Slides and Transcript
Slide 2 of 10
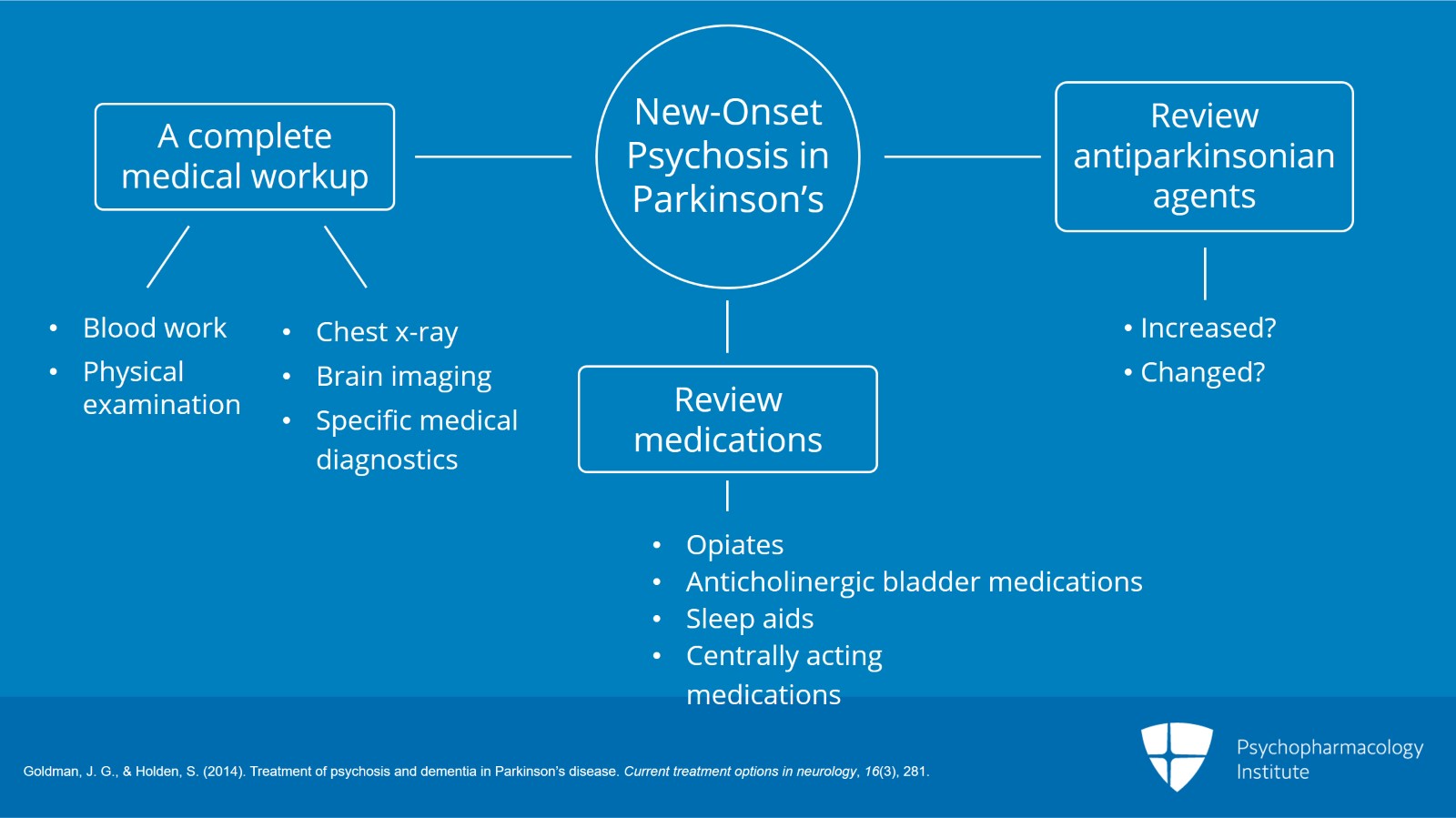
In the case of new onset psychosis in Parkinson’s, it’s very important to do a complete medical workup that includes blood work, physical examination and in some cases maybe even chest x-ray, head imaging or other specific types of medical diagnostics. You would want to review the medications to see if there’s anything that was either recently added or adjusted that could cause or contribute to the risk of psychosis in Parkinson’s. So common things are opiate pain medications, anticholinergic bladder medications or sleep aids. So diphenhydramine, for instance, is very commonly used as a sleep aid and can increase the risk of psychosis. And any centrally acting medication. If Parkinson’s medications had been recently increased or changed, that could be the cause of the new onset psychosis and you’d want to review that with the treating neurologist.
References:
- Goldman, J. G., & Holden, S. (2014). Treatment of psychosis and dementia in Parkinson’s disease. Current treatment options in neurology, 16(3), 281.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
And if you don’t find any medical cause to explain the onset of psychosis, you might assume then that it’s related to the overall disease process and the use of dopaminergic therapies and consider the use of antipsychotic. There is some evidence that treatment with cholinesterase inhibitors might be helpful but this is a lower level of evidence that primarily comes from secondary outcomes in cholinesterase trials for cognitive impairment. And then there are some non-pharmacologic techniques to address Parkinson’s disease psychosis. So for instance, there are things like looking away from the visual hallucination and then looking back, keeping rooms better lit, avoiding isolation and things like that.
References:
- Goldman, J. G., & Holden, S. (2014). Treatment of psychosis and dementia in Parkinson’s disease. Current treatment options in neurology, 16(3), 281.
Slide 4 of 10
When we talk about antipsychotic therapy in Parkinson’s, the main risk is that antipsychotics work by blocking postsynaptic dopamine receptors. And if you do this in Parkinson’s disease, you’ll worsen the motor function. So essentially, you’re working against the main treatment of Parkinson’s. And so you have to choose antipsychotics that avoid this postsynaptic D2, dopamine type 2, receptor blockade. And really, there are only three that do this in an acceptable way for Parkinson’s and that’s clozapine and quetiapine which are available on the market in most countries and then a new drug called pimavanserin.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
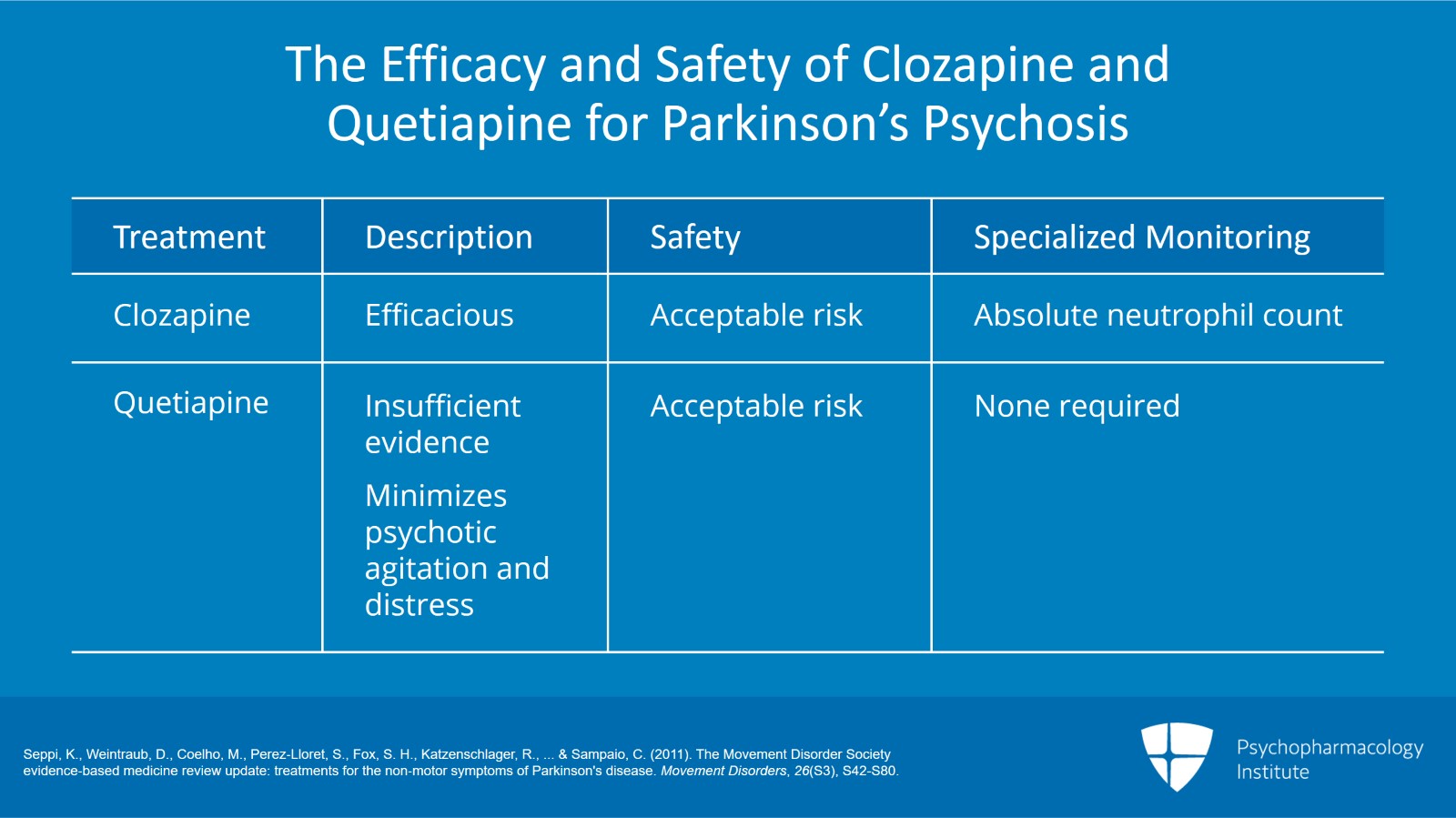
Now, all of these drugs have been shown to have efficacy to some extent in clinical trials. And what this table I’m presenting shows is sort of the summation of evidence. And basically, you can see that clozapine is clearly efficacious and has acceptable risk but requires specialized monitoring. And this monitoring is primarily for the absolute neutrophil count because there’s a risk of neutropenia and agranulocytosis which can be a life-threatening side effect. Quetiapine, when you look at all of the trials, it lacks evidence of clear efficacy but it doesn’t require specialized monitoring. And if nothing else, it seems to sort of minimize the agitation and distress caused by the psychosis if it doesn’t actually modify the actual psychosis. So it still is often used and practiced despite this lack of efficacy.
References:
- Seppi, K., Weintraub, D., Coelho, M., Perez‐Lloret, S., Fox, S. H., Katzenschlager, R., … & Sampaio, C. (2011). The Movement Disorder Society evidence‐based medicine review update: treatments for the non‐motor symptoms of Parkinson's disease. Movement Disorders, 26(S3), S42-S80.
Slide 6 of 10
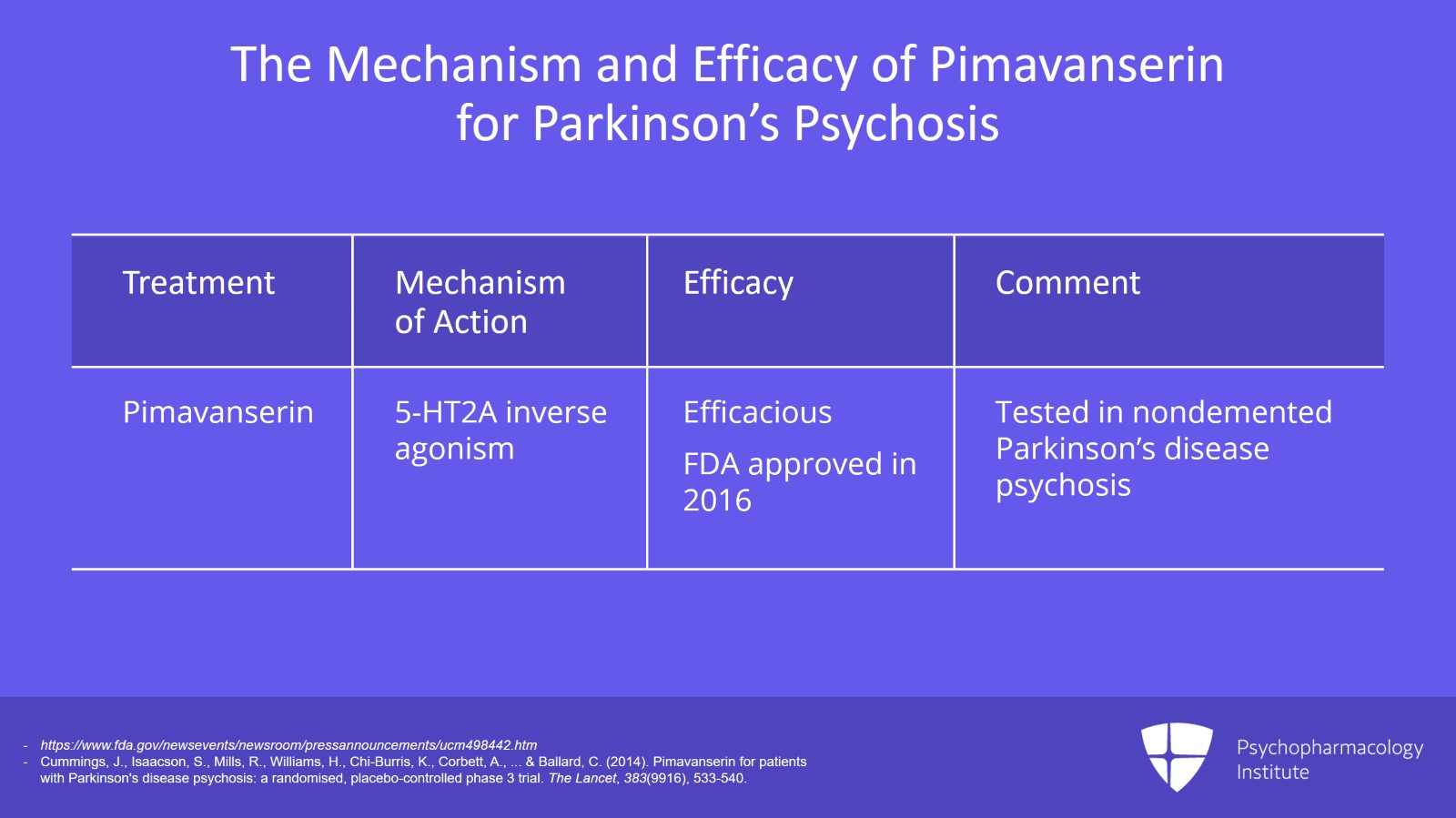
The newest drug is pimavanserin which works through 5-HT2A inverse agonism. So it’s a serotonergic mechanism. It’s proven to be efficacious in the treatment of Parkinson’s disease psychosis and doesn’t impair motor function and is generally well tolerated. There is one caveat. It’s mostly at this point been tested in non-demented Parkinson’s disease psychosis. And so if you’re using it in demented Parkinson’s, there may be additional considerations. So just keep that in mind.
References:
- https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm498442.htm
- Cummings, J., Isaacson, S., Mills, R., Williams, H., Chi-Burris, K., Corbett, A., … & Ballard, C. (2014). Pimavanserin for patients with Parkinson's disease psychosis: a randomised, placebo-controlled phase 3 trial. The Lancet, 383(9916), 533-540.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
But using any of the other antipsychotics, you risk worsening the Parkinson’s disease and use of almost any antipsychotic increases the risk of all-cause mortality in the elderly. And so you want to also know that you’re accepting that risk by the time you choose to use these medications for psychosis in Parkinson’s.
References:
- http://www.fda.gov/Drugs/DrugSafety/ucm124830.htm
Slide 8 of 10
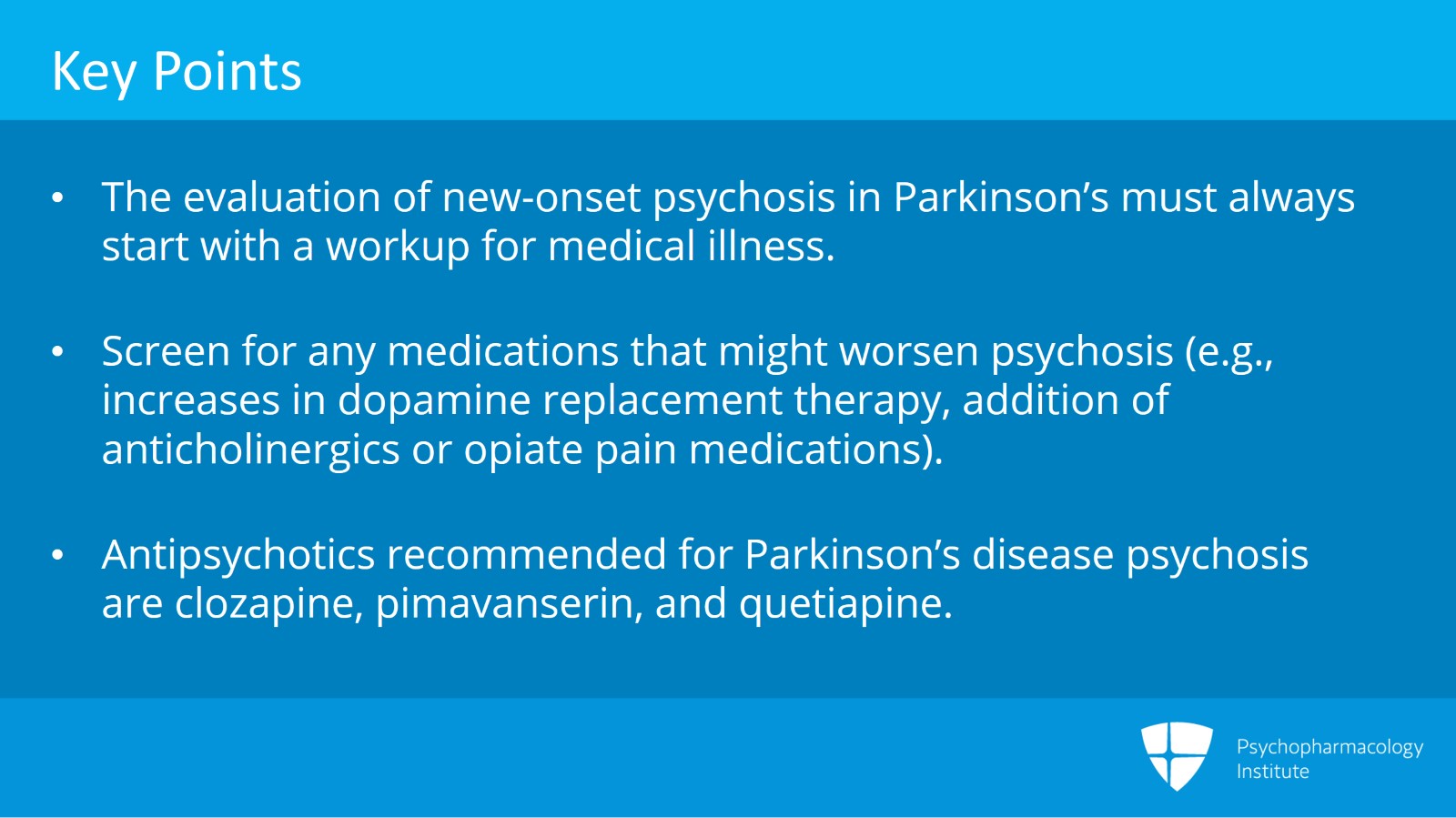
So the key points here are that the evaluation of new onset psychosis in Parkinson’s must always start with a workup for medical illness. These are things like urinary tract infection and pneumonia most commonly and screening for any medications that might worsen the psychosis. So recent increases in the dopamine replacement therapy, addition of anticholinergics or opiate pain medications are common ones there. To avoid worsening the motor symptoms of Parkinson’s, there are really only three antipsychotics that are recommended for Parkinson’s disease psychosis and those are clozapine, pimavanserin and quetiapine.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
If reduction of dopamine replacement therapy is necessary, meaning you’ve tried all these other things and it still is causing a problem, you want to remove the dopamine replacement medications with the least relative motor benefit. And so these are things like the amantadine, the monoamine oxidase inhibitors like rasagiline and selegiline, the COMT inhibitors and dopamine agonists. And then finally, the most potent motor medication, levodopa, should be left for last if possible because you’ll have the most movement loss by removing that.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.