Slides and Transcript
Slide 1 of 10
So we've talked a bit about nonpharmacological treatments for PMS and PMDD. What about psychopharmacology? Antidepressants are the first-line, gold standard treatment for PMS and PMDD.
Slide 2 of 10
And when symptoms are severe or not completely relieved by nonpharmacologic treatments, antidepressant treatment is indicated and essential. It can be combined with nonpharmacologic treatments or it can be used on its own.
References:
- Steiner, M., Pearlstein, T., Cohen, L. S., Endicott, J., Kornstein, S. G., Roberts, C., … & Yonkers, K. (2006). Expert guidelines for the treatment of severe PMS, PMDD, and comorbidities: the role of SSRIs. Journal of women's health, 15(1), 57-69.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
So what do we know about antidepressant treatment? SSRIs are the first-line treatment and there have been at least 40 placebo-controlled, randomized controlled trials of SSRIs for either PMS or PMDD. Of those women with PMS or PMDD, about 60% to 70% will respond to SSRIs versus about 30% responding to placebo. Effective dosages are lower in PMDD than for MDD and response is more rapid.
References:
- Steiner, M., Pearlstein, T., Cohen, L. S., Endicott, J., Kornstein, S. G., Roberts, C., … & Yonkers, K. (2006). Expert guidelines for the treatment of severe PMS, PMDD, and comorbidities: the role of SSRIs. Journal of women's health, 15(1), 57-69.
- Freeman, E. W., Rickels, K., Sondheimer, S. J., Polansky, M., & Xiao, S. (2004). Continuous or intermittent dosing with sertraline for patients with severe premenstrual syndrome or premenstrual dysphoric disorder. American Journal of Psychiatry, 161(2), 343-351.
Slide 4 of 10
So antidepressants that primarily affect other transmitters other than serotonin are not effective for PMS or PMDD. So, for example, you don't want to use desipramine which is a noradrenergic antidepressant, bupropion which has weak serotonin, it's mostly noradrenergic and dopaminergic, or maprotiline, for example, which is noradrenergic. The unique feature of SSRI response in PMDD is that it's rapid onset such that intermittent dosing and SSRI taken only in the luteal phase is effective. Many women find this very comforting. They don't like the idea of being on a drug all the time. And knowing that luteal phase dosing is possible makes psychopharmacologic treatment more palatable for some patients.
References:
- Steiner, M., Pearlstein, T., Cohen, L. S., Endicott, J., Kornstein, S. G., Roberts, C., … & Yonkers, K. (2006). Expert guidelines for the treatment of severe PMS, PMDD, and comorbidities: the role of SSRIs. Journal of women's health, 15(1), 57-69.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
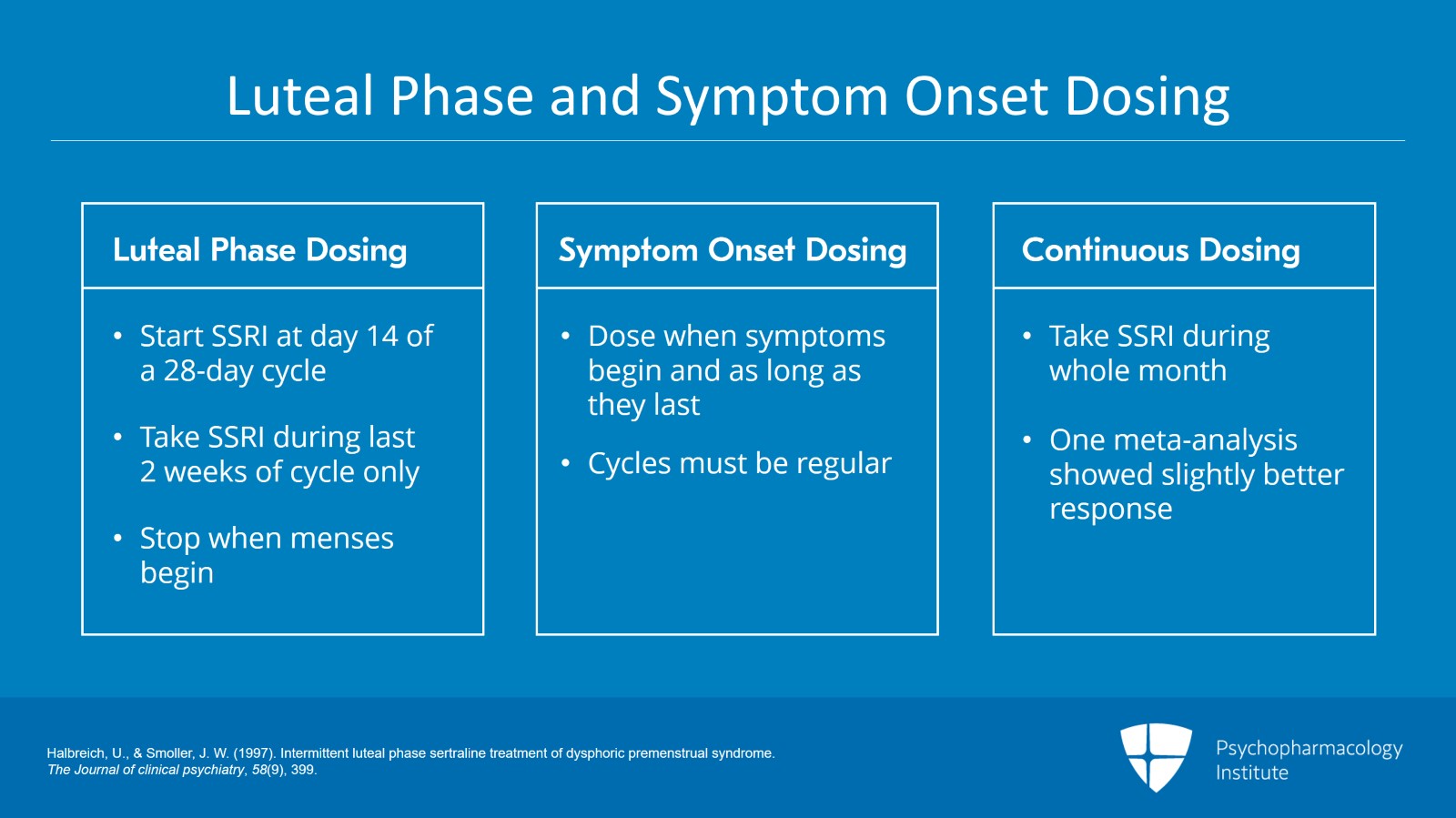
Let me just take a step back here and make sure that I've defined my terms. What do I mean by luteal phase dosing or symptom-onset dosing? Well, luteal phase dosing would mean starting the SSRI in the luteal phase, after the woman ovulates which is usually around day 14 of a 28-day cycle and taking the SSRI during the last two weeks of the cycle only and stopping it once menses begin. Symptom-onset dosing, on the other hand, would happen only at the moment when the symptoms begin. So the luteal phase is two weeks long. For some women, that means they have symptoms during those two weeks. For some women, the symptoms may be only seven or eight days or only three or four days. For those women, you could start the SSRI at the time that symptoms begin as long as they have regular cycles and can reasonably predict when they will get symptoms in every cycle. Continuous dosing means taking it just the way you do for major depressive disorder or taking it the whole month. Some women will actually prefer that because then they don't have to remember to start it up in the middle of the month. There's one meta-analysis that did show that response was slightly better when you took the SSRI as a continuous dose rather than luteal phase.
References:
- Halbreich, U., & Smoller, J. W. (1997). Intermittent luteal phase sertraline treatment of dysphoric premenstrual syndrome. The Journal of clinical psychiatry, 58(9), 399.
Slide 6 of 10
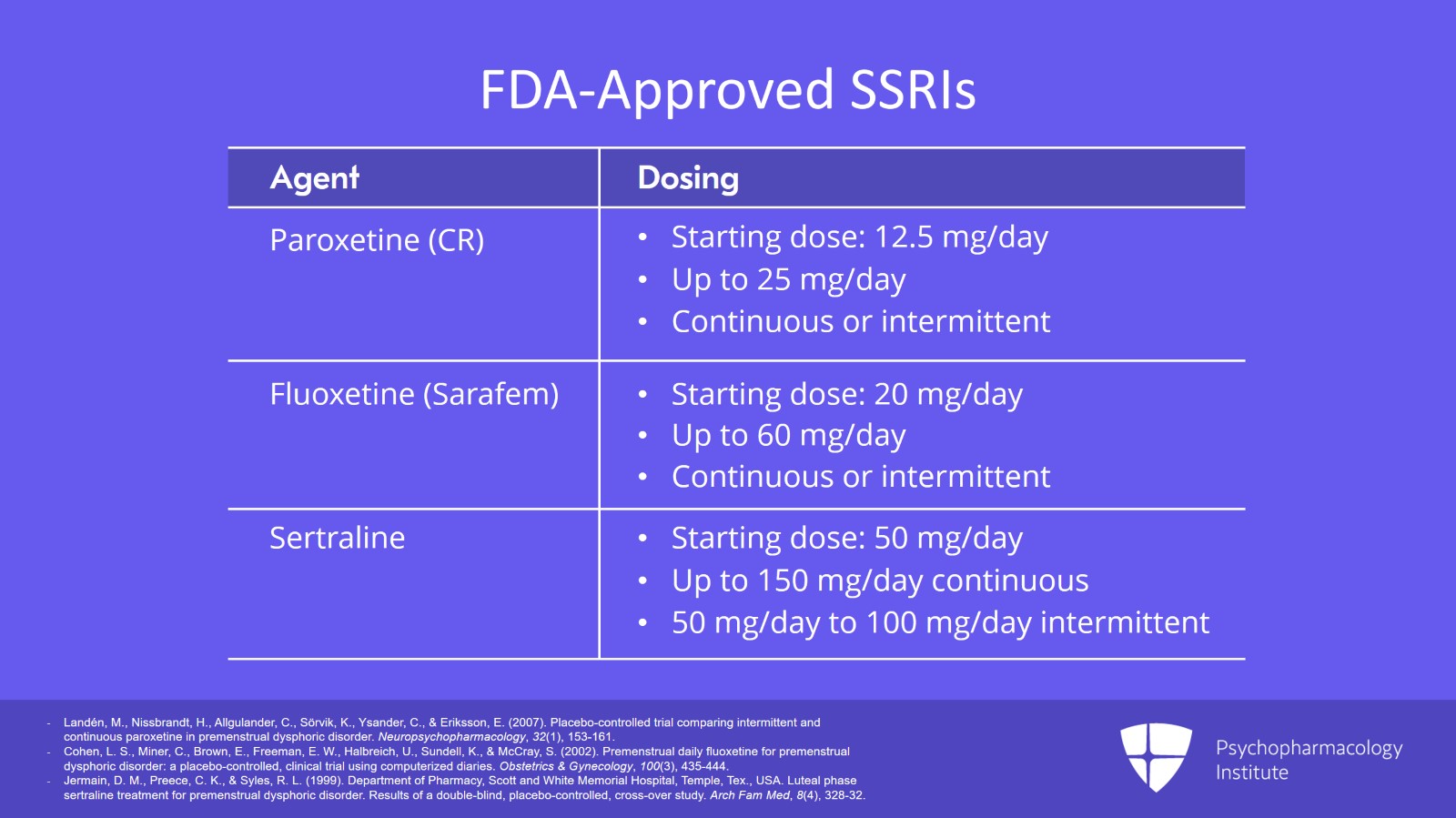
So we know that there are a number of SSRIs that are FDA approved for PMDD but other SSRIs are likely equally effective. They just haven't been studied enough to be FDA approved. Most of the studies show that there's actually no difference in efficacy by method of dosing whether you dose them luteal phase only, symptom onset only or continuous. The three SSRIs that have been FDA approved are controlled release paroxetine, fluoxetine, and sertraline. And what we also know about SSRIs in PMDD is that they can be used at much lower doses than we use them for major depressive disorder. So for the controlled release paroxetine, the usual starting dose for PMDD is 12.5 mg and using it at 12.5 to 25 mg a day either continuous or intermittent dosing. For fluoxetine, usual starting dose will be 20 mg and use again 20 to 60 mg for either continuous or intermittent dosing. And for sertraline, that usual starting dose would be 50 mg and using it 50 to 150 when there is continuous dosing and 50 to 100 for intermittent dosing.
References:
- Landén, M., Nissbrandt, H., Allgulander, C., Sörvik, K., Ysander, C., & Eriksson, E. (2007). Placebo-controlled trial comparing intermittent and continuous paroxetine in premenstrual dysphoric disorder. Neuropsychopharmacology, 32(1), 153-161.
- Cohen, L. S., Miner, C., Brown, E., Freeman, E. W., Halbreich, U., Sundell, K., & McCray, S. (2002). Premenstrual daily fluoxetine for premenstrual dysphoric disorder: a placebo-controlled, clinical trial using computerized diaries. Obstetrics & Gynecology, 100(3), 435-444.
- Jermain, D. M., Preece, C. K., & Syles, R. L. (1999). Department of Pharmacy, Scott and White Memorial Hospital, Temple, Tex., USA. Luteal phase sertraline treatment for premenstrual dysphoric disorder. Results of a double-blind, placebo-controlled, cross-over study. Arch Fam Med, 8(4), 328-32.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
The other SSRIs, citalopram, fluvoxamine and escitalopram, appear to be similarly effective. There was one small negative study with fluvoxamine but otherwise the evidence is good that they are similarly effective but they have not been FDA approved for this indication. We don't have any direct comparisons among the SSRIs to establish their relative effectiveness. So there isn't any one best SSRI to PMDD. It's likely that individual response and tolerability will vary from drug to drug and person to person and there's no way to predict this in advance. So the way I generally choose is based on the side effect profiles and other symptoms that we're trying to target, which drug makes the most sense for that person and also talking to them about whether other women in their family have had premenstrual symptoms and have had particularly good response to one drug or the other.
Slide 8 of 10
So key points of this section are that SSRIs are first-line treatment for PMDD but only serotonergic antidepressants will work for this. So you don't want to choose an antidepressant that does not have action on serotonin. You can use lower doses than you do for major depressive disorder and the response will be almost immediate.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
While there are only three medications that are FDA approved for PMDD, there's likely equal efficacy for the other SSRIs so no real reason to choose one of the FDA approved ones over the ones that are equally efficacious unless you have a reason to need something that's been FDA approved for this indication.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.