Slides and Transcript
Slide 2 of 15
Now, in regard to our own experience at the Minnesota Regional Sleep Disorder Center, our timeline involved the formal identification and naming of RBD in 1986 and 1987. In 1992, we identified the strong association of RBD with narcolepsy and cataplexy. Also in 1992, we identified medication-induced RBD with fluoxetine, an SSRI. 1997, we identified the parasomnia overlap disorder which is the combination of RBD and a disorder of arousal from non-REM sleep such as sleepwalking and sleep terrors.
References:
- Schenck, C. H., Bundlie, S. R., Ettinger, M. G., & Mahowald, M. W. (1986). Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep, 9(2), 293-308.
- Schenck, C. H., Mahowald, M. W., Kim, S. W., O'Connor, K. A., & Hurwitz, T. D. (1992). Prominent eye movements during NREM sleep and REM sleep behavior disorder associated with fluoxetine treatment of depression and obsessive-compulsive disorder. Sleep, 15(3), 226-235.
- Schenck, C. H., Boyd, J. L., & Mahowald, M. W. (1997). A parasomnia overlap disorder involving sleepwalking, sleep terrors, and REM sleep behavior disorder in 33 polysomnographically confirmed cases. Sleep, 20(11), 972-981.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
And then the very important topic in Neuroscience took place in 1996 when we identified a conversion rate from idiopathic RBD to parkinsonism, mainly, Parkinson's disease and dementia of Lewy bodies. And then in 2013, we followed up our original series and we were astounded to find an 81% conversion rate from idiopathic RBD to Parkinson's disease or dementia of Lewy bodies. Our colleagues in Barcelona, Spain, found an 82% conversion rate in their series from idiopathic RBD to parkinsonism, virtually the same data.
References:
- Schenck, C. H., Boeve, B. F., & Mahowald, M. W. (2013). Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: A 16-year update on a previously reported series. Sleep Medicine, 14(8), 744-748.
- Iranzo, A., Tolosa, E., Gelpi, E., Molinuevo, J. L., Valldeoriola, F., Serradell, M., … & Santamaria, J. (2013). Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep behaviour disorder: An observational cohort study. The Lancet Neurology, 12(5), 443-453.
Slide 4 of 15
The prevalence of RBD is now known from two community-based epidemiologic studies to be 1%. The first study was in Switzerland that not only found a 1% prevalence rate in middle aged and older adults but they found an equal male to female ratio. Now, we know that women with more mild RBD still have the same prevalence rate as men. The second study was from Japan, again a community-based study that found a slightly more than 1% prevalence rate in older adult Japanese people. So really, the 1% prevalence rate for RBD is equivalent to the 1% prevalence of schizophrenia worldwide.
References:
- Haba-Rubio, J., Frauscher, B., Marques-Vidal, P., Toriel, J., Tobback, N., Andries, D., Preisig, M., Vollenweider, P., Postuma, R., & Heinzer, R. (2017). Prevalence and determinants of rapid eye movement sleep behavior disorder in the general population. Sleep, 41(2).
- Sasai-Sakuma, T., Takeuchi, N., Asai, Y., Inoue, Y., & Inoue, Y. (2020). Prevalence and clinical characteristics of REM sleep behavior disorder in Japanese elderly people. Sleep, 43(8).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
Now, we do have a validated single-question screen for RBD from a multicenter validation study and this can be used in a variety of clinical settings. The question is this: Have you ever been told or suspected yourself that you seem to act out your dreams while asleep, for example, punching, flailing your arms in the air, making running movements, etc.?
References:
- Postuma, R. B., Arnulf, I., Hogl, B., Iranzo, A., Miyamoto, T., Dauvilliers, Y., Oertel, W., Ju, Y., Puligheddu, M., Jennum, P., Pelletier, A., Wolfson, C., Leu-Semenescu, S., Frauscher, B., Miyamoto, M., Cochen De Cock, V., Unger, M. M., Stiasny-Kolster, K., Livia Fantini, M., … Montplaisir, J. Y. (2012). A single-question screen for rapid eye movement sleep behavior disorder: A multicenter validation study. Movement Disorders, 27(7), 913-916.
Slide 6 of 15
If there's a positive response to the screen, then that warrants a much more systematic sleep medicine evaluation with the clinical history and then the gold standard would be polysomnography to document the loss of REM atonia in the sleep lab.
References:
- Postuma, R. B., Arnulf, I., Hogl, B., Iranzo, A., Miyamoto, T., Dauvilliers, Y., Oertel, W., Ju, Y., Puligheddu, M., Jennum, P., Pelletier, A., Wolfson, C., Leu-Semenescu, S., Frauscher, B., Miyamoto, M., Cochen De Cock, V., Unger, M. M., Stiasny-Kolster, K., Livia Fantini, M., … Montplaisir, J. Y. (2012). A single-question screen for rapid eye movement sleep behavior disorder: A multicenter validation study. Movement Disorders, 27(7), 913-916.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
In terms of the treatment of RBD, the American Academy of Sleep Medicine published in 2010 in the Journal of Clinical Sleep Medicine, the "best practice guide for the treatment of REM sleep behavior disorder." First of all, you must protect the bedside environment. You want to remove any bedside table or any other type of objects that could cause injury. If you fling out your arm, you don't want to hit the corner of a table that could cause a serious injury. You don't want to sleep near the window which could be really devastating. I already mentioned that study showing defenestration or near defenestration from people sleeping near a bedroom window.
References:
- Aurora, R. N., Zak, R. S., Maganti, R. K., Auerbach, S. H., Casey, K. R., Chowdhuri, S., Karippot, A., Ramar, K., Kristo, D. A., & Morgenthaler, T. I. (2010). Best practice guide for the treatment of REM sleep behavior disorder (RBD). Journal of Clinical Sleep Medicine, 06(01), 85-95.
Slide 8 of 15
Now, there are some tips for patients who live in long-term care facilities or nursing homes who may have RBD. Obviously, protect the bedside environment but also use bed rails. You have to use common sense and look at the bed as a potential lethal situation for the sleeping patient with RBD and protect the bedside environment. Some patients even put pillows on the floor by their bedside as well.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
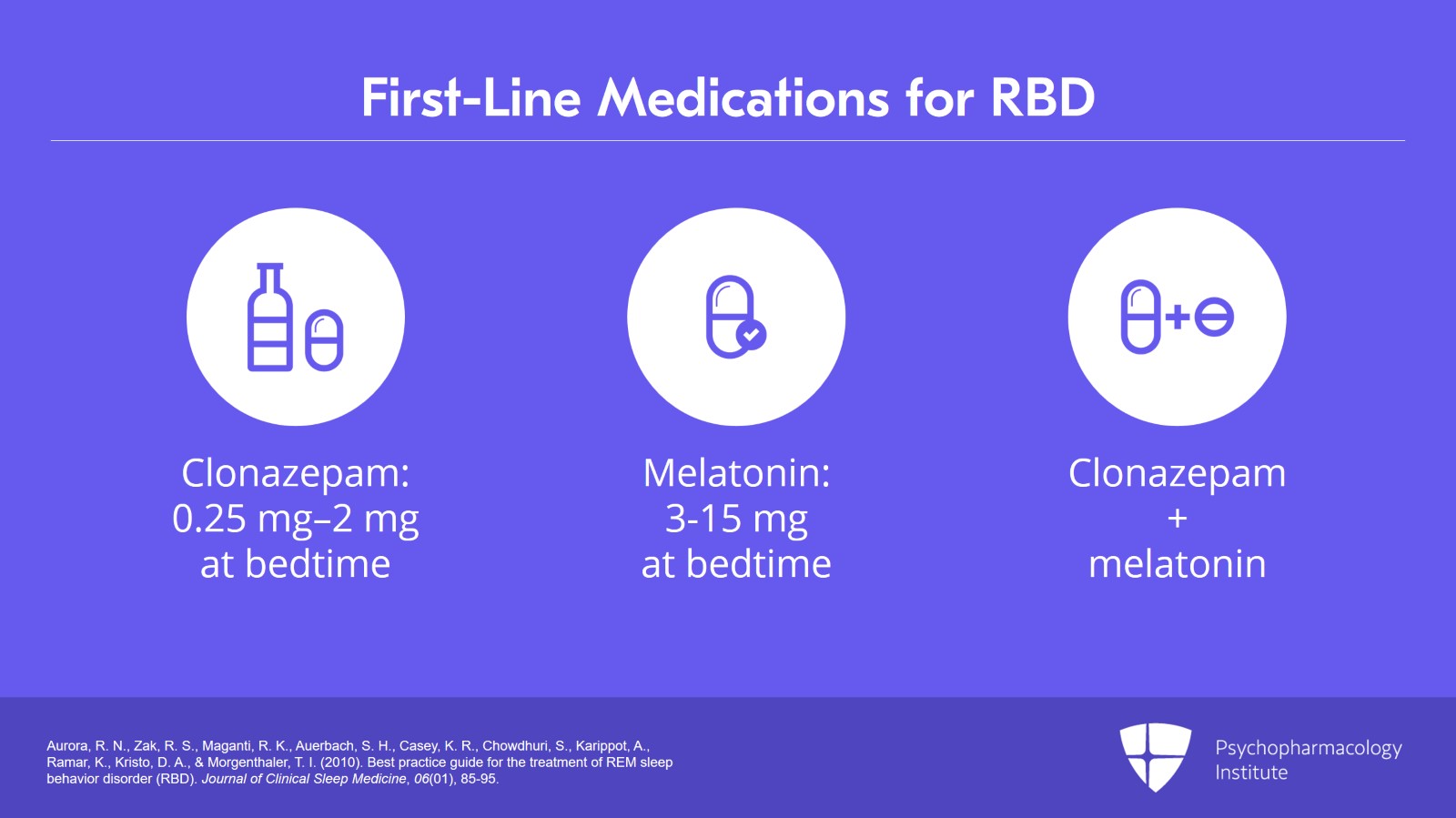
Now, there are two first-line medication treatments with between 80% and 90% published efficacy. First of all, clonazepam which was the medication we identified in our initial series, anywhere from 0.25 mg to 2 mg at bedtime but also melatonin can be very effective and usually in higher doses, up to 15 mg at bedtime or the combination of clonazepam and melatonin.
References:
- Aurora, R. N., Zak, R. S., Maganti, R. K., Auerbach, S. H., Casey, K. R., Chowdhuri, S., Karippot, A., Ramar, K., Kristo, D. A., & Morgenthaler, T. I. (2010). Best practice guide for the treatment of REM sleep behavior disorder (RBD). Journal of Clinical Sleep Medicine, 06(01), 85-95.
Slide 10 of 15
For RBD patients with Parkinson's disease, in 2016 a Japanese study identified ramelteon as being actually quite effective. Ramelteon is a selective melatonin 1 and melatonin 2 receptor agonist. So I think we should consider ramelteon in older patients with RBD alone or in combination with Parkinson's disease if clonazepam and/or melatonin are not effective or are not tolerated.
References:
- Kashihara, K., Nomura, T., Maeda, T., Tsuboi, Y., Mishima, T., Takigawa, H., & Nakashima, K. (2016). Beneficial effects of Ramelteon on rapid eye movement sleep behavior disorder associated with Parkinson's disease – Results of a multicenter open trial. Internal Medicine, 55(3), 231-236.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
Now, a question that's frequently brought up that I think is a very important question is – for patients with treatment-resistant depression who finally found an antidepressant that worked, that may have stopped suicidal ideation or major life dysfunction related to major depression, that patient and the treating psychiatrist, they don't want to give up on that medicine because of RBD being induced. I would agree that you need to keep the patient on the life-preserving, life-enhancing antidepressant medication and then you treat the RBD even though the offending agent is still being taken and that offending agent for RBD is critical for quality of life and saving a life in a severely depressed patient.
References:
- Standards of Practice Committee, Aurora, R. N., Zak, R. S., Maganti, R. K., Auerbach, S. H., Casey, K. R., … & Morgenthaler, T. I. (2010). Best practice guide for the treatment of REM sleep behavior disorder (RBD). Journal of Clinical Sleep Medicine, 6(1), 85-95
Slide 12 of 15
Key points. First, the prevalence of community-based polysomnography confirmed RBD in middle aged and older adults is 1%, comparable to the prevalence of schizophrenia. Second, a validated single-question screen for RBD has been published which can be utilized in a broad range of clinical settings.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
Effective pharmacotherapies of RBD exist although protecting the bedside environment remains of paramount importance.
Slide 14 of 15
And in particular rare cases where you cannot really think about switching to another antidepressant, then you treat the RBD while the offending medication continues to be taken. That will result in a positive outcome across the board.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.