Text version
Selecting Antipsychotics for First-Episode Psychosis
In this Quick Take, we’re examining an important question you may face when treating someone with first-episode psychosis or first-episode schizophrenia: Which antipsychotic should I start?
To address this question, I’ll discuss a 2024 prospective paper by Matej Markota and colleagues from the Mayo Clinic in Rochester, New York, published in the journal Schizophrenia. The authors correctly point out that the American Psychiatric Association’s schizophrenia guideline isn’t directive enough for many clinicians who need more concrete guidance. They note that existing guidelines differ in their conclusions and need an update.
The authors developed an algorithm focusing on medications with:
- Long-term efficacy data
- All-cause treatment discontinuation data
- Mortality data
Download PDF and other files
Violence Stratification Approach
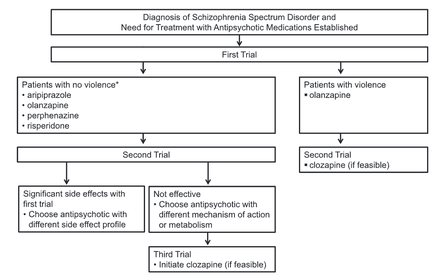
The algorithm begins after you’ve made a working diagnosis of a schizophrenia spectrum disorder. The first and most critical decision point is whether violence is present, which leads to two different pathways:
- Patients without violence (left pathway)
- Patients with concurrent violence (right pathway)
Violence can be subtle, like hostility, which is often measured in clinical schizophrenia trials with typical rating scales.
Non-Violent Patients: Four Equal Choices
For patients without violence, most guidelines prioritize antipsychotics with a low risk of side effects, particularly weight gain and metabolic syndrome. However, the authors disagree with this approach.
They list in alphabetical order four equally good choices for the first antipsychotic trial:
- Aripiprazole
- Olanzapine
- Perphenazine
- Risperidone
Download PDF and other files
Managing Side Effects and Non-Response
If side effects occur with the first selected antipsychotic, switch to one with different side effects. Most first-episode patients should respond well to first-line treatment.
If a patient doesn’t respond to the first choice:
- Switch to a second choice
- Then switch to clozapine
Violent Patients: Olanzapine First
For patients with comorbid violence in psychosis, the algorithm is simpler:
- Start with olanzapine
- If there is not a good response, switch to clozapine (if feasible)
Download PDF and other files
Key Aspects of the Algorithm
Two crucial elements of this algorithm are:
- Initial stratification based on violence presence/absence
- Inclusion of olanzapine as a good initial treatment despite metabolic risks
Olanzapine’s Inclusion as First-Line
I agree with including olanzapine as a first-line choice. Excluding a highly effective antipsychotic based solely on manageable side effects never made sense to me.
The authors reviewed a large body of recent literature indicating that long-term management with olanzapine does not lead to worse outcomes, including mortality when compared to risperidone or aripiprazole.
Possible explanations for olanzapine’s effectiveness:
- Good psychiatric efficacy allows better medical self-care
- Ataractic (calming) properties help with sleep
- Patient persistence with olanzapine due to perceived benefits
Download PDF and other files
Perphenazine’s Resurrection
The authors included perphenazine, an older first-generation antipsychotic, based on:
- Good mix of efficacy and tolerability
- Results from the CATIE trial
However, concerns about tardive dyskinesia temper my enthusiasm. The authors claim it has the lowest TD risk among first-generation antipsychotics, but I’m not certain this has been proven.
Amisulpride: A Potential Oversight
The authors acknowledge amisulpride could be an oversight in the algorithm. Although it’s not available in the US, where they practice, clinicians outside the US may want to include it.
Download PDF and other files
Olanzapine and Clozapine for Violent Patients
I appreciate the initial choice of olanzapine immediately followed by clozapine as a second step for patients who are hostile or violent. Several randomized trials show better efficacy for clozapine and olanzapine compared to haloperidol, especially in patients with conduct disorder or sociopathy in addition to their psychosis
It’s unfortunate that haloperidol is still widely used in forensic settings despite better alternatives.
Long-Acting Injectables Considerations
The authors briefly discussed LAIs, which I believe should be considered and discussed as a good first-line option. They have good evidence for reducing relapse and possibly mortality in first-episode patients.
- Aripiprazole and risperidone have the advantage that they can be easily switched to the long-acting injectable formulation once tolerability is established with the pill.
- Olanzapine is more problematic since many treatment systems in the United States aren’t set up for the monitoring requirements for long-acting injectable olanzapine.
- Perphenazine is also not available as a long-acting injectable in all countries including the United States.
Download PDF and other files
Clinical Bottom Line
For first-episode patients, the first decision about which antipsychotic to use needs to be made based on the presence or absence of violence:
- If violence is present:
- Try olanzapine first
- Then go immediately to clozapine
- If no violence, discuss these four choices with your patient:
- Olanzapine
- Risperidone
- Perphenazine
- Aripiprazole
These four have the best long-term efficacy and safety data, including mortality, according to the authors.
I usually limit my discussion to aripiprazole and olanzapine with first-episode patients when following this algorithm’s logic.
Download PDF and other files
Abstract
Updated rationale for the initial antipsychotic selection for patients with schizophrenia
Matej Markota, Robert J. Morgan III & Jonathan G. Leung
Introduction
Expert groups differ in their recommendations for early-stage schizophrenia treatment. Some expert groups, including American Psychiatric Association (APA), are non-directive and do not specify preferred agents for patients with first-episode psychosis1,2,3. This approach, while patient-centric, may challenge early practitioners and learners. Others offer algorithmic guidelines, but existing algorithms only partially agree on “first-line” treatments (see the section “Summary of first-line treatment options for patients without concurrent violence” for definition), reflecting the complexity of risk-benefit analysis4,5,6,7,8,9. In addition, updates to guidelines are essential to incorporate the latest research.
Based on up-to-date evidence (as of January 2024), we present a rationale for the selection of “first-line treatments” for patients with early-stage schizophrenia and challenges surrounding the selection of these agents. We present a general rationale, such that when idiographic factors of individuals dictate a different approach, the considerations discussed here should defer to individualized plans, and patients and practitioners should engage in shared decision-making at every step.
Reference
Markota, M. M.D., Morgan III, R. M.D. & Leung, J. M.D. (2024). Updated rationale for the initial antipsychotic selection for patients with schizophrenia. Schizophrenia, volume 10, Article number: 74.



