Slides and Transcript
Slide 1 of 12
Because stimulants are classified as schedule 2 drugs by the DEA, many prescribers approach the prescribing of stimulants with much trepidation. Because of their potential abusability, they are on schedule 2. This is due to the subjective effects similar to cocaine, significant reinforcement or drug-seeking effects in both animals and human beings.
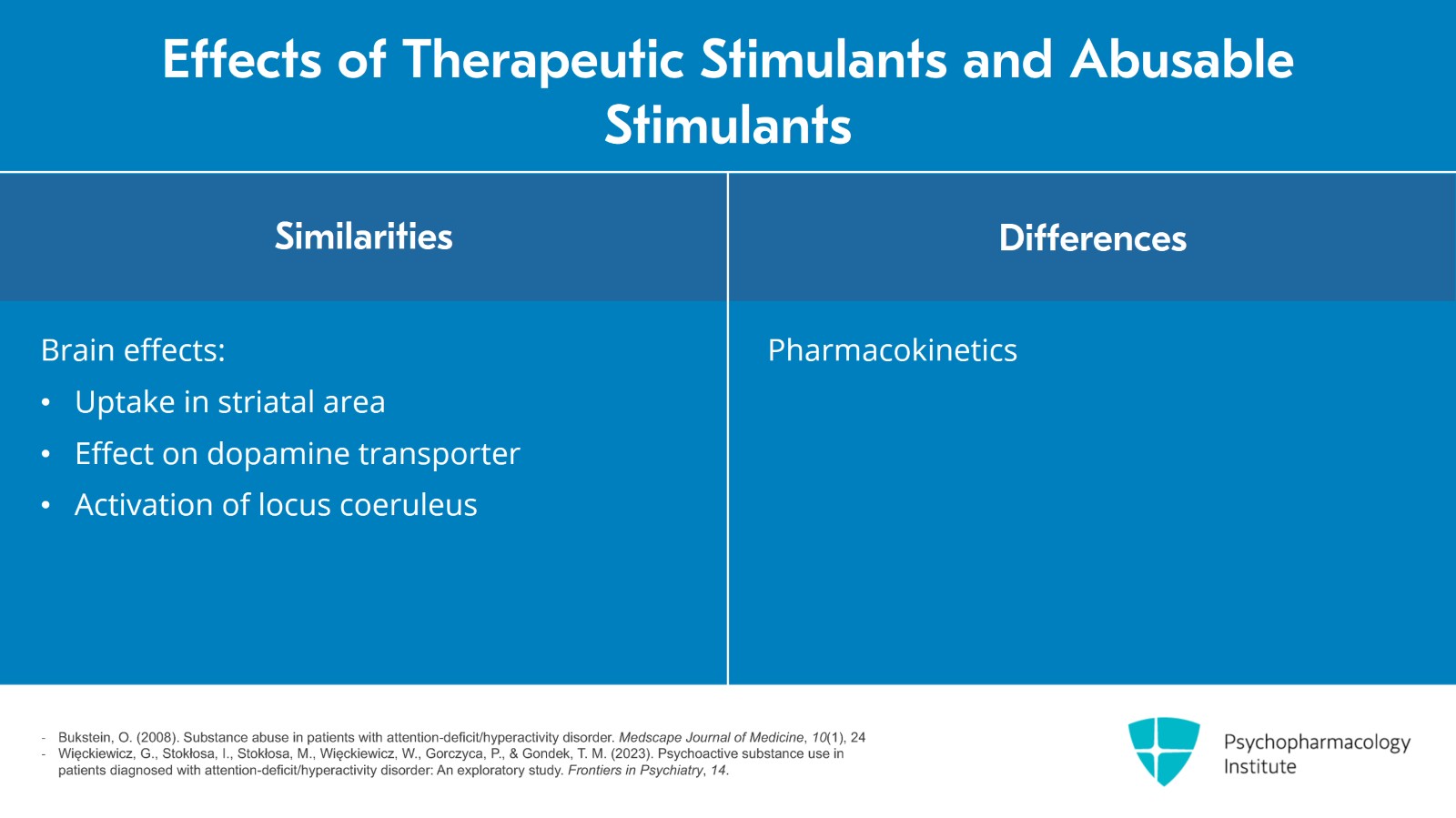
Slide 2 of 12
In many ways, therapeutic stimulants are similar to abusable stimulants such as cocaine in terms of their brain effects, that is their uptake in the striatal area of the brain, their effects on dopamine transporter and activation of the locus coeruleus. However, there are some differences in the pharmacokinetics of stimulants or therapeutic stimulants. For example, methylphenidate clears more slowly than cocaine despite similar rapid uptake and probably prevents an adaptation process.
References:
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
- Więckiewicz, G., Stokłosa, I., Stokłosa, M., Więckiewicz, W., Gorczyca, P., & Gondek, T. M. (2023). Psychoactive substance use in patients diagnosed with attention-deficit/hyperactivity disorder: An exploratory study. Frontiers in Psychiatry, 14.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 12
Well, what are clinical considerations to avoid diversion, abuse or addiction?
Well, there are several obvious questions. You know, is the patient a current drug abuser or past substance abuser? Is there a period of abstinence? Is there ongoing substance use disorder treatment or a history of substance use disorder treatment?
Specifically, about the type of substance use or use disorder, it is very important to determine whether they might have a history of stimulant or amphetamine abuse. That is, are individuals who might be considered at much higher risk for abuse of therapeutic stimulants?
Now, of course, you need to look past at their reasons for use. Many individuals have misused therapeutic stimulants in the past, that is taking stimulants that were not prescribed for them in college but not necessarily for recreational use. It might have been to get work done, to produce better in school or on the job.
References:
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
- Więckiewicz, G., Stokłosa, I., Stokłosa, M., Więckiewicz, W., Gorczyca, P., & Gondek, T. M. (2023). Psychoactive substance use in patients diagnosed with attention-deficit/hyperactivity disorder: An exploratory study. Frontiers in Psychiatry, 14.
Slide 4 of 12
It’s important for the prescriber to have much insight and understanding that there is a danger with stimulants, that they can be used with other stimulants, that there are interactions with other stimulant drugs. They should be aware of the contraindications and precautions of using stimulants and, of course, the risk of cardiovascular problems.
References:
- Holt, A., Strange, J. E., Rasmussen, P. V., Nouhravesh, N., Nielsen, S. K., Sindet-Pedersen, C., Fosbøl, E. L., Køber, L., Torp-Pedersen, C., Gislason, G. H., McGettigan, P., Schou, M., & Lamberts, M. (2024). Long-term cardiovascular risk associated with treatment of attention-deficit/hyperactivity disorder in adults. Journal of the American College of Cardiology, 83(19), 1870–1882.
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
There are precautions that prescribers can take when prescribing medications with abuse potential for individuals with substance use disorder or a past history of substance use disorders. These kinds of behaviors including keeping track of pills or when pills were prescribed, even obtaining urine drug screens or other toxicology screens regularly and more frequent patient visits.
References:
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
Slide 6 of 12
The use of long-acting stimulant medications, avoid allowing the individual to take stimulant medications on an as-needed basis and, finally, a discussion with patients and this includes patients with or without substance use problems regarding safe storage and not advertising that they’re taking stimulant medications. This is particularly important for college students with whom roommates and their friends might be tempted to borrow medication.
References:
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
There are a number of red flags for diversion or misuse. These include calls for emergency supplies of stimulants, that someone has run out prior to the expected expiration of a particular prescription, continued evidence of substance use or substance use disorder, demands for immediate-release compounds which may have a higher abuse potential as well as lost prescriptions and escalating doses.
References:
- Substance Abuse and Mental Health Services Administration (US). (1999). Treatment for stimulant use disorders: Updated 2021 (Treatment Improvement Protocol (TIP) Series, No. 33). Rockville, MD: Author. Chapter 3—Medical aspects of stimulant use disorders. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK576550/
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
Slide 8 of 12
Symptoms indicating higher dose such as psychosis and, finally, signs of overdose or supratherapeutic dosing indicated by palpitations, syncope or shortness of breath.
References:
- Substance Abuse and Mental Health Services Administration (US). (1999). Treatment for stimulant use disorders: Updated 2021 (Treatment Improvement Protocol (TIP) Series, No. 33). Rockville, MD: Author. Chapter 3—Medical aspects of stimulant use disorders. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK576550/
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
It’s important that the prescriber communicate with their patients about the risk of these agents, about what precautions they need to take to make sure that these medications aren’t diverted or stolen by others.
And of course, prescribers need to be aware of these issues as well so that they may take precautions.
References:
- Substance Abuse and Mental Health Services Administration (US). (1999). Treatment for stimulant use disorders: Updated 2021 (Treatment Improvement Protocol (TIP) Series, No. 33). Rockville, MD: Author. Chapter 3—Medical aspects of stimulant use disorders. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK576550/
- Bukstein, O. (2008). Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape Journal of Medicine, 10(1), 24
Slide 10 of 12
Key points in this section include: A screen for the history of current substance use or substance use disorder is very important prior to prescribing for individuals having a risk for substance use problems.
Use precautions to prevent or reduce abuse and diversion. Being aware of red flags suggest a possible abuse or diversion.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
Communication of the expectation of a patient’s behavior regarding therapeutic use of stimulants is very important.
In those cases where stimulants are deemed a little too risky for the specific provider, they can use non-stimulants such as atomoxetine, viloxazine or bupropion rather than stimulant medications.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.