Slides and Transcript
Slide 1 of 9
Okay. In this video, I’m going to talk about augmentation with second-generation antipsychotics as well as ondansetron and other medications.
Slide 2 of 9
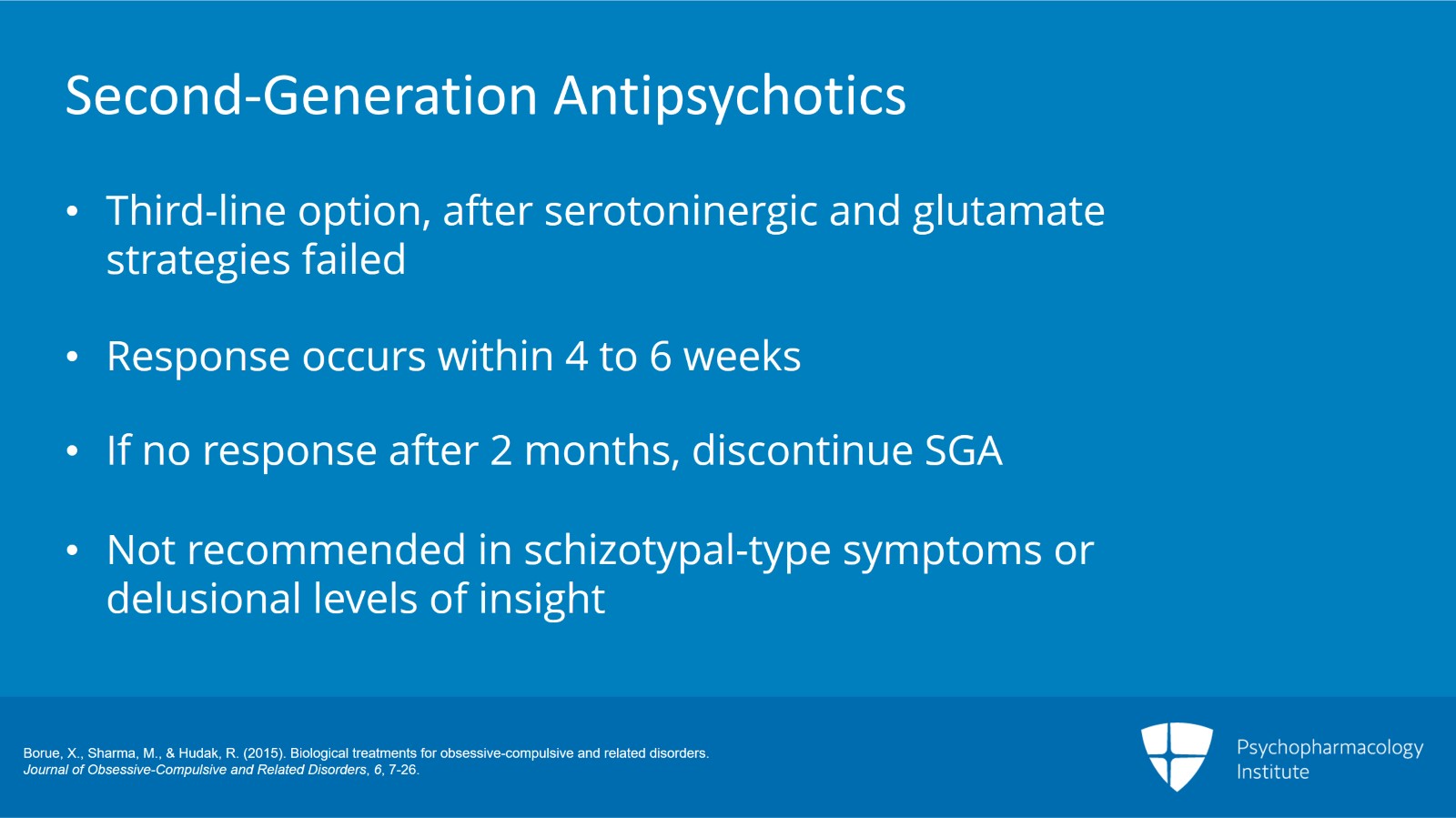
So the second-generation antipsychotics, I consider them to be third-line augmentation only when someone has failed additional serotonergic augmentation as well as has failed glutamatergic augmentation as well. Just so you know, as someone who is an OCD specialist and I treat the most severe OCD patients that there are and I treat hundreds of OCD patients every year, I very rarely initiate antipsychotics on my patients. I rarely see the need to. So it’s not something that I think should be done commonly at this point.
The response to most second-generation antipsychotics usually occurs within the first four to six weeks. So if the patient has not had a significant improvement after two months of being on a second-generation antipsychotic, I recommend stopping the medication at that point. There’s no reason to keep someone on an antipsychotic if they haven’t specifically improved. However, if they do get a response to the second-generation antipsychotic, some patients may relapse if it is discontinued so you have to be aware of that. If they do respond well, they may need to keep taking the medication.
Now, patients who have schizotypal-type symptoms, so some of the unusual obsessions that I talked about in video 1 or patients who have delusional level of insight, antipsychotics are not necessary in those patients. They’re not recommended. There is actually zero evidence that antipsychotics work in any of this type of OCD patients. However, if the patient does have a comorbid tic disorder, there are suggestions that the patient may have an improved response to antipsychotic augmentation.
So again, to reiterate, there are no specific characteristics of OCD that have been identified to relate to response requiring second-generation antipsychotics. So in other words, once you’ve diagnosed someone with OCD, you diagnose them with OCD. It doesn’t matter what kind of OCD symptoms they have. Second-generation antipsychotics wouldn’t be more effective for one type of OCD than another type of OCD.
References:
- Borue, X., Sharma, M., & Hudak, R. (2015). Biological treatments for obsessive-compulsive and related disorders. Journal of Obsessive-Compulsive and Related Disorders, 6, 7-26.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 9
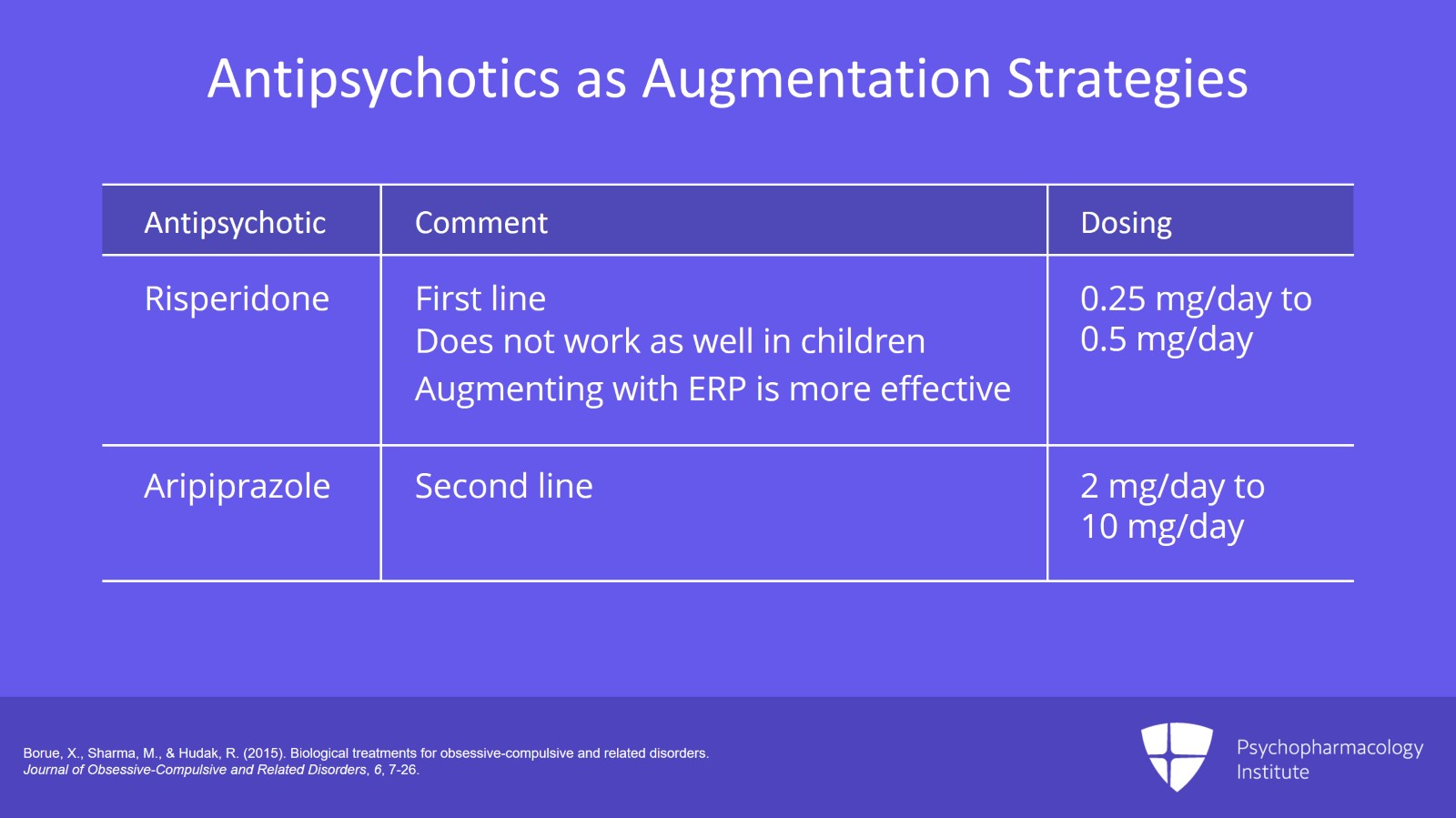
Now, please be aware that second-generation antipsychotics are not a homogenous group of medication. They are really a diverse group of medications that often have very little in common. Therefore, just because one second-generation antipsychotic has an effect on an illness including OCD augmentation does not mean a different one will.
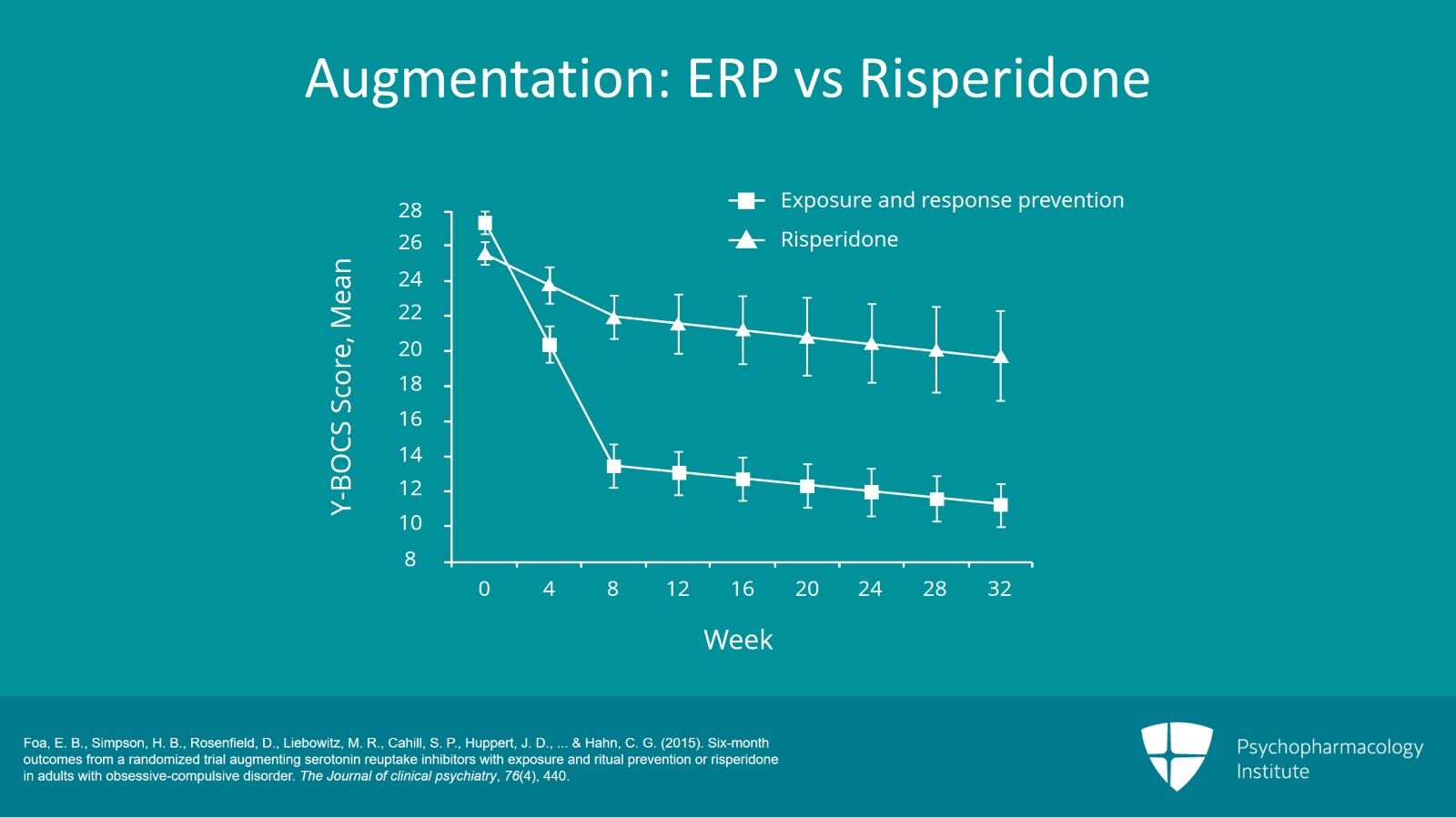
So we know that with risperidone, it’s been effective in three double-blind randomized controlled trials for OCD and it is the antipsychotic that has been studied most for augmentation. Therefore, if you want to choose a second-generation antipsychotic as augmentation, risperidone probably should be the first line of choice. However, there are some caveats to that. It is less studied in children than it is in adults. So we know what works in adults. Maybe it doesn’t work so well in children. Importantly, when you take a look at studies that compare augmentation of SSRIs with ERP and augmentation of SSRIs with risperidone, augmentation with ERP comes out on top every time. So, risperidone is not really some sort of magic augmentation. ERP plus SSRI seems to work better than adding risperidone could work. Note that all second-generation antipsychotics including risperidone has the possibility of exacerbating OCD symptoms.
Now, aripiprazole has been shown to be effective in two double-blind studies. And therefore, I consider that to be a second-line medication augmentation. If you don’t want to use risperidone or you cannot use risperidone, aripiprazole seems to be the second choice of second-generation antipsychotics.
References:
- Borue, X., Sharma, M., & Hudak, R. (2015). Biological treatments for obsessive-compulsive and related disorders. Journal of Obsessive-Compulsive and Related Disorders, 6, 7-26.
Slide 4 of 9
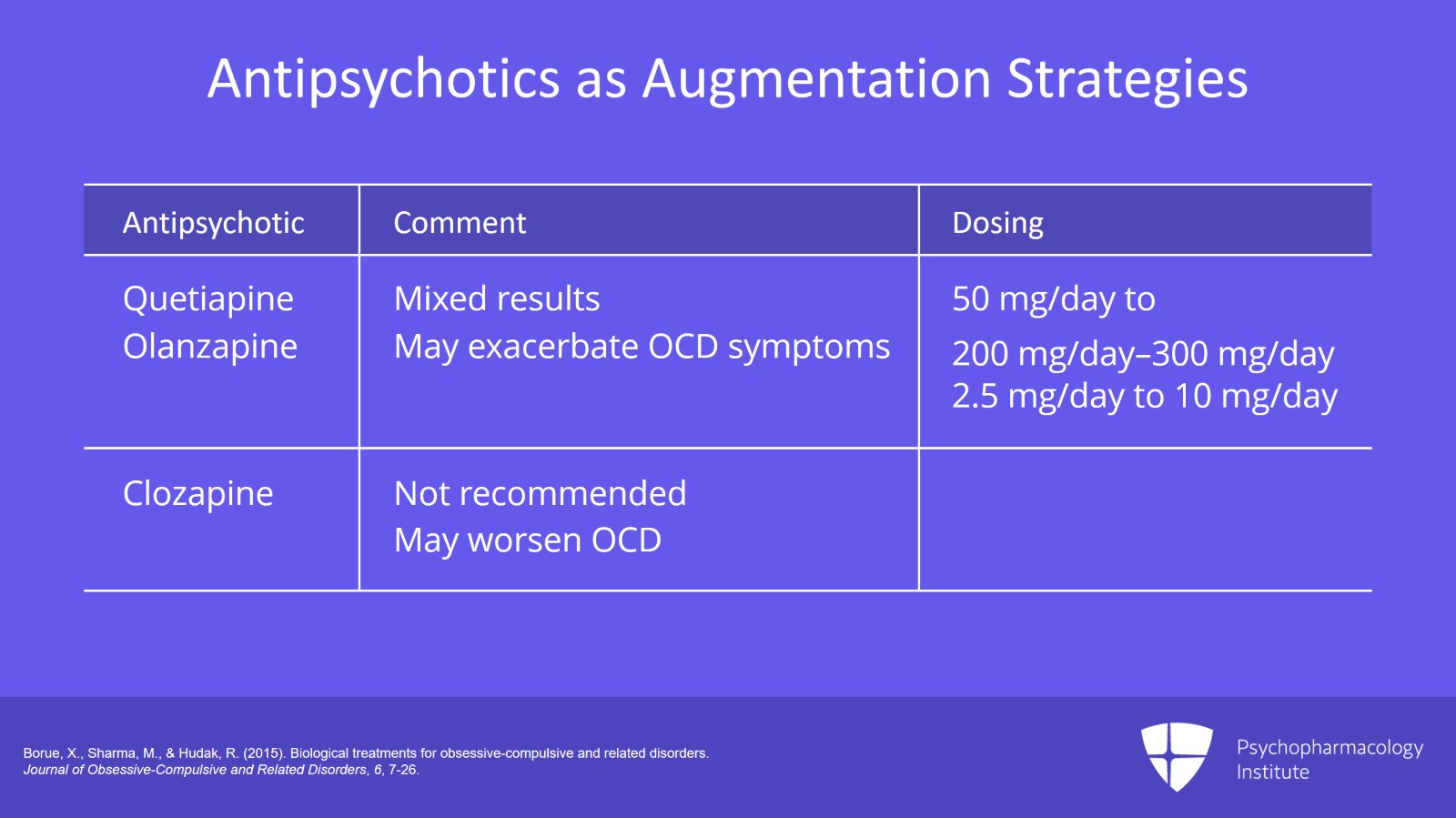
Now, there are two other antipsychotics that have some mixed data, quetiapine and olanzapine. Quetiapine has some mixed results in single-blind and double-blind studies. Some show it to be effective, others less so. Olanzapine has mixed results but it has two double-blind studies behind it, something that quetiapine doesn’t. Olanzapine may also specifically exacerbate OCD more so than other second-generation antipsychotics. Therefore, I consider as a third-line strategy for augmentation using a second-generation antipsychotics, quetiapine and olanzapine to be behind risperidone and aripiprazole.
Notice that there are very little data on other second-generation antipsychotics including clozapine. Therefore, I do not recommend that any other second-generation antipsychotics be used for augmentation. And in fact, clozapine may indeed exacerbate OCD and make OCD worse. And so that’s something that needs to be looked at. So for dosing of these medications, it’s much less than what’s used for schizophrenia or OCD. To give you some examples, typically I dose risperidone as OCD augmentation between 0.25 and 2 mg. Aripiprazole, between 2 and 10 mg. Quetiapine, between 50 and 200 to 300. And olanzapine, again somewhere between 2.5 to about 10 mg. So as augmentation, unlike the SSRIs where we’re using maximal dose, for the second-generation antipsychotics, we’re using much lower doses.
References:
- Borue, X., Sharma, M., & Hudak, R. (2015). Biological treatments for obsessive-compulsive and related disorders. Journal of Obsessive-Compulsive and Related Disorders, 6, 7-26.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 9
This is a slide from a study done by Foa, et al. and this was published in 2015. And it shows patients who are on stable high-dose SSRI treatment who are then given into two groups, one using ERP and the other using risperidone augmentation. And you can see that when it comes to which one is better, it’s clear who the winner here, no doubt about it, ERP augmentation does far better than risperidone augmentation does. So again, medications are not a magic solution in OCD. Appropriate ERP is the most powerful option we have to treat treatment-resistant OCD.
References:
- Foa, E. B., Simpson, H. B., Rosenfield, D., Liebowitz, M. R., Cahill, S. P., Huppert, J. D., … & Hahn, C. G. (2015). Six-month outcomes from a randomized trial augmenting serotonin reuptake inhibitors with exposure and ritual prevention or risperidone in adults with obsessive-compulsive disorder. The Journal of clinical psychiatry, 76(4), 440.
Slide 6 of 9
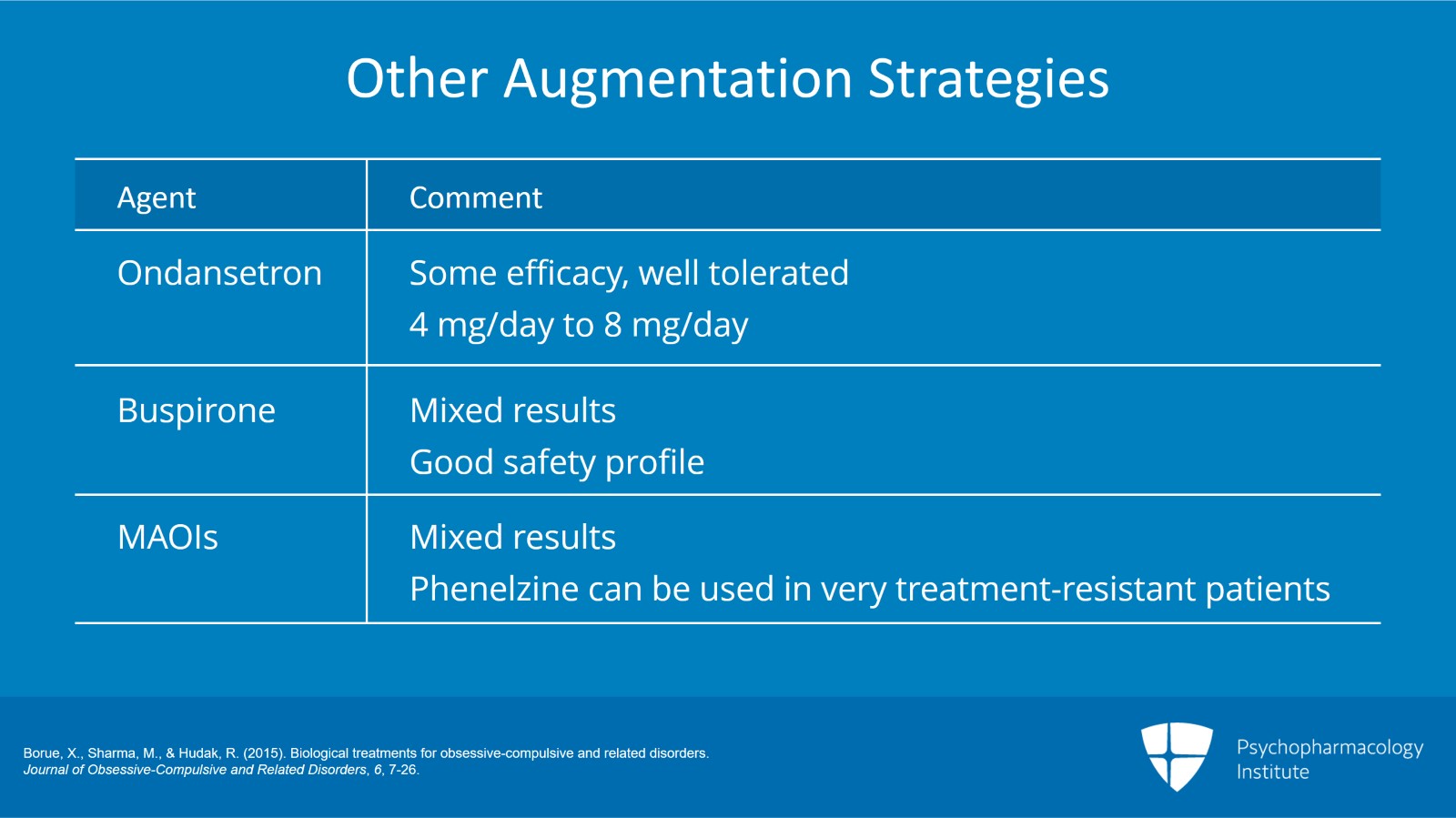
Ondansetron. It’s been studied in multiple trials, mostly small trials and it showed some efficacy in many of the trials. Because it’s well tolerated, consider this as an alternative trial medication. Usually dosed at typical doses of 4 to 8 mg daily. There are other medications that can be used as well.
Buspirone, the results on this are mixed but because of its extreme safety profile, it’s always worth the potential of an augmentation trial.
MAO inhibitors have shown some mixed results in OCD. There are some case reports some decades ago that said that it may be helpful in patients with symmetry obsessions. This is specifically phenelzine in that case, something that can be used in very treatment-resistant patients as a possibility.
References:
- Borue, X., Sharma, M., & Hudak, R. (2015). Biological treatments for obsessive-compulsive and related disorders. Journal of Obsessive-Compulsive and Related Disorders, 6, 7-26.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 9
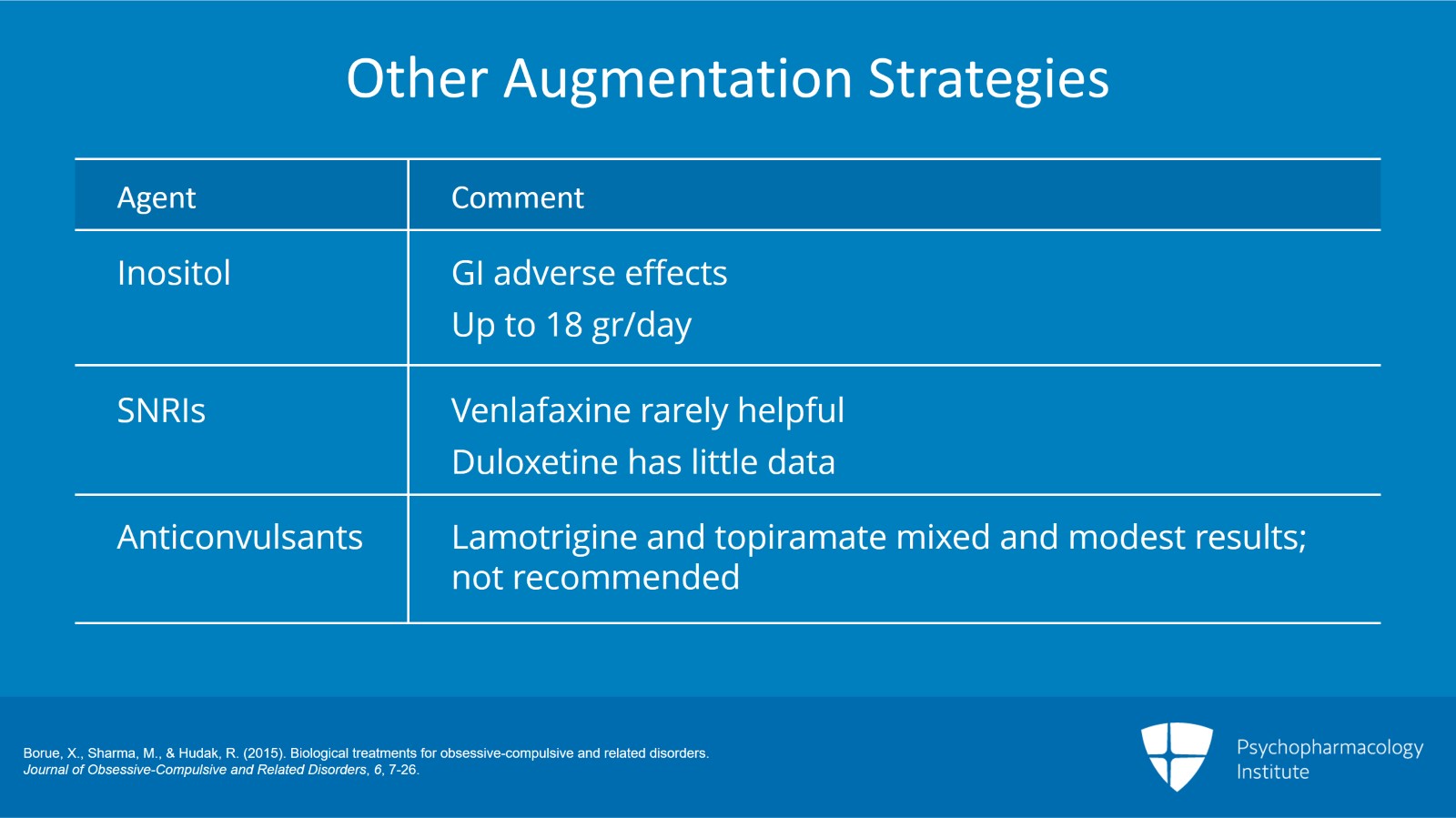
Inositol has been looked at in up to 18 grams a day. There has been one positive study shown as primary treatment. I will say that I have very rarely used inositol. Most patients cannot tolerate the GI side effects at the clinically effective doses.
There are some mixed data on SNRIs. Venlafaxine can be helpful maybe in some people but again very rare. There are really minimal data with duloxetine or other SNRIs and they’re again generally not recommended as an option.
Anticonvulsants, both lamotrigine and topiramate have been looked at. The results are mixed at best and very modest, generally not recommend for use in OCD.
References:
- Borue, X., Sharma, M., & Hudak, R. (2015). Biological treatments for obsessive-compulsive and related disorders. Journal of Obsessive-Compulsive and Related Disorders, 6, 7-26.
Slide 8 of 9
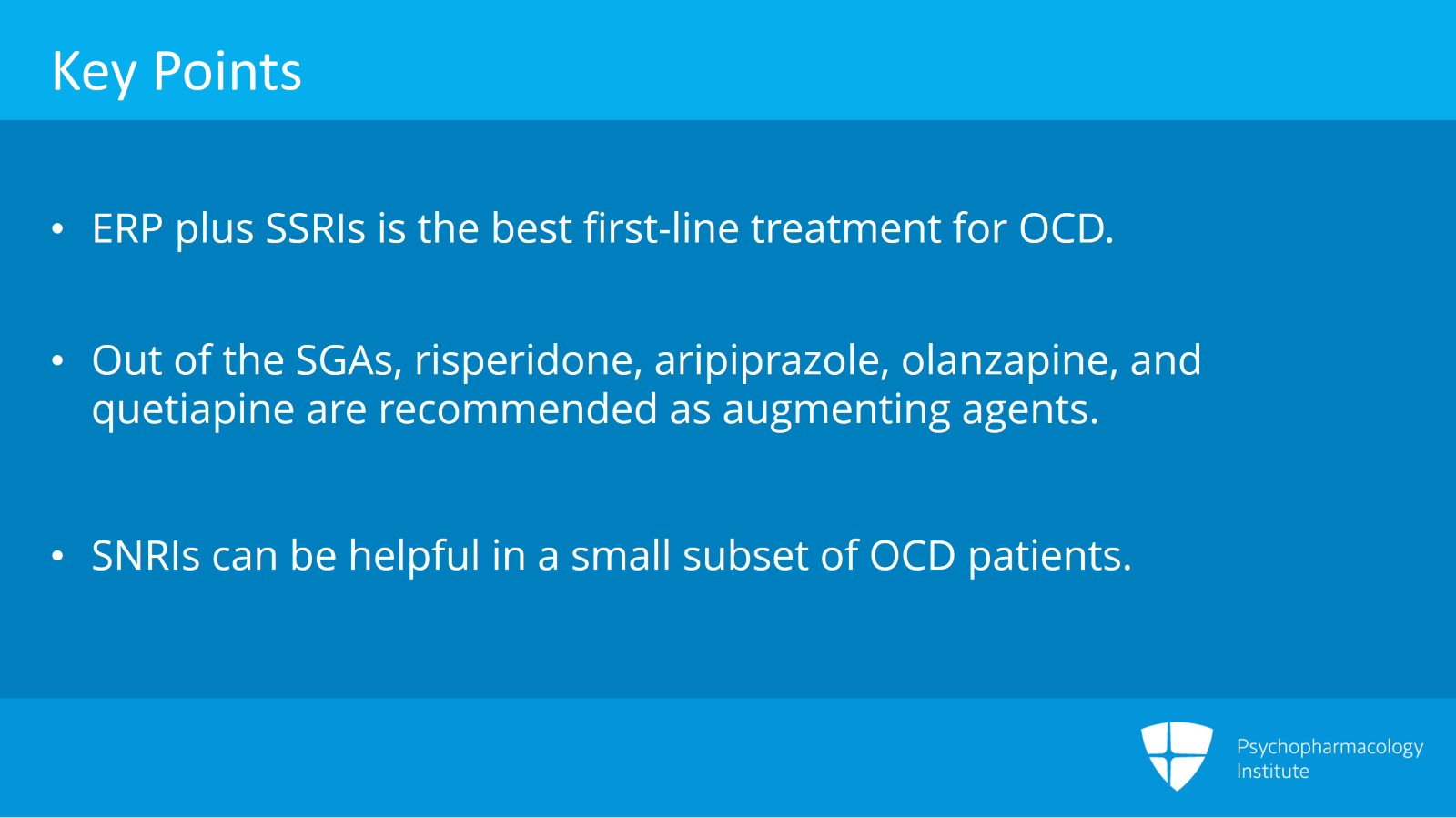
So the key points with this. Augmentation is important but studies indicate that ERP is better than the best medication augmentation. ERP plus SSRI is still the best first-line treatment for OCD.
Antipsychotics and especially the second-generation antipsychotics have shown to have positive clinical trials. However, they’re not a homogenous group of meds and it’s recommended that you augment with only four second-generation antipsychotics, risperidone, aripiprazole, and they have less data, olanzapine and quetiapine.
Data with other medication options are ongoing but much of that is still preliminary and I don’t recommend other medications for the most part as augmentation at this time. SNRIs can be helpful in a very small subset of OCD patients but really lack overall efficacy and in my mind make them what I call a last-line option.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.