Slides and Transcript
Slide 1 of 10
In the sixth section of these talks on the assessment and management of first episodes of psychosis, I'm going to talk about treatment resistance which can occur within the first episode.
Slide 2 of 10
This is from a study which is done here at my home, UCLA, where we looked at remission in patients receiving a long-acting antipsychotic and those on oral medications. And what you see is that remission rates were much higher on long-acting antipsychotic.
References:
- Subotnik, K. L., Casaus, L. R., Ventura, J., Luo, J. S., Hellemann, G. S., Gretchen-Doorly, D., Marder, S., & Nuechterlein, K. H. (2015). Long-acting injectable Risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. JAMA Psychiatry, 72(8), 822.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
And what this suggests is that one of the important predictors of poor outcome in these first episodes is probably going to be nonadherence to oral medications. And when patients do poorly during a first episode, I think this needs to be one of the first considerations.
References:
- Subotnik, K. L., Casaus, L. R., Ventura, J., Luo, J. S., Hellemann, G. S., Gretchen-Doorly, D., Marder, S., & Nuechterlein, K. H. (2015). Long-acting injectable Risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. JAMA Psychiatry, 72(8), 822.
Slide 4 of 10
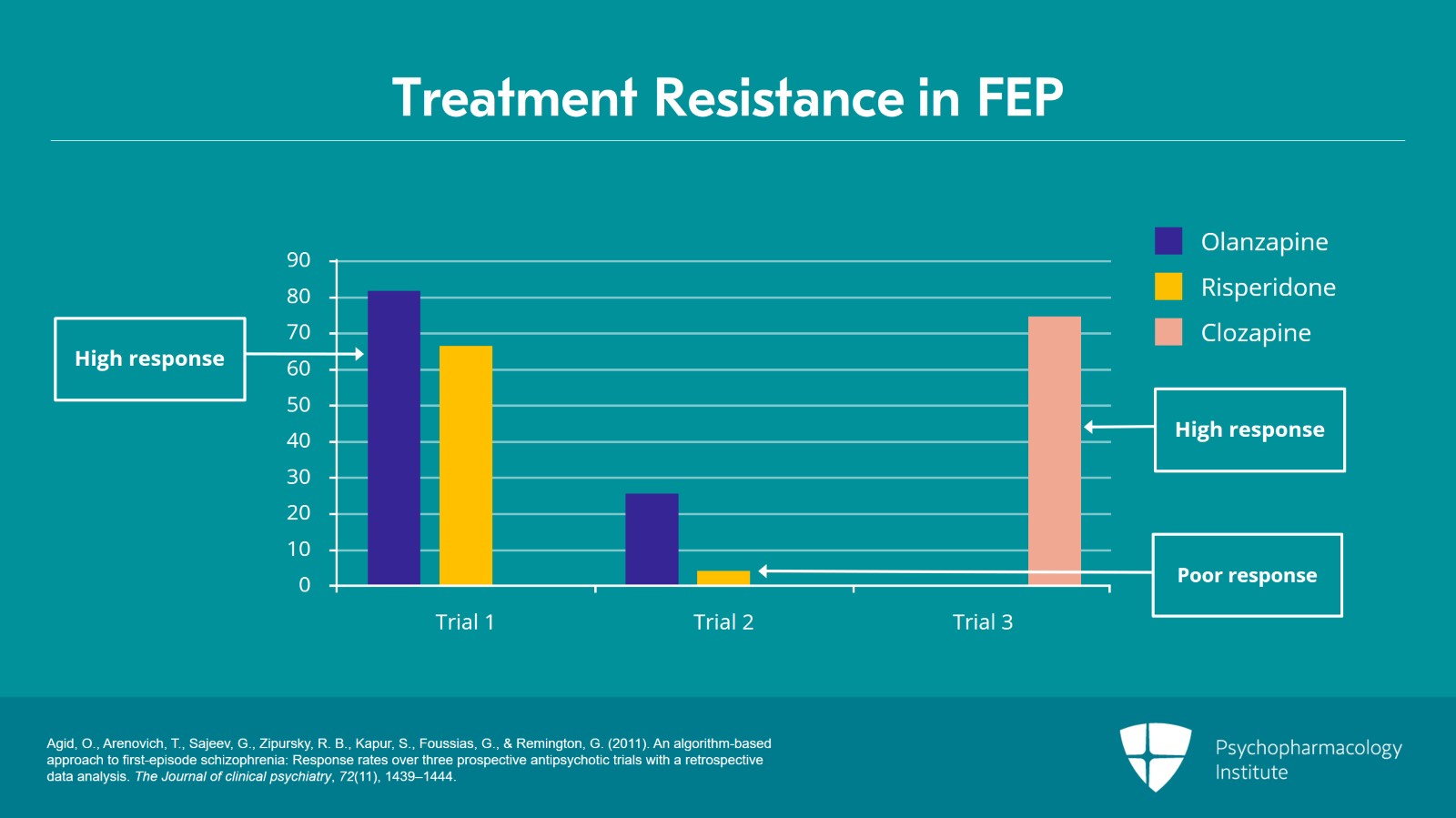
But let me talk about what we've learned about what to do if somebody is treatment resistant after a first episode. This slide is a study by Ofer Agid in Canada in which patients were treated with either olanzapine or risperidone.
References:
- Agid, O., Arenovich, T., Sajeev, G., Zipursky, R. B., Kapur, S., Foussias, G., & Remington, G. (2011). An algorithm-based approach to first-episode schizophrenia: Response rates over three prospective antipsychotic trials with a retrospective data analysis. The Journal of clinical psychiatry, 72(11), 1439–1444.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
If they didn't respond, they were switched to the other medication, risperidone to olanzapine or olanzapine to risperidone. And then they would measure response rate. And if they were still nonresponsive, they were changed to clozapine.
References:
- Agid, O., Arenovich, T., Sajeev, G., Zipursky, R. B., Kapur, S., Foussias, G., & Remington, G. (2011). An algorithm-based approach to first-episode schizophrenia: Response rates over three prospective antipsychotic trials with a retrospective data analysis. The Journal of clinical psychiatry, 72(11), 1439–1444.
Slide 6 of 10
In trial 1, there were high response rates on both, as I said in my past talk that you could expect something around 80% remission rate. But look what happens next time. The people who didn't respond to olanzapine when they were put on risperidone, their response rate was 4% which is pretty poor. For people who were on risperidone then changed to olanzapine, it was only 26% which suggests that switching to another second-generation antipsychotic is not very likely to work. But if you look at the next, trial 3, you'll see that things changed dramatically and that when these people were changed to clozapine there was a 75% response rate.
References:
- Agid, O., Arenovich, T., Sajeev, G., Zipursky, R. B., Kapur, S., Foussias, G., & Remington, G. (2011). An algorithm-based approach to first-episode schizophrenia: Response rates over three prospective antipsychotic trials with a retrospective data analysis. The Journal of clinical psychiatry, 72(11), 1439–1444.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
What I'm trying to emphasize is that there is a high likelihood that patients if they don't respond to one or even two antipsychotics, putting them on another one is not very likely to be helpful. Clozapine is likely to make a difference.
References:
- Agid, O., Arenovich, T., Sajeev, G., Zipursky, R. B., Kapur, S., Foussias, G., & Remington, G. (2011). An algorithm-based approach to first-episode schizophrenia: Response rates over three prospective antipsychotic trials with a retrospective data analysis. The Journal of clinical psychiatry, 72(11), 1439–1444.
Slide 8 of 10
This is why the guidelines from the UK, the National Institute on Clinical Excellence, suggest that even in children and young people who haven't responded despite receiving two antipsychotics that they should have a clozapine trial. Clozapine is too often reserved for patients who are severely ill and in the late stages of illness. I think it's probably more reasonable, to get people on clozapine treatment at the relatively early stages of illness.
References:
- National Institute for Health and Care Excellence (Great Britain). (2013). Psychosis and schizophrenia in children and young people: Recognition and management. https://www.nice.org.uk/guidance/cg155/update/cg155/documents/new-nice-guidance-on-psychosis-and-schizophrenia-in-children-and-young-people
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
So in this talk on treatment resistance in first episodes, I've tried to make two points. First, when a first episode patient fails to respond to an antipsychotic trial particularly when they're on oral medications, one should consider nonadherence as a cause and one can either intervene by better education or putting them on a long-acting antipsychotic. Other intervention which seems to have a high likelihood of being effective is the use of clozapine and that has a very important role even at the early stages of the illness. Thank you.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.