Slides and Transcript
Slide 1 of 10
Okay. So what do you do when medications don’t work? In this video, I want to talk more about somatic therapies.
Slide 2 of 10
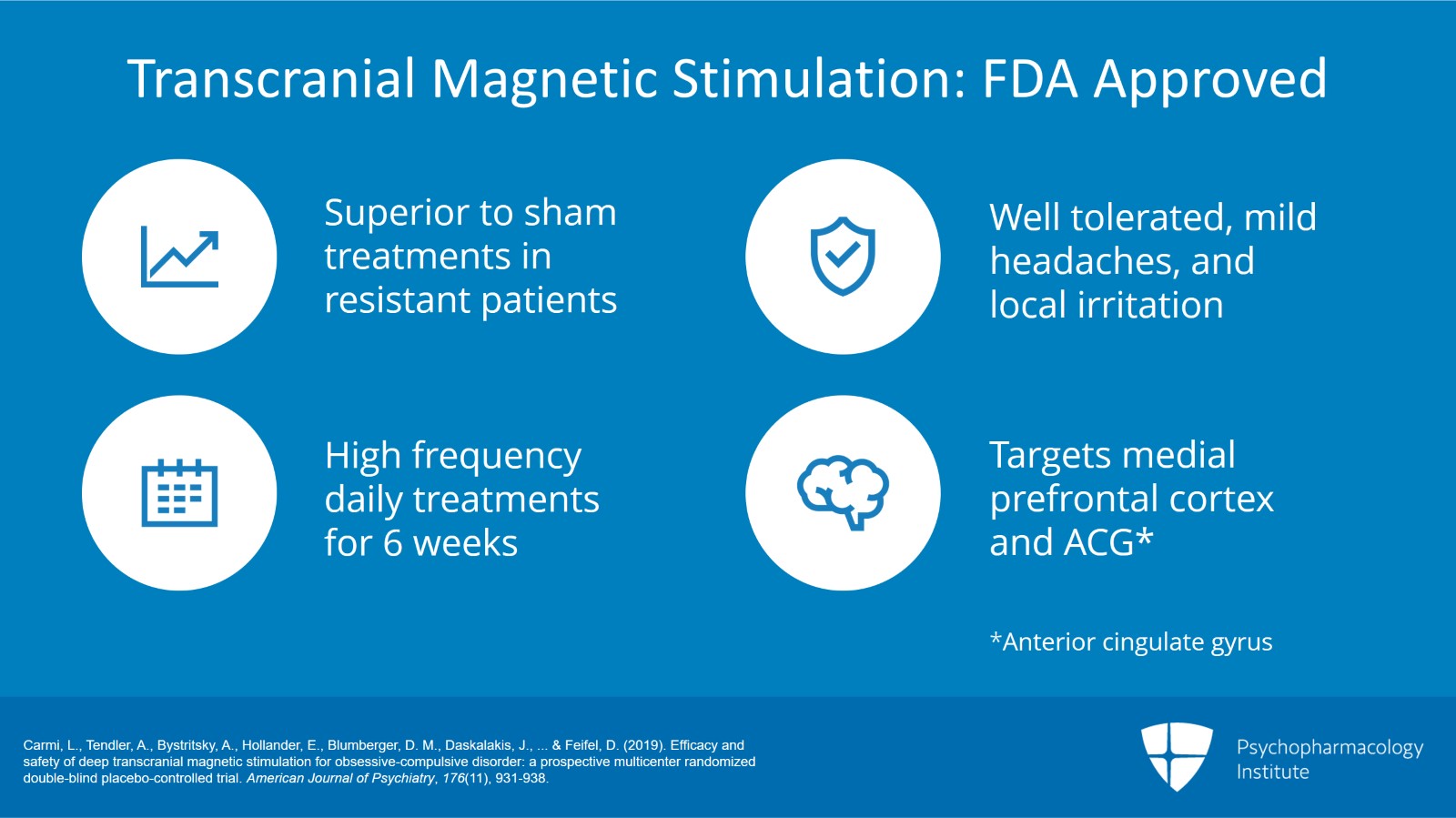
There is one somatic therapy that’s recently been approved by the FDA, transcranial magnetic stimulation. There are some very recent data published in 2019 to show that TMS is superior to placebo or sham treatments in treatment-resistant patients. And this is a big deal.
This is a pretty well-tolerated treatment. There are some side effects to transcranial magnetic stimulation. It can have some mild headache and local irritation. It is FDA approved.
This really requires high frequency daily treatments for six weeks. And in order to do proper TMS for OCD, there’s actually a mini exposure session that is done as part of the ERP. And you’re targeting the medial prefrontal cortex and the ACG in this.
References:
- Carmi, L., Tendler, A., Bystritsky, A., Hollander, E., Blumberger, D. M., Daskalakis, J., … & Feifel, D. (2019). Efficacy and safety of deep transcranial magnetic stimulation for obsessive-compulsive disorder: a prospective multicenter randomized double-blind placebo-controlled trial. American Journal of Psychiatry, 176(11), 931-938.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
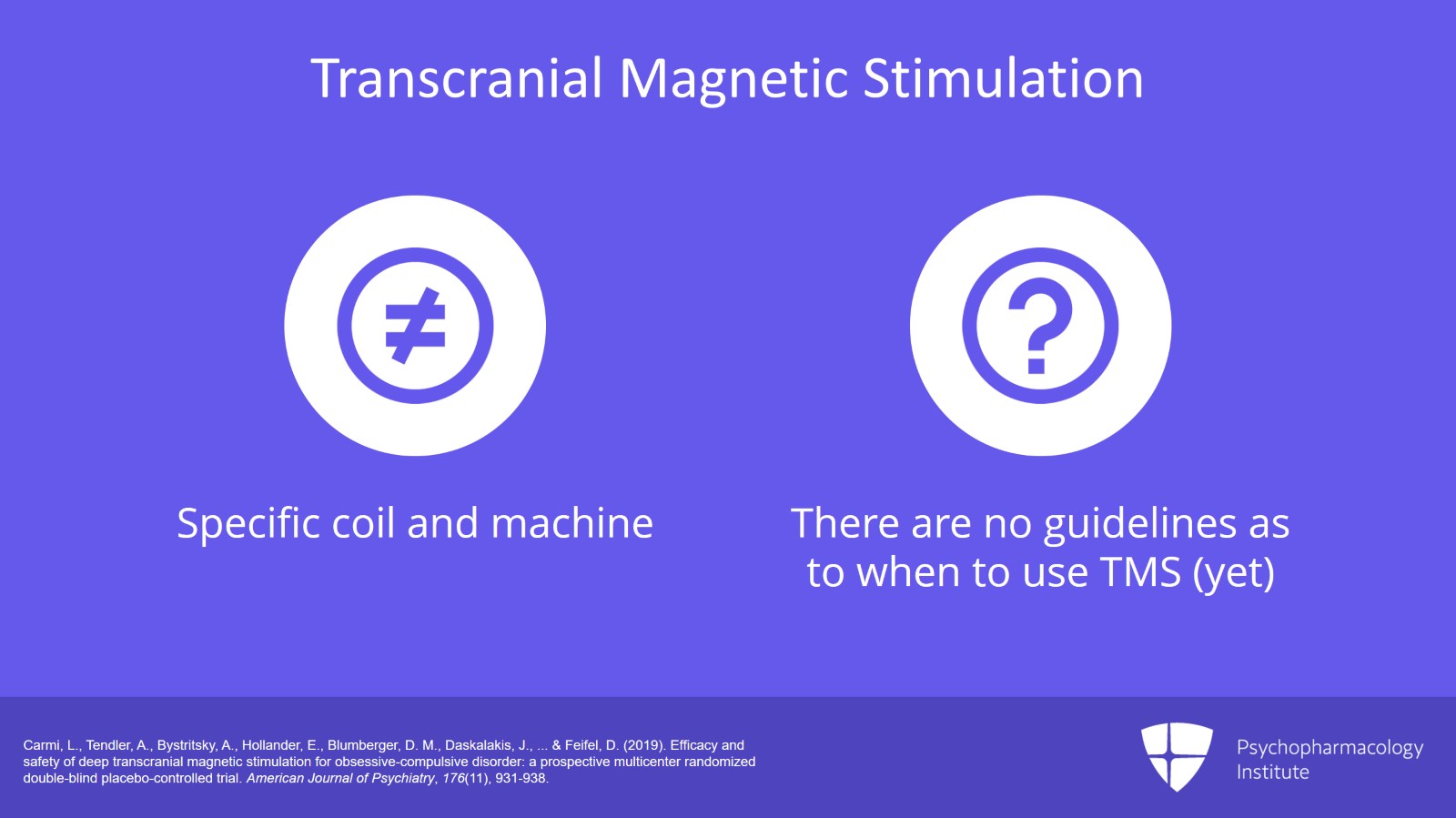
Now, this is very important. The coil that is used for transcranial magnetic stimulation is different than what is used for MDD. So people who have a TMS machine that they use for MDD, this will not work for OCD. It requires a very different coil and a different machine or setup than MDD machine. So just someone who has TMS, you just can’t send your OCD patients to them. They need the right machine. As I said, there’s an exposure-like provocation that’s used during the procedure. So they have to be trained on how to do that.
The only difficulty with TMS right now is there isn’t yet consensus guidelines on where you place it in the OCD treatment algorithm. If you notice, I had the treatment algorithm in other prior videos. I don’t yet have TMS on there. I don’t really know when the proper time to include TMS on the treatment algorithm. I suspect it should be somewhere before using antipsychotic augmentation and maybe even before using polypharmacy or using augmentation at all. But again, it hasn’t been worked out by expert consensus guidelines or by research data. But we do know it works in treatment-resistant patients and this is a big breakthrough.
References:
- Carmi, L., Tendler, A., Bystritsky, A., Hollander, E., Blumberger, D. M., Daskalakis, J., … & Feifel, D. (2019). Efficacy and safety of deep transcranial magnetic stimulation for obsessive-compulsive disorder: a prospective multicenter randomized double-blind placebo-controlled trial. American Journal of Psychiatry, 176(11), 931-938.
Slide 4 of 10
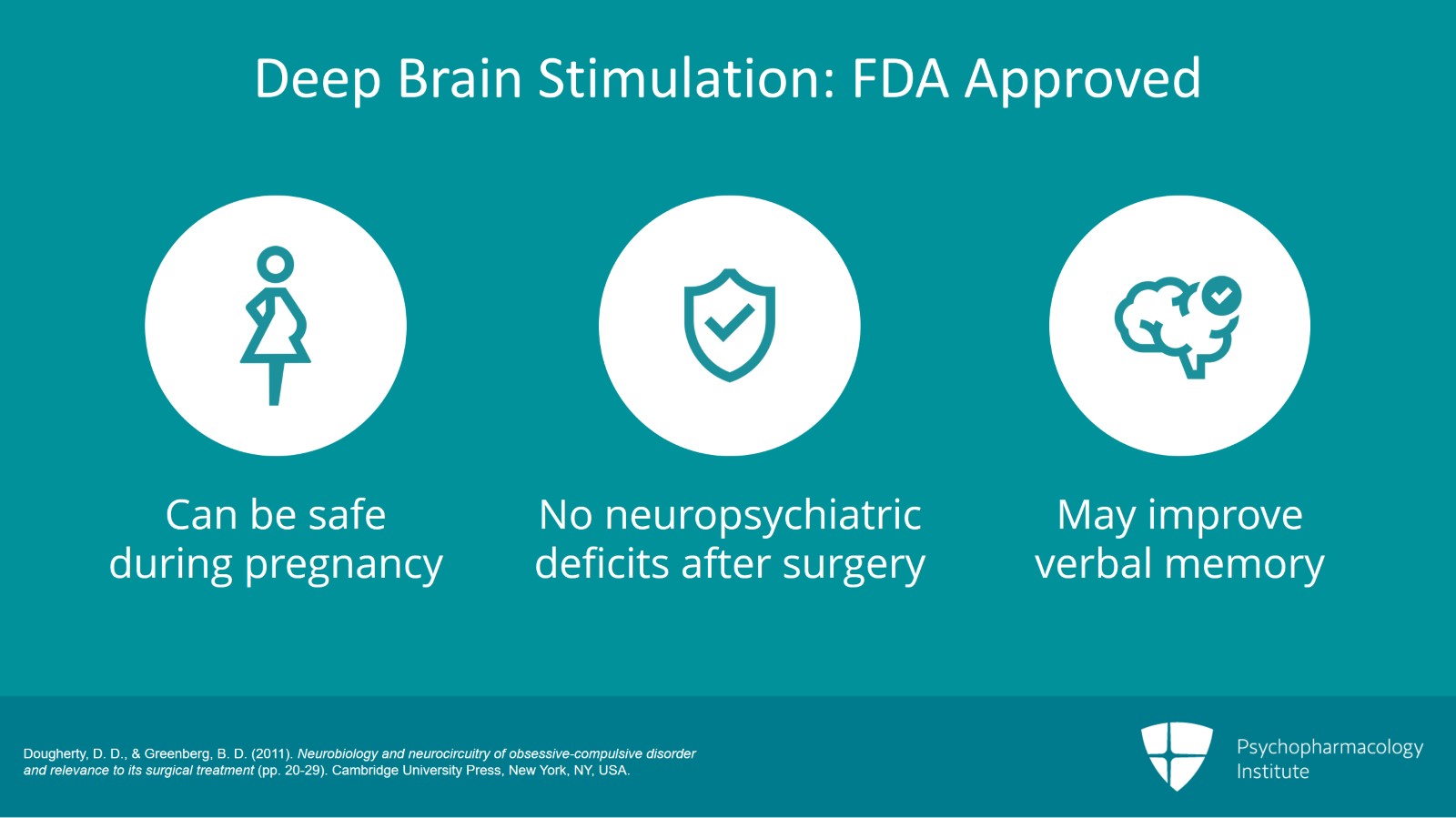
So there is another procedure we can do, deep brain stimulation. So the FDA approved this for a humanitarian device exemption in 2009. So basically, the FDA gave the green light to use deep brain stimulation in patients with OCD. It can be safe in pregnant patients.
The improvement varies according to studies that are done. And interestingly, better results occur with more recent studies. So DBS has been shown to be better the more recently it’s done and that’s simply because of the refinement of the surgical techniques and particularly the targets. As surgeons have evolved their techniques, they know better where to place the electrodes and the leads in the brain and that’s led to better results.
And at this point, there is no noted neuropsychiatric deficits secondary to the surgery. There may even be an improvement in verbal memory.
References:
- Dougherty, D. D., & Greenberg, B. D. (2011). Neurobiology and neurocircuitry of obsessive-compulsive disorder and relevance to its surgical treatment (pp. 20-29). Cambridge University Press, New York, NY, USA.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
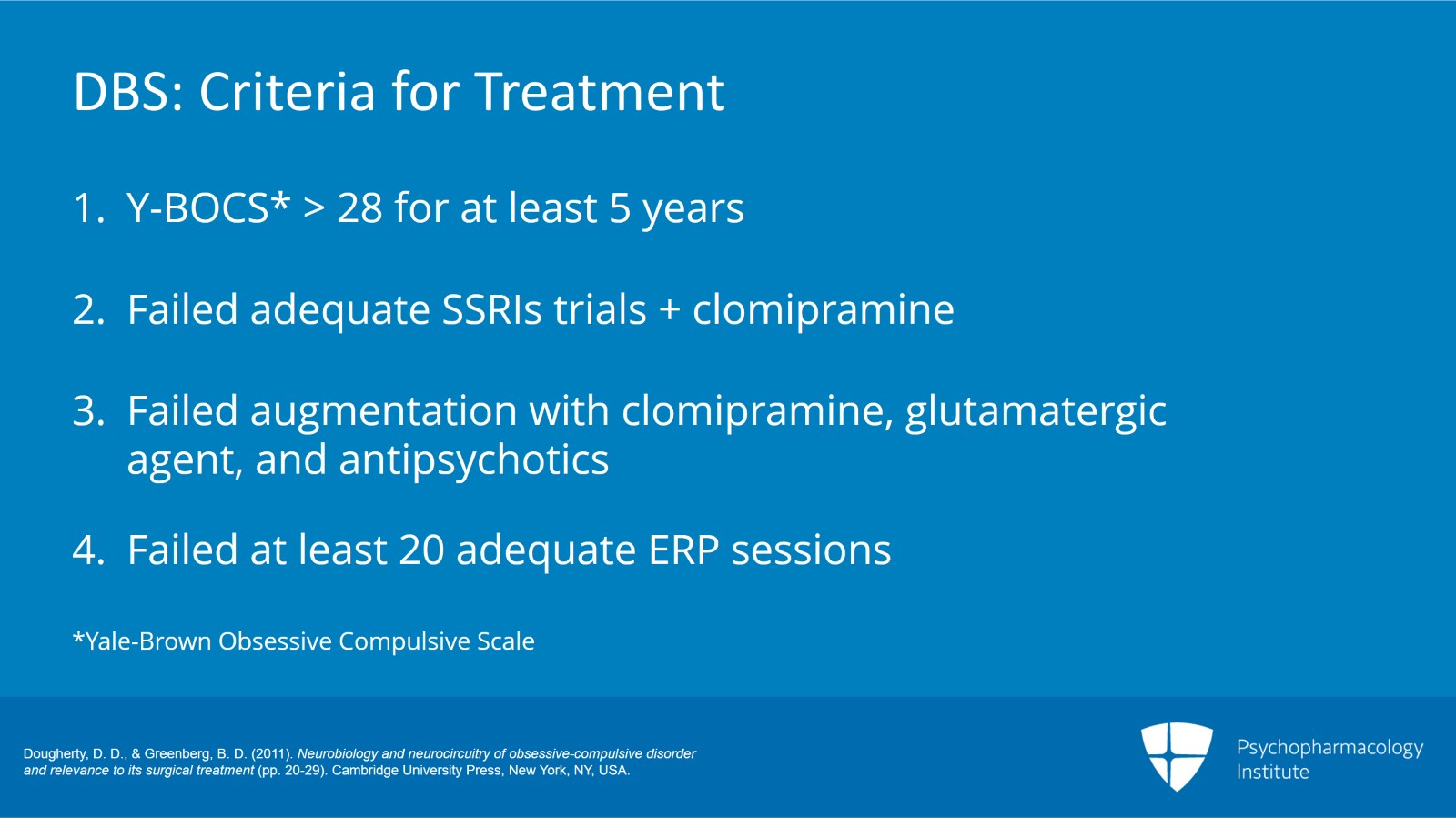
Now, to have DBS, someone needs to meet some very pretty strict criteria for treatment. They have to have a Y-BOCS score of 28 or greater that notifies severe OCD and it has to be for a minimum of a five-year duration.
Their global assessment of functioning has to be 45 or lower.
So in other words, they have to be very impaired by their OCD.
They’ve had to have adequate trial of two SSRIs plus clomipramine, so three SSRIs total.
They have to have failed augmentation with clomipramine, a glutamatergic agent and also an antipsychotic.
The old criteria include a benzodiazepine for that. I’ve mostly gotten rid of that criteria from our DBS program because benzodiazepines are really very rarely used as OCD augmentation anymore. Quite frankly, they don’t work. These augmentations must last at least a month.
So a patient must have failed an augmentation with these medications of at least a one-month duration.
Patient must have also failed a minimum of 20 adequate ERP sessions. And note, specifically, these must be adequate ERP. ERP is not available in many parts of the country. That means in order to be eligible for deep brain stimulation, patients may have to travel to an OCD treatment center in another city.
References:
- Dougherty, D. D., & Greenberg, B. D. (2011). Neurobiology and neurocircuitry of obsessive-compulsive disorder and relevance to its surgical treatment (pp. 20-29). Cambridge University Press, New York, NY, USA.
Slide 6 of 10
There are exclusion criteria. A history of psychosis, bipolar disorder, body dysmorphic disorder or current substance use disorder can disqualify you for deep brain stimulation.
So of the patients that are brought to our attention, patients who are referred to me by psychiatrists who say, we would like a DBS on this patient because the patient is so severe, it’s important to note that less than 1% of those patients meet criteria for deep brain stimulation. In other words, they’ve been inadequately treated. Their treatment resistance is iatrogenic and not because they truly have failed proper OCD protocol. However, that wouldn’t happen to you after you finish these videos. You know OCD treatment protocol that’s proper and you will make sure that you do not have your patients suffer from iatrogenic treatment resistance.
References:
- Greenberg, B. D., Malone, D. A., Friehs, G. M., Rezai, A. R., Kubu, C. S., Malloy, P. F., … & Rasmussen, S. A. (2006). Three-year outcomes in deep brain stimulation for highly resistant obsessive–compulsive disorder. Neuropsychopharmacology, 31(11), 2384-2393.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
Okay. So there was an initial study of 10 subjects of deep brain stimulation. These were patients that were pooled from Mass General, Brown University and the Cleveland Clinic. And they had these inclusion and exclusion criteria as above. And after the device is implanted in the brain, they get stimulation two weeks later.
And they noticed six of eight experienced a 25% reduction in Y-BOCS at 36 months, four of eight experienced a 35% reduction at 36 months. And depression and anxiety scores improved pretty significantly. By three months, depression and anxiety were better in most patients.
References:
- Greenberg, B. D., Malone, D. A., Friehs, G. M., Rezai, A. R., Kubu, C. S., Malloy, P. F., … & Rasmussen, S. A. (2006). Three-year outcomes in deep brain stimulation for highly resistant obsessive–compulsive disorder. Neuropsychopharmacology, 31(11), 2384-2393.
Slide 8 of 10
You can see the adverse events include transient elevated mood. Mania is a possibility here. Epigastric, olfactory, gustatory sensations. One person in this early study had an asymptomatic brain hemorrhage.
We generally like deep brain stimulation, preferred over other older treatments such as cingulotomy because it does not destroy brain tissue.
Ablative techniques, however, such as cingulotomies may be preferred in patients with things like comorbid skin picking disorder or other body-focused repetitive behaviors or in patients with symmetry concerns, worried about having a battery pack on one side of the body.
References:
- Greenberg, B. D., Malone, D. A., Friehs, G. M., Rezai, A. R., Kubu, C. S., Malloy, P. F., … & Rasmussen, S. A. (2006). Three-year outcomes in deep brain stimulation for highly resistant obsessive–compulsive disorder. Neuropsychopharmacology, 31(11), 2384-2393.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
So the key points are: Deep TMS is newly approved for OCD. Best patient selection for these patients, we’re still working on that. The machine, the coil and the procedure are different than the TMS used for major depression. Other surgical techniques such as ablative procedures and DBS may be used in the very most severe and treatment-resistant cases. Generally, this is a very uncommon option. This is not used frequently. And I will tell you as an OCD specialist who’s literally treated thousands of patients in my career, I’ve only had a handful or two of patients that I have referred for surgery.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.