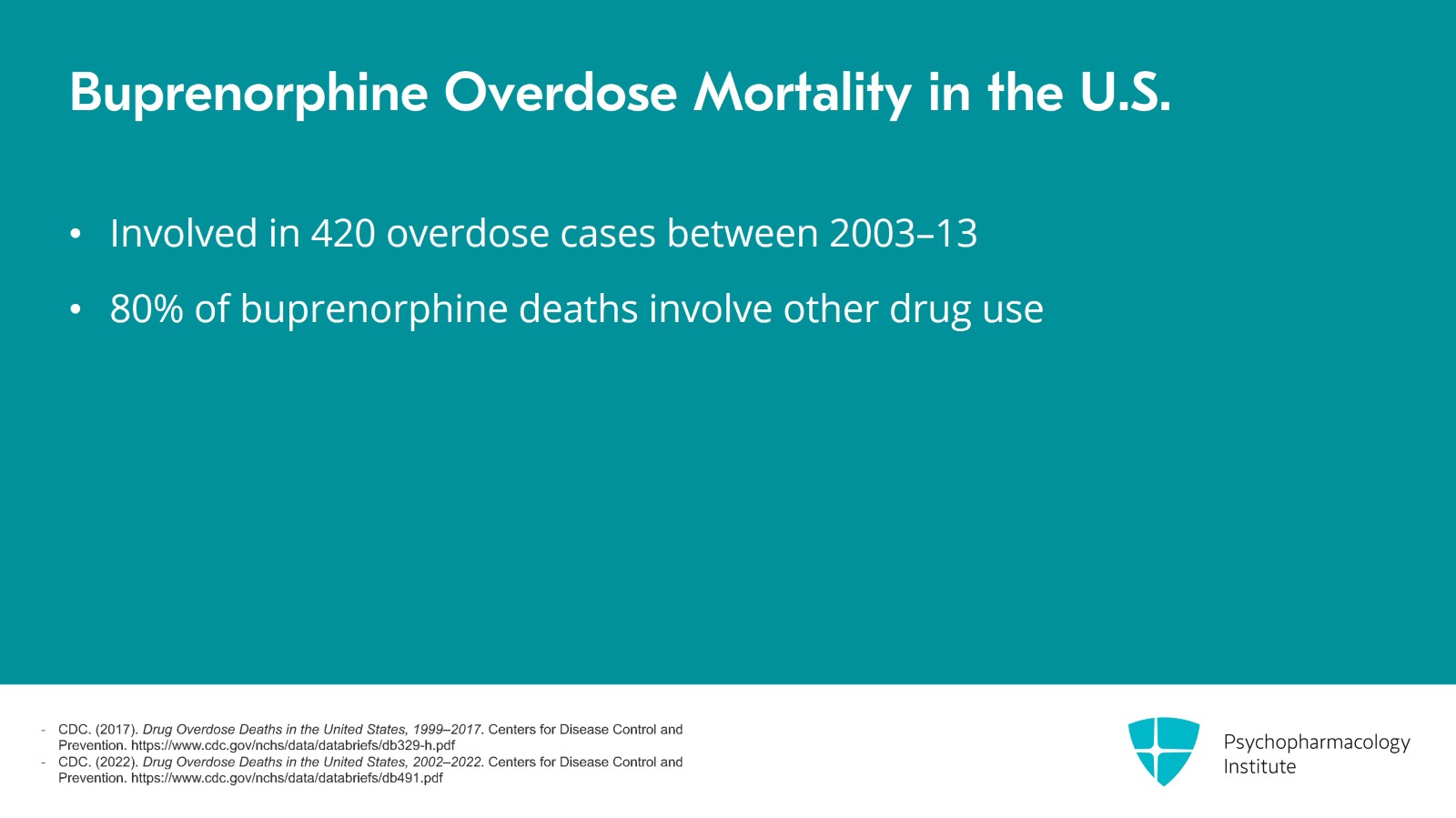
Slide 11 of 21
Buprenorphine is the primary suspect in only 420 overdose cases between 2003 and 2013. This is just 42 annually. It is estimated that 80% of buprenorphine deaths involve some other drug use or mixing with benzodiazepines versus overdosing from buprenorphine alone.
References:
- CDC. (2017). Drug Overdose Deaths in the United States, 1999–2017. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/databriefs/db329-h.pdf
- CDC. (2022). Drug Overdose Deaths in the United States, 2002–2022. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/databriefs/db491.pdf
Slide 12 of 21
Finally, it's important to note that while there is some data around possible methadone or buprenorphine involved overdose deaths, the risk of overdose due to not being on one of these medications is much higher.
References:
- Marteau, D., McDonald, R., & Patel, K. (2015). The relative risk of fatal poisoning by methadone or buprenorphine within the wider population of England and Wales. BMJ Open, 5(5), e007629.
- Bell, J. R., Butler, B., Lawrance, A., Batey, R., & Salmelainen, P. (2009). Comparing overdose mortality associated with methadone and buprenorphine treatment. Drug and Alcohol Dependence, 104(1-2), 73–77.
- CDC. (2022). Drug Overdose Deaths in the United States, 2002–2022. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/databriefs/db491.pdf
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 21
A special population that may be important in pointing out when discussing the different options is expectant mothers. The Maternal Opioid Treatment: Human Experimental Research or MOTHER study was an important study of 175 pregnant women randomized to methadone or buprenorphine. It found that retention was 18% with methadone and 33% with buprenorphine. Children delivered to mothers who were on buprenorphine required less morphine, shorter hospital stays and shorter duration of treatment. There was no difference in other outcomes such as head circumference, number of neonates requiring treatment and adverse events.
References:
- Jones, H. E., Fischer, G., Heil, S. H., Kaltenbach, K., Martin, P. R., Coyle, M. G., Selby, P., Stine, S. M., O'Grady, K. E., & Arria, A. M. (2012). Maternal Opioid Treatment: Human Experimental Research (MOTHER)–approach, issues and lessons learned. Addiction, 107 Suppl 1(0 1), 28–35.
Slide 14 of 21
The study concluded that buprenorphine is an acceptable treatment for pregnant women and notes that this is buprenorphine only, not buprenorphine combined with naloxone. Also note that leaving OUD or opioid use disorder untreated in pregnant women can worsen many outcomes.
References:
- Jones, H. E., Fischer, G., Heil, S. H., Kaltenbach, K., Martin, P. R., Coyle, M. G., Selby, P., Stine, S. M., O'Grady, K. E., & Arria, A. M. (2012). Maternal Opioid Treatment: Human Experimental Research (MOTHER)–approach, issues and lessons learned. Addiction, 107 Suppl 1(0 1), 28–35.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 21
With respect to buprenorphine versus long-acting naltrexone in the general population, the most notable study is a 24-week open-label randomized controlled trial in Norway of 570 patients. They found that while harder to start people on long-acting naltrexone since they will have to be off opioids, once on the medications both were similar in terms of opioid use and craving outcomes.
References:
- Lee, J. D., Nunes, E. V., Jr, Novo, P., Bachrach, K., Bailey, G. L., Bhatt, S., Farkas, S., Fishman, M., Gauthier, P., Hodgkins, C. C., King, J., Lindblad, R., Liu, D., Matthews, A. G., May, J., Peavy, K. M., Ross, S., Salazar, D., Schkolnik, P., Shmueli-Blumberg, D., … Rotrosen, J. (2018). Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): A multicentre, open-label, randomised controlled trial. Lancet, 391(10118), 309–318.
Slide 16 of 21
To summarize with key points, both methadone and buprenorphine are very effective medications. Outcomes including retention efficacy for opioid use disorder are similar. Individual patient characteristics and needs will help determine which medication is best.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 21
For patients who need more structure, may have pain or have done well with methadone in the past or who are not able to be induced because they will need to go into some opioid withdrawal, methadone may be a good choice.
Slide 18 of 21
For people who have difficulty accessing a methadone clinic, would benefit from the ceiling effect on overdose or are using other substances, buprenorphine may be a good option.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 21
Finally, people with safety sensitive positions that prevent them from using an opioid medication may benefit from injectable naltrexone. Injectable naltrexone is very efficacious if somebody is able to go through complete withdrawal and be started on it.
Slide 20 of 21
Finally, both methadone and buprenorphine are recommended in pregnant people with opioid use disorder with buprenorphine having a slightly better profile. Ultimately, the best medication for somebody's opioid use disorder is the medication that they will remain on.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.