Slides and Transcript
Slide 1 of 25
Now, we’re going to move on to talking about specific medication classes and considerations when prescribing in geriatric populations. And we’ll start first talking about antidepressants.
Slide 2 of 25
So our general prescribing consideration or mantra for older adults is start low, go slow but don’t stop particularly in anxious patients.
References:
- Pretorius, R. W., Gataric, G., Swedlund, S. K., & Miller, J. R. (2013). Reducing the risk of adverse drug events in older adults. American Family Physician, 87(5), 331–336.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 25
For start low, generally the starting dose of antidepressants is going to be about a quarter to half of the usual starting dose for younger adults. So an example of that could be for escitalopram or Lexapro, we would start at doses of 2.5 mg and then titrate upwards. Go slow, so if minimal improvement, we want to make sure that we’re continuing to titrate up the dose but don’t stop. We really want to treat to symptom resolution and remission, and many patients will still need kind of therapeutic doses of the medication. And lastly, be patient. We know that these medications can take time to kick in and it can take 8 to 12 weeks for these antidepressants to be fully effective.
References:
- Pretorius, R. W., Gataric, G., Swedlund, S. K., & Miller, J. R. (2013). Reducing the risk of adverse drug events in older adults. American Family Physician, 87(5), 331–336.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Slide 4 of 25
It’s really important to explain the anticipated time to benefit for medications so patients don’t become frustrated. One of the things I’m really trying to avoid in my clinical work is a patient taking an antidepressant for a week or two, and then stopping ’cause they didn’t notice a benefit and then waiting until that next clinic visit to tell me. I think it’s really important to help people understand that it does take time for these medications to kick in, and that they need to be patient while the medications are starting to work and getting titrated up.
References:
- Pretorius, R. W., Gataric, G., Swedlund, S. K., & Miller, J. R. (2013). Reducing the risk of adverse drug events in older adults. American Family Physician, 87(5), 331–336.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 25
It can also be helpful to provide psychoeducation on coping skills and strategies to behaviorally manage symptoms. This is where referrals to individual or group psychotherapy can be very helpful.
References:
- Pretorius, R. W., Gataric, G., Swedlund, S. K., & Miller, J. R. (2013). Reducing the risk of adverse drug events in older adults. American Family Physician, 87(5), 331–336.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Slide 6 of 25
I’m rarely using other medications such as benzodiazepines, hydroxyzine, gabapentin to bridge unless absolutely necessary. And this would be in specific cases of patients maybe with psychotic depression or really bad anxious depression.
References:
- Pretorius, R. W., Gataric, G., Swedlund, S. K., & Miller, J. R. (2013). Reducing the risk of adverse drug events in older adults. American Family Physician, 87(5), 331–336.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 25
When we think about first-line antidepressants in older adults, generally selective serotonin reuptake inhibitors or SSRIs are going to be our first-line treatment. And we generally choose these medications because they tend to be safer in overdose and have a relatively benign side effect profile.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Slide 8 of 25
In terms of the most common side effects that we see, there are a lot of serotonergic receptors in our brain. There’s also a lot of serotonergic receptors in our GI tract. So GI upset, nausea, vomiting, upset stomach, those tend to be the most common side effects that we see. However, those can be transient. And sometimes, sticking on the medication or taking the medication with food can help.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391(10128), 1357-1366. https://doi.org/10.1016/S0140-6736(17)32802-7
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 25
Headaches can be an issue, sexual side effects. I think sometimes there can be stigma that sexual health is not as important to older adults but mentioning the sexual side effects and following up to make sure that patients feel comfortable kind of reporting any side effects that they might have.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
- Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391(10128), 1357-1366. https://doi.org/10.1016/S0140-6736(17)32802-7
Slide 10 of 25
Hyponatremia is something that as a class can happen with these medications. In general, I like to see at least some previous documentation of a sodium level. And if anyone has a known history of hyponatremia, I would follow that moving forward. Or patients who become confused or have altered mental status once starting an antidepressant, I would be checking a basic metabolic panel to assess their sodium level.
References:
- Jacob, S., & Spinler, S. A. (2006). Hyponatremia associated with selective serotonin-reuptake inhibitors in older adults. Annals of Pharmacotherapy, 40(9), 1618-1622. https://doi.org/10.1345/aph.1G293
- Gheysens, T., Van Den Eede, F., & De Picker, L. (2024). The risk of antidepressant-induced hyponatremia: A meta-analysis of antidepressant classes and compounds. European Psychiatry: The Journal of the Association of European Psychiatrists, 67(1), e20. https://doi.org/10.1192/j.eurpsy.2024.11
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 25
Antidepressants can act synergistically with other medications that increase bleeding risk, and there are also antiplatelet effects and serotonin receptors on platelets. So bleeding risk for patients who are also on NSAIDs, aspirin, warfarin, that’s something that you need to think about.
References:
- Edinoff, A. N., Raveendran, K., Colon, M. A., Thomas, B. H., Trettin, K. A., Hunt, G. W., Kaye, A. M., Cornett, E. M., & Kaye, A. D. (2022). Selective serotonin reuptake inhibitors and associated bleeding risks: A narrative and clinical review. Health Psychology Research, 10(4), 39580. https://doi.org/10.52965/001c.39580
Slide 12 of 25
As a class, antidepressants might be associated with an increased fall risk. Generally, that tends to be when folks are first initiating the medication or titrating up the dose. I think about it as more of a concern for medications that have alpha blockade and can lead to postural hypotension. But as a class, we know that these medications can be associated with that. And the medications can be associated with some weight gain as well.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- van Poelgeest, E. P., Pronk, A. C., Rhebergen, D., & van der Velde, N. (2021). Depression, antidepressants and fall risk: therapeutic dilemmas-a clinical review. European Geriatric Medicine, 12(3), 585–596. https://doi.org/10.1007/s41999-021-00475-7
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 25
In terms of the most common antidepressants that we prescribe for older adults, generally it’s going to be one of these top three – so sertraline, citalopram and escitalopram. Generally, we’ll choose those medications because they have relatively limited drug-drug interactions, and tend to have a little bit less of some of those side effects that we talked about. Again, we’re going to start on the lower range of things and then titrate upwards as tolerated.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391(10128), 1357-1366. https://doi.org/10.1016/S0140-6736(17)32802-7
Slide 14 of 25
A few pearls I’ll mention just where we might consider prescribing a little bit differently than our average adult population. Paroxetine or Paxil is a medication that generally I try to avoid prescribing in older adults. And the reason for that is that it is anticholinergic, so it can lead to side effects like constipation, urinary retention, confusion. It’s also both a substrate and an inhibitor of the CYP2D6 pathway, and so can have more drug-drug interactions. It also has a very short half-life. So if people stop the medication abruptly, it can lead to a bad discontinuation syndrome.
References:
- Chew, M. L., Mulsant, B. H., Pollock, B. G., Lehman, M. E., Greenspan, A., Mahmoud, R. A., Kirshner, M. A., Sorisio, D. A., Bies, R. R., & Gharabawi, G. (2008). Anticholinergic activity of 107 medications commonly used by older adults. Journal of the American Geriatrics Society, 56(7), 1333-1341. https://doi.org/10.1111/j.1532-5415.2008.01737.x
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 25
Fluoxetine or Prozac, that’s a medication that also has some CYP2D6 inhibition, so more drug-drug interactions. I’m probably less inclined to prescribe that medication for older adults.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Chew, M. L., Mulsant, B. H., Pollock, B. G., Lehman, M. E., Greenspan, A., Mahmoud, R. A., Kirshner, M. A., Sorisio, D. A., Bies, R. R., & Gharabawi, G. (2008). Anticholinergic activity of 107 medications commonly used by older adults. Journal of the American Geriatrics Society, 56(7), 1333-1341. https://doi.org/10.1111/j.1532-5415.2008.01737.x
Slide 16 of 25
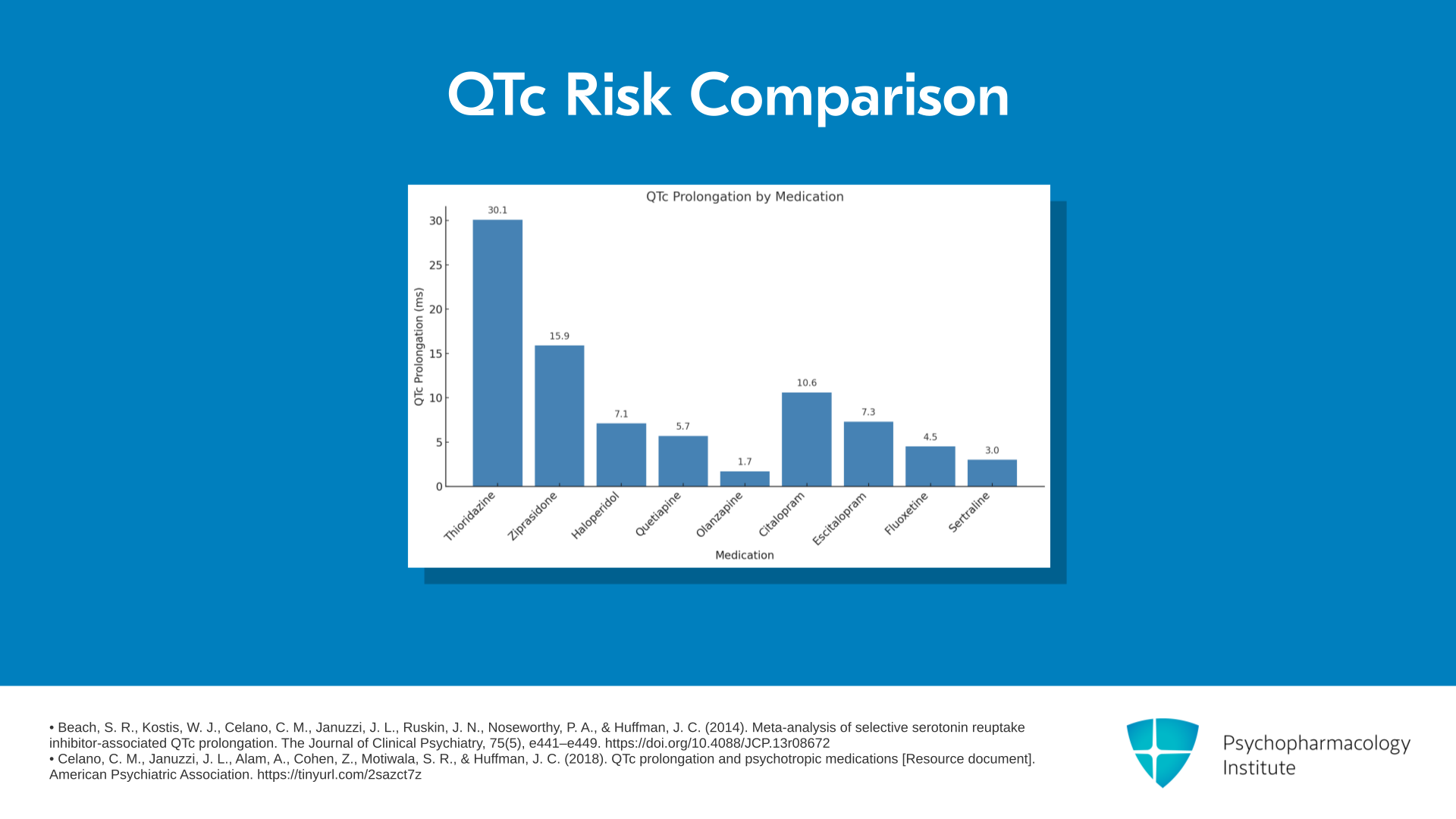
Citalopram. I’ll just make a mention of the 2011 FDA warning that was specific for citalopram, that talked about dose-dependent increases in the QT interval. And when you look across those studies, it’s generally about somewhere in the range of 10 to 12 msec that the QT can be prolonged. However, because of the recommended EKG monitoring and discussion of the risk-benefit profile with patients, it’s probably a little less widely prescribed in the United States than it was before that FDA warning. How I think about it is that if you have a patient with a baseline normal QT interval, if their QT interval goes up by 12 seconds in a normal QTc, probably not that big of a deal. For someone who has a history of prolonged QT interval, this may not be a medication that you’d like to start first line.
References:
- Beach, S. R., Kostis, W. J., Celano, C. M., Januzzi, J. L., Ruskin, J. N., Noseworthy, P. A., & Huffman, J. C. (2014). Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. The Journal of Clinical Psychiatry, 75(5), e441–e449. https://doi.org/10.4088/JCP.13r08672
- U.S. Food and Drug Administration. (2011, August 24). FDA drug safety communication: Abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). FDA Safety Announcement. https://tinyurl.com/3ccwx577
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 25
Escitalopram or Lexapro, the S-enantiomer of citalopram, is probably one of the most widely prescribed antidepressants now. It also can cause dose-dependent increases in the QT interval, but was not flagged with the FDA warning.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Beach, S. R., Kostis, W. J., Celano, C. M., Januzzi, J. L., Ruskin, J. N., Noseworthy, P. A., & Huffman, J. C. (2014). Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. The Journal of Clinical Psychiatry, 75(5), e441–e449. https://doi.org/10.4088/JCP.13r08672
Slide 18 of 25
A few other medications. Vidazolone acts as an SSRI and then also has serotonin receptor partial agonist as well, so it works on a couple of different mechanisms. Vortioxetine is a novel antidepressant with effects on multiple serotonin receptors and on the serotonin transporter. Trazodone or Desyrel is another medication that we often use for treatment of insomnia at lower doses than we would for depression.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Kok, R. M., & Reynolds, C. F., III. (2017). Management of depression in older adults: A review. JAMA, 317(20), 2114-2122. https://doi.org/10.1001/jama.2017.5706
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 25
This graph here shows the relative risk of QTc prolongation across several different psychiatric medications including antipsychotics as well as antidepressants. Again, we can see the relative risk of medications like citalopram and escitalopram as compared to some of the antipsychotic medications like thioridazine and ziprasidone.
References:
- Beach, S. R., Kostis, W. J., Celano, C. M., Januzzi, J. L., Ruskin, J. N., Noseworthy, P. A., & Huffman, J. C. (2014). Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. The Journal of Clinical Psychiatry, 75(5), e441–e449. https://doi.org/10.4088/JCP.13r08672
- Celano, C. M., Januzzi, J. L., Alam, A., Cohen, Z., Motiwala, S. R., & Huffman, J. C. (2018). QTc prolongation and psychotropic medications [Resource document]. American Psychiatric Association. https://tinyurl.com/2sazct7z
Slide 20 of 25
Next, moving on to the SNRIs. So these medications work on both serotonin and norepinephrine and common medications within this class include duloxetine, venlafaxine and desvenlafaxine.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 25
Duloxetine or Cymbalta is a medication that commonly gets used for chronic pain. It’s kind of an add-on as well. And all of these medications have an indication for chronic pain. So if you have a patient with depression, anxiety plus chronic pain, you can sometimes think about two birds, one stone.
References:
- Lunn, M. P., Hughes, R. A., & Wiffen, P. J. (2014). Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. The Cochrane Database of Systematic Reviews, 2014(1), CD007115. https://doi.org/10.1002/14651858.CD007115.pub3
Slide 22 of 25
Venlafaxine or Effexor is another commonly used SNRI. We really need to dose the medication kind of above 150 mg to get both the serotonin and norepinephrine effect. Desvenlafaxine or Pristiq is just the metabolite of venlafaxine, and kind of the shtick with that medication is that you get both the serotonin and norepinephrine effect right at that starting dose.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Harvey, A. T., Rudolph, R. L., & Preskorn, S. H. (2000). Evidence of the dual mechanisms of action of venlafaxine. Archives of General Psychiatry, 57(5), 503-509. https://doi.org/10.1001/archpsyc.57.5.503
- Spoelhof, G. D., Davis, G. L., & Licari, A. (2011). Clinical vignettes in geriatric depression. American Family Physician, 84(10), 1149-1154.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 25
Related to the norepinephrine effects, these medications are all going to be more activating and so these are medications that you really want to dose towards the beginning of the day as not to disrupt sleep at night. Also related to the norepinephrine effect, these are medications that can increase blood pressure, specifically diastolic blood pressure.
References:
- Kovich, H., Kim, W., & Quaste, A. M. (2023). Pharmacologic treatment of depression. American Family Physician, 107(2), 173-181.
- Spoelhof, G. D., Davis, G. L., & Licari, A. (2011). Clinical vignettes in geriatric depression. American Family Physician, 84(10), 1149-1154.
Slide 24 of 25
So key points for this section: Our general mantra of prescribing in Geriatrics is to start low, go slow, but don’t stop and be patient. These medications can take time to kick in. SSRIs are generally first-line treatment for late life depression and anxiety. The most common side effects of SSRIs are GI upset, headache, and sexual side effects.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 25 of 25
Of the SSRIs, generally we’ll avoid using paroxetine in older adults given the anticholinergic properties. The SNRIs are indicated for chronic pain, depression, and anxiety, but related to that norepinephrine effect, we need to watch out for side effects, including activation and increased blood pressure.