Slides and Transcript
Slide 1 of 10
Here I’m going to talk about prescribing and monitoring lithium during pregnancy.
So you’ve decided that the risk of a mood episode versus medication exposure is such that it’s worth continuing medication treatment of lithium. Our prescribing and monitoring examples here are going to be for lithium but the concepts can be applied to prescribing other medications for mood in pregnancy as well.
Slide 2 of 10
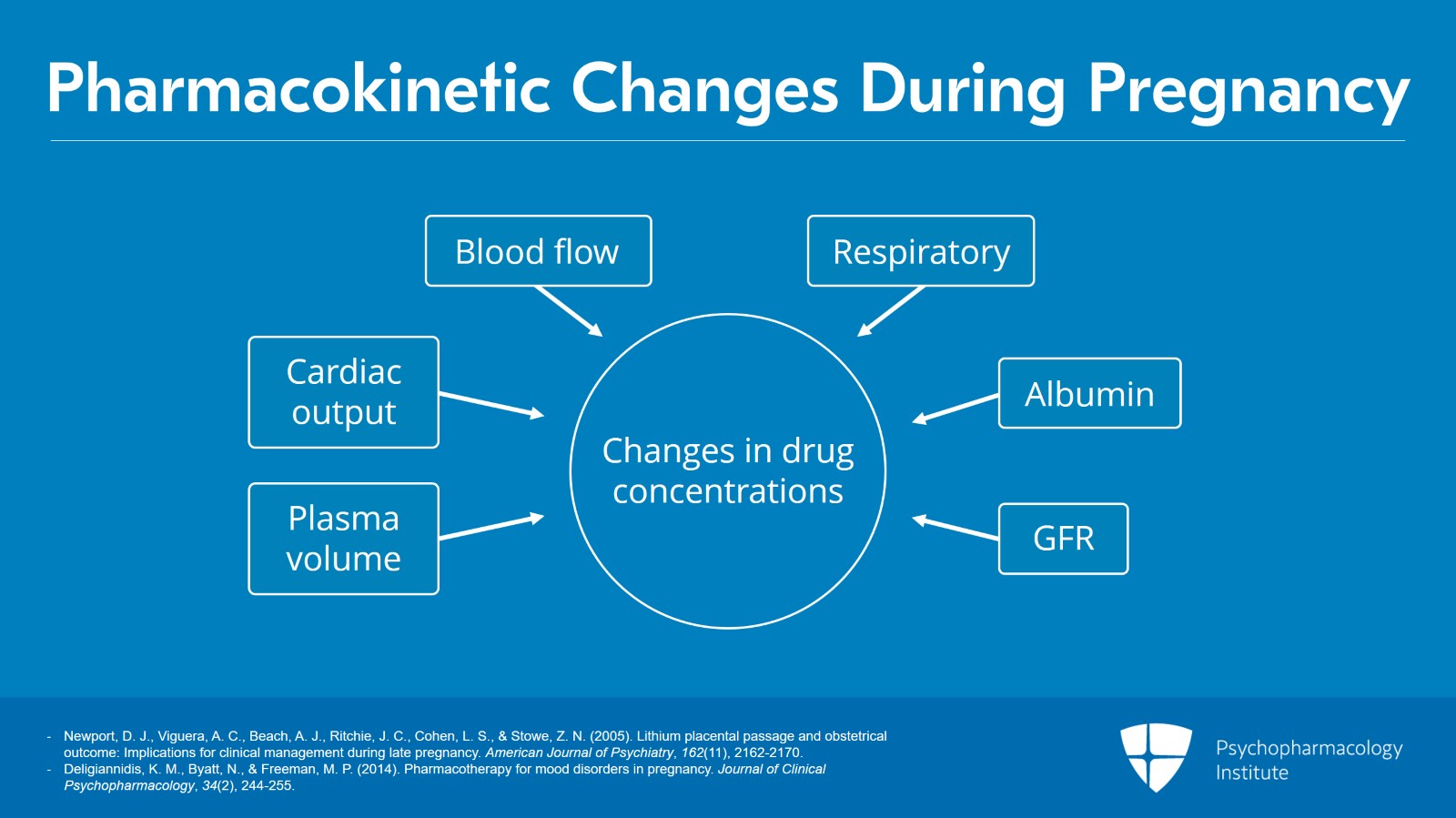
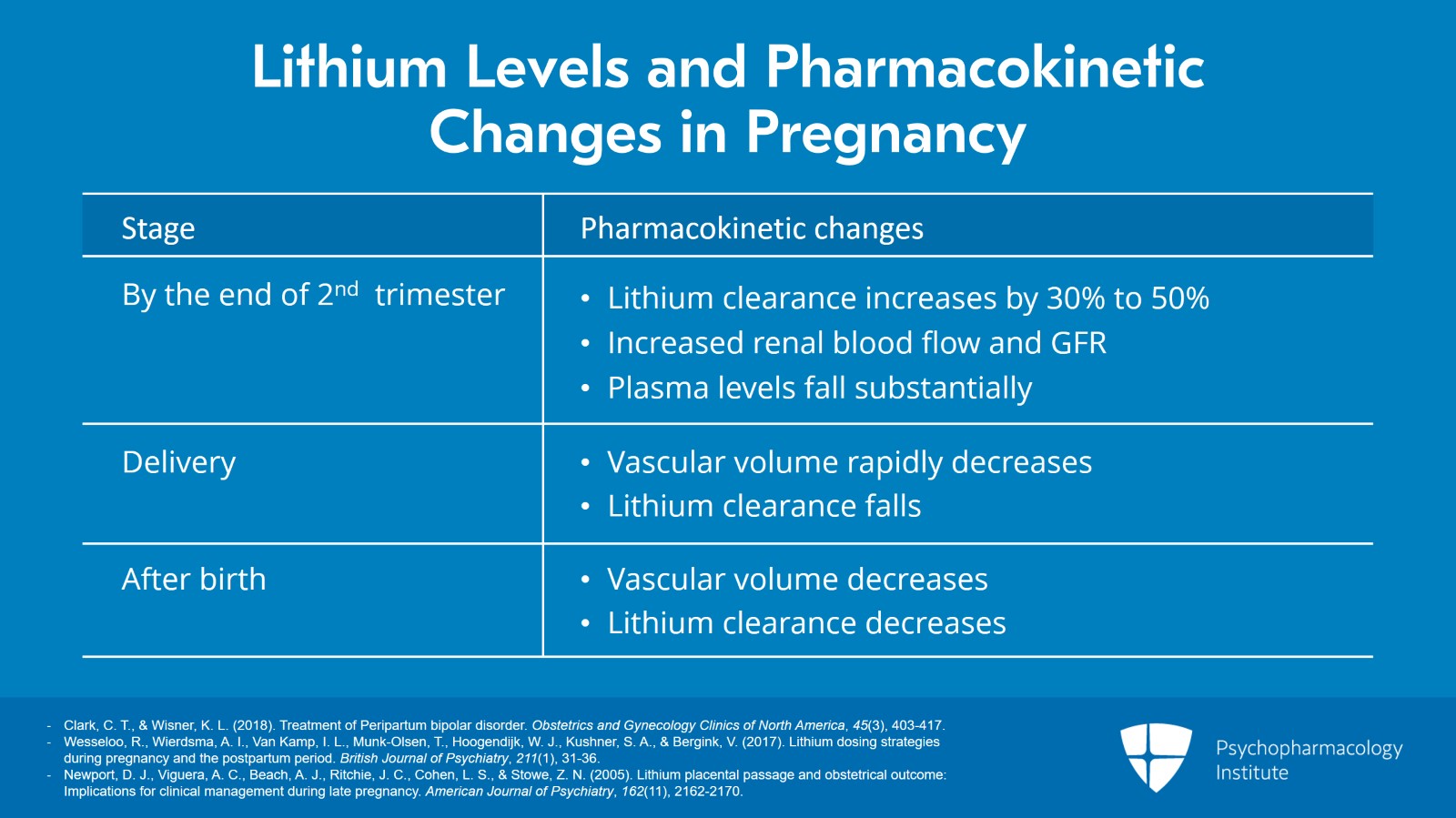
So the pharmacokinetics of lithium and most other meds change throughout pregnancy.
This image here is of the pharmacokinetic changes occurring during pregnancy. It’s an example of the complex biological changes that can influence psychotropic medications and their effects. For example, small to moderate sex differences which exist in drug absorption, distribution, metabolism and elimination may be amplified during pregnancy.
And using lithium in this example, there’s increased renal blood flow and associated increasing glomerular filtration rate that may increase the medication’s elimination during pregnancy.
Or increase hepatic blood flow may account for increased clearance and decreased concentrations of hepatically metabolized medication during pregnancy.
References:
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
- Deligiannidis, K. M., Byatt, N., & Freeman, M. P. (2014). Pharmacotherapy for mood disorders in pregnancy. Journal of Clinical Psychopharmacology, 34(2), 244-255.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
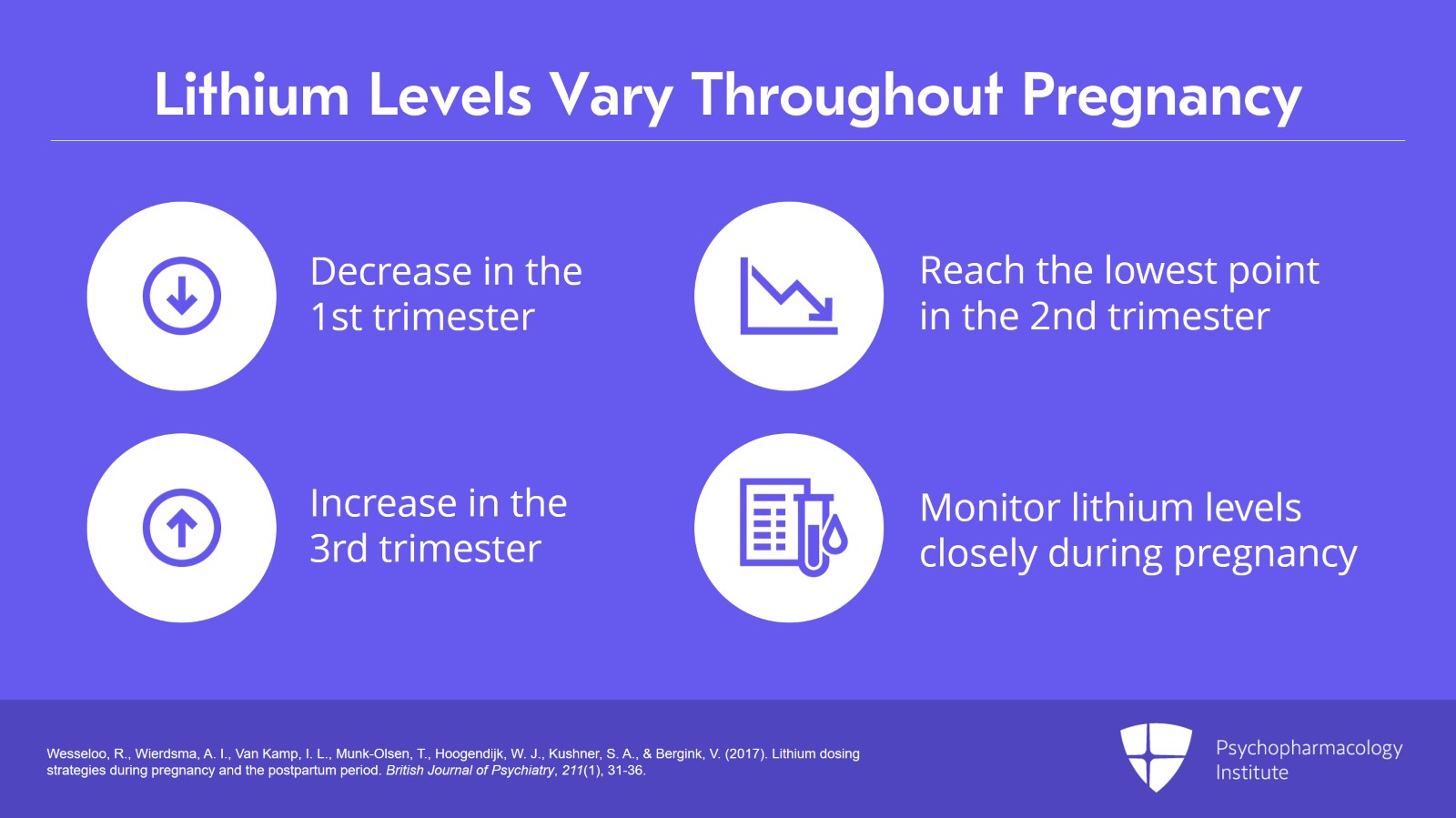
So lithium levels vary throughout pregnancy.
Lithium blood levels have been reported to decrease in the first trimester, reach a nadir or lowest point in the second trimester and they may increase in the third trimester.
Thus, monitoring of lithium levels needs to be done closely during pregnancy.
References:
- Wesseloo, R., Wierdsma, A. I., Van Kamp, I. L., Munk-Olsen, T., Hoogendijk, W. J., Kushner, S. A., & Bergink, V. (2017). Lithium dosing strategies during pregnancy and the postpartum period. British Journal of Psychiatry, 211(1), 31-36.
Slide 4 of 10
Remember our treatment in pregnancy principles. Preconception, to have a baseline lithium level, the lowest yet effective dose which maintains euthymia in a patient. If you can gather that, that’s going to be your target in pregnancy.
It’s also helpful to have a preconception TSH and renal function levels to compare during pregnancy as the pregnancy progresses. It’s also recommended starting b.i.d. dosing pre-pregnancy with the plan to reduce the amplitude or fluctuations of lithium levels during pregnancy as half of pregnancies are unexpected.
References:
- Wesseloo, R., Wierdsma, A. I., Van Kamp, I. L., Munk-Olsen, T., Hoogendijk, W. J., Kushner, S. A., & Bergink, V. (2017). Lithium dosing strategies during pregnancy and the postpartum period. British Journal of Psychiatry, 211(1), 31-36.
- Diav-Citrin, O., Shechtman, S., Tahover, E., Finkel-Pekarsky, V., Arnon, J., Kennedy, D., Erebara, A., Einarson, A., & Ornoy, A. (2014). Pregnancy outcome following in utero exposure to lithium: A prospective, comparative, observational study. American Journal of Psychiatry, 171(7), 785-794.
- Clark, C. T., & Wisner, K. L. (2018). Treatment of Peripartum bipolar disorder. Obstetrics and Gynecology Clinics of North America, 45(3), 403-417.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
During pregnancy, it’s important to be aware of the pharmacokinetic changes.
During pregnancy, lithium clearance increases 30% to 50% due to increased renal blood flow and glomerular filtration rate particularly in the last month of gestation. This causes plasma levels to fall substantially and increases the risk of maternal relapse.
At delivery, vascular volume rapidly decreases, and lithium clearance precipitously falls to pre-pregnancy levels.
So after birth, we have decrease in vascular volume and a decrease in lithium clearance.
References:
- Clark, C. T., & Wisner, K. L. (2018). Treatment of Peripartum bipolar disorder. Obstetrics and Gynecology Clinics of North America, 45(3), 403-417.
- Wesseloo, R., Wierdsma, A. I., Van Kamp, I. L., Munk-Olsen, T., Hoogendijk, W. J., Kushner, S. A., & Bergink, V. (2017). Lithium dosing strategies during pregnancy and the postpartum period. British Journal of Psychiatry, 211(1), 31-36.
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Slide 6 of 10
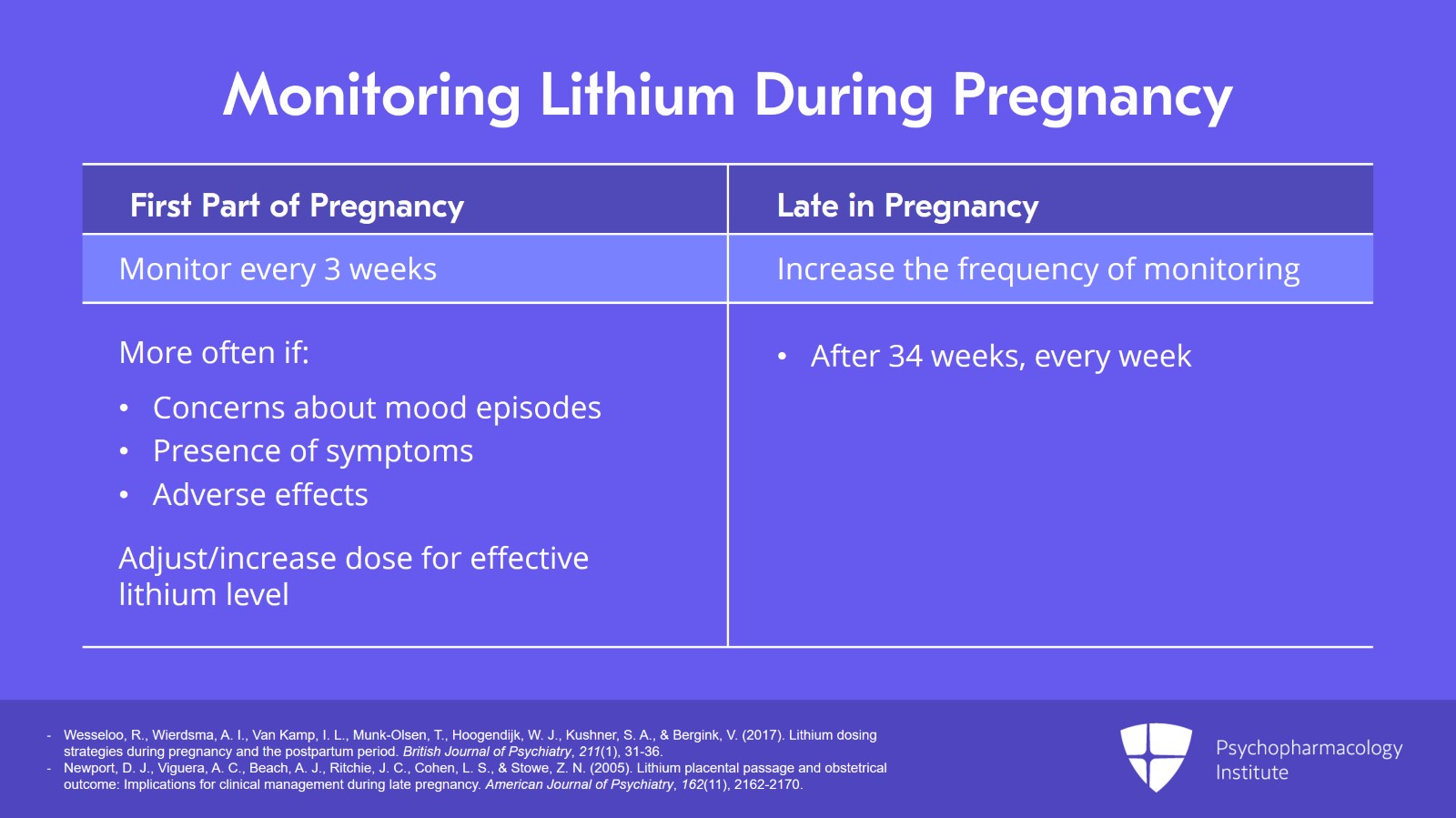
So it’s important to follow levels closely in pregnancy and recommendations are often every three weeks for the first part of pregnancy, certainly more often if there’s concern about a mood episode or symptoms coming on or adverse effects may be occurring.
And also to anticipate the need to adjust or increase dose during pregnancy to target that effective lithium level.
Late in pregnancy, increased frequency of monitoring. After 34 weeks, the goal of monitoring lithium every week to follow for those concentration or plasma level changes.
References:
- Wesseloo, R., Wierdsma, A. I., Van Kamp, I. L., Munk-Olsen, T., Hoogendijk, W. J., Kushner, S. A., & Bergink, V. (2017). Lithium dosing strategies during pregnancy and the postpartum period. British Journal of Psychiatry, 211(1), 31-36.
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
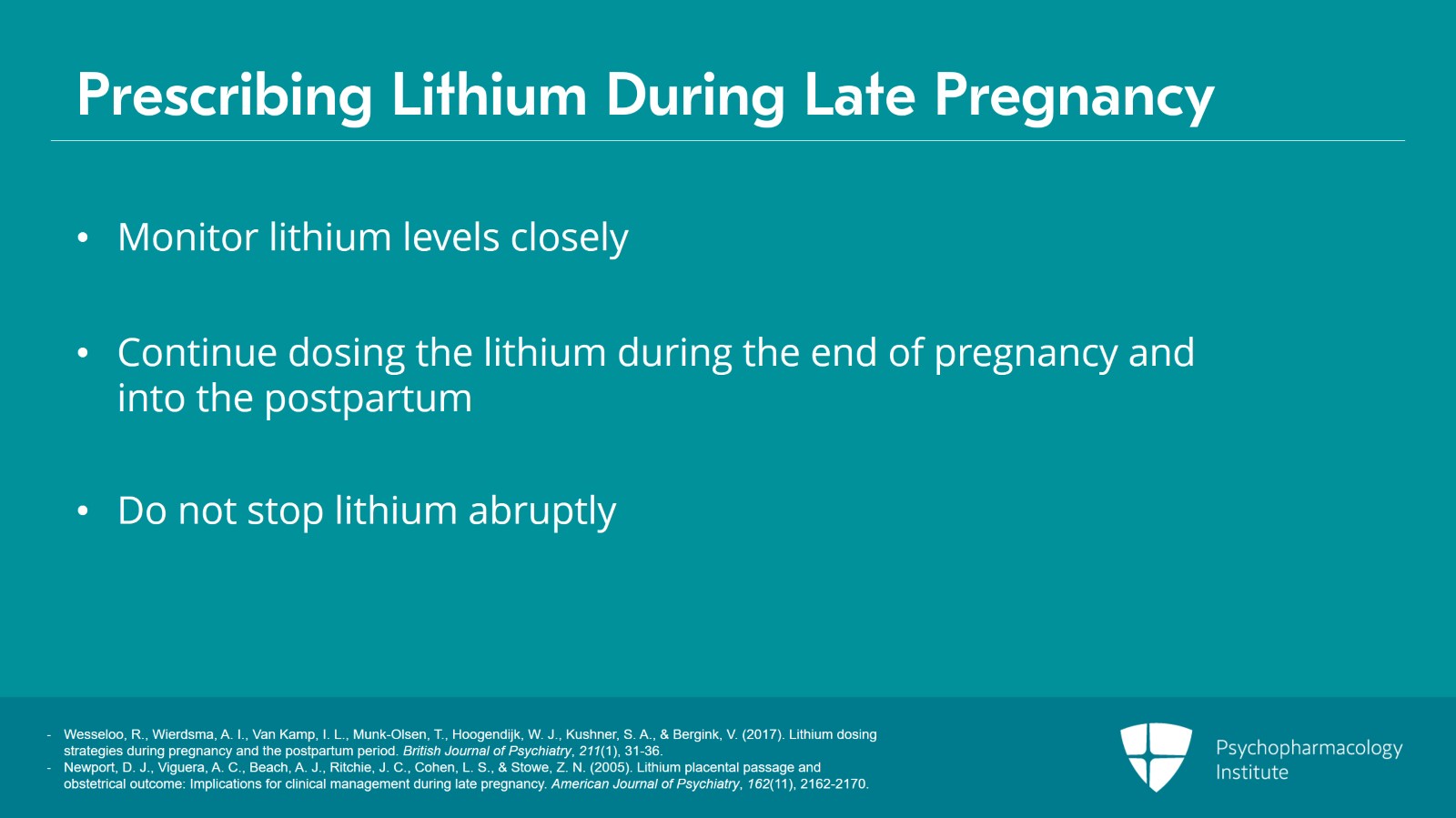
And historically, the thought was to hold or to stop the lithium prior to labor with the goal of reducing the risk of neonatal adjustment or floppy baby syndrome.
However, the newer proposition is to actually follow that lithium level very closely and to continue dosing as the mother enters the end of pregnancy and into the postpartum time. The reasoning behind this is that we know that maintaining euthymia in the mom benefits both the mom and the infant and this postpartum time is just such a high risk for a mood episode in bipolar disorder.
And here, we are with the idea of stopping the lithium abruptly can put the woman at an increased risk itself.
And there are some initial data saying that adjustment symptoms in the infant are not looking like they’re associated with ongoing sequelae. Again, these are earlier studies. But these are some of the risks to be weighing as you’re treating a woman going into labor and delivery.
References:
- Wesseloo, R., Wierdsma, A. I., Van Kamp, I. L., Munk-Olsen, T., Hoogendijk, W. J., Kushner, S. A., & Bergink, V. (2017). Lithium dosing strategies during pregnancy and the postpartum period. British Journal of Psychiatry, 211(1), 31-36.
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Slide 8 of 10
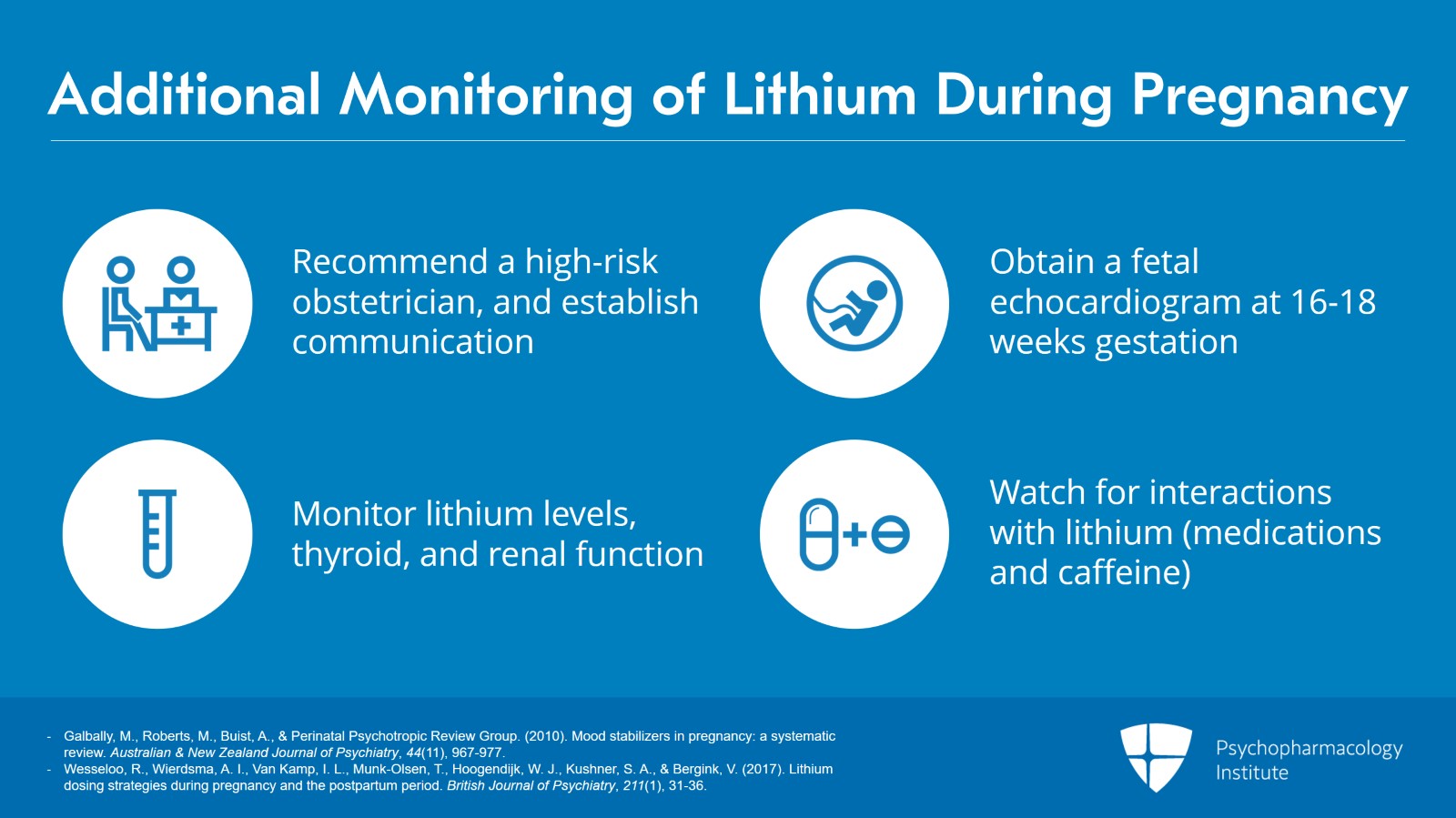
So also, thoughts on additional monitoring with lithium during pregnancy.
Definitely recommend a high-risk OB and getting release of information to communicate with that physician.
Obtaining a fetal echocardiogram or level 2 ultrasound at that 16 or 18 weeks’ gestational age. That’s under the purview of the OB.
And then monitoring for lithium serum levels as well as TSH, thyroid and renal function as the pregnancy progresses.
And don’t forget about interactions with lithium, that medication use can change in pregnancy and there’s increase in lithium levels if the woman starts using NSAIDs or diuretics or ACE inhibitors and then a decrease in lithium levels — Primarily watch for the caffeine. With the sleep disruption and exhaustion that can come with pregnancy, women may be using more caffeine to counteract that.
References:
- Galbally, M., Roberts, M., Buist, A., & Perinatal Psychotropic Review Group. (2010). Mood stabilizers in pregnancy: a systematic review. Australian & New Zealand Journal of Psychiatry, 44(11), 967-977.
- Wesseloo, R., Wierdsma, A. I., Van Kamp, I. L., Munk-Olsen, T., Hoogendijk, W. J., Kushner, S. A., & Bergink, V. (2017). Lithium dosing strategies during pregnancy and the postpartum period. British Journal of Psychiatry, 211(1), 31-36.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
Our key points in using lithium in pregnancy.
So while management of lithium in pregnancy needs to be rigorous and use of lithium is not without risks, stick to your guiding principles.
Our goal is to have the woman doing well, use the lowest effective dose and work with close monitoring for lithium in pregnancy with the guideline of every three weeks until week 34 and then every week after that to assess for your need to adjust dose.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.