Slides and Transcript
Slide 1 of 15
Next, we’re moving on to considerations for using antipsychotics in the geriatric population.
Slide 2 of 15
We know that antipsychotics come with a variety of adverse effects. So some of these medications can cause alpha blockade, which can lead to orthostatic hypotension. That could be medications like quetiapine or clozapine.
References:
- Holder, S. D., & Wayhs, A. (2014). Schizophrenia. American Family Physician, 90(11), 775-782.
- Masand, P. S. (2000). Side effects of antipsychotics in the elderly. The Journal of Clinical Psychiatry, 61(Suppl 8), 43-51.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
Medications can also have significant extrapyramidal side effects related to the D2 blockade, which can lead to gait disturbances, motor stiffness, tremor, akathisia, and tardive dyskinesia. A lot of these medications have antimuscarinic properties, which can lead to anticholinergic side effects.
References:
- Holder, S. D., & Wayhs, A. (2014). Schizophrenia. American Family Physician, 90(11), 775-782.
- Masand, P. S. (2000). Side effects of antipsychotics in the elderly. The Journal of Clinical Psychiatry, 61(Suppl 8), 43-51.
Slide 4 of 15
They can have antihistaminergic properties, which can lead to sedation, weight gain, the metabolic syndrome, as well as related to the antimuscarinic effects can lead to arrhythmia and QT prolongation. There’s also an increased risk of vascular events or stroke with these medications as well.
References:
- Holder, S. D., & Wayhs, A. (2014). Schizophrenia. American Family Physician, 90(11), 775-782.
- Masand, P. S. (2000). Side effects of antipsychotics in the elderly. The Journal of Clinical Psychiatry, 61(Suppl 8), 43-51.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
When we look at the cumulative annual incidence of tardive dyskinesia with conventional antipsychotics, we know that use of these medications in older adults is associated with a higher risk of tardive dyskinesia. So these extrapyramidal side effects or tardive dyskinesia are more likely to happen with older adults.
References:
- Holder, S. D., & Wayhs, A. (2014). Schizophrenia. American Family Physician, 90(11), 775-782.
- Jeste, D. V., Caligiuri, M. P., Paulsen, J. S., Heaton, R. K., Lacro, J. P., Harris, M. J., Bailey, A., Fell, R. L., & McAdams, L. A. (1995). Risk of tardive dyskinesia in older patients. A prospective longitudinal study of 266 outpatients. Archives of General Psychiatry, 52(9), 756–765. https://doi.org/10.1001/archpsyc.1995.03950210050010
- Masand, P. S. (2000). Side effects of antipsychotics in the elderly. The Journal of Clinical Psychiatry, 61(Suppl 8), 43-51.
Slide 6 of 15
The starting doses for these medications, we’re generally going to use about a quarter to half of the typical starting dose and titrate up. For antidepressants, we say start low, go slow and don’t stop. In the case of antipsychotics, we might think about start low, go slow and maybe stop especially in the setting of dementia.
References:
- Holder, S. D., & Wayhs, A. (2014). Schizophrenia. American Family Physician, 90(11), 775-782.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
In dementia, we know that there is a black box warning for antipsychotics and that they’re associated with increased mortality when used for the treatment of behavioral disorders in elderly patients with dementia. This is based on an analysis of 17 placebo-controlled trials with olanzapine, quetiapine, risperidone, and aripiprazole. And they found that use of these medications is associated with a 1.6 to 1.7-fold increase in mortality. And we know that these medications can be very helpful for some patients with behavioral disturbances in dementia, but they do come with this mortality side effect and risk. And that’s generally due to cardiac risk, a stroke, or an aspiration event like an aspiration pneumonia.
References:
- Kales, H. C., Valenstein, M., Kim, H. M., McCarthy, J. F., Ganoczy, D., Cunningham, F., & Blow, F. C. (2007). Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. The American Journal of Psychiatry, 164(10), 1568-1623. https://doi.org/10.1176/appi.ajp.2007.06101710
- Carson, S., McDonagh, M. S., & Peterson, K. (2006). A systematic review of the efficacy and safety of atypical antipsychotics in patients with psychological and behavioral symptoms of dementia. Journal of the American Geriatrics Society, 54(2), 354–361. https://doi.org/10.1111/j.1532-5415.2005.00566.x
Slide 8 of 15
There are several studies that have been done that looked at the number needed to harm, and harm in this study in particular is the risk of death at six months. And compared to non-antipsychotic users, patients with dementia who were newly initiated on antipsychotics, it only takes 8 patients treated with haloperidol before 1 death.
References:
- Maust, D. T., Kim, H. M., Seyfried, L. S., Chiang, C., Kavanagh, J., Schneider, L. S., & Kales, H. C. (2015). Antipsychotics, other psychotropics, and the risk of death in patients with dementia: Number needed to harm. JAMA Psychiatry, 72(5), 438–445. https://doi.org/10.1001/jamapsychiatry.2014.3018
- Carson, S., McDonagh, M. S., & Peterson, K. (2006). A systematic review of the efficacy and safety of atypical antipsychotics in patients with psychological and behavioral symptoms of dementia. Journal of the American Geriatrics Society, 54(2), 354–361. https://doi.org/10.1111/j.1532-5415.2005.00566.x
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
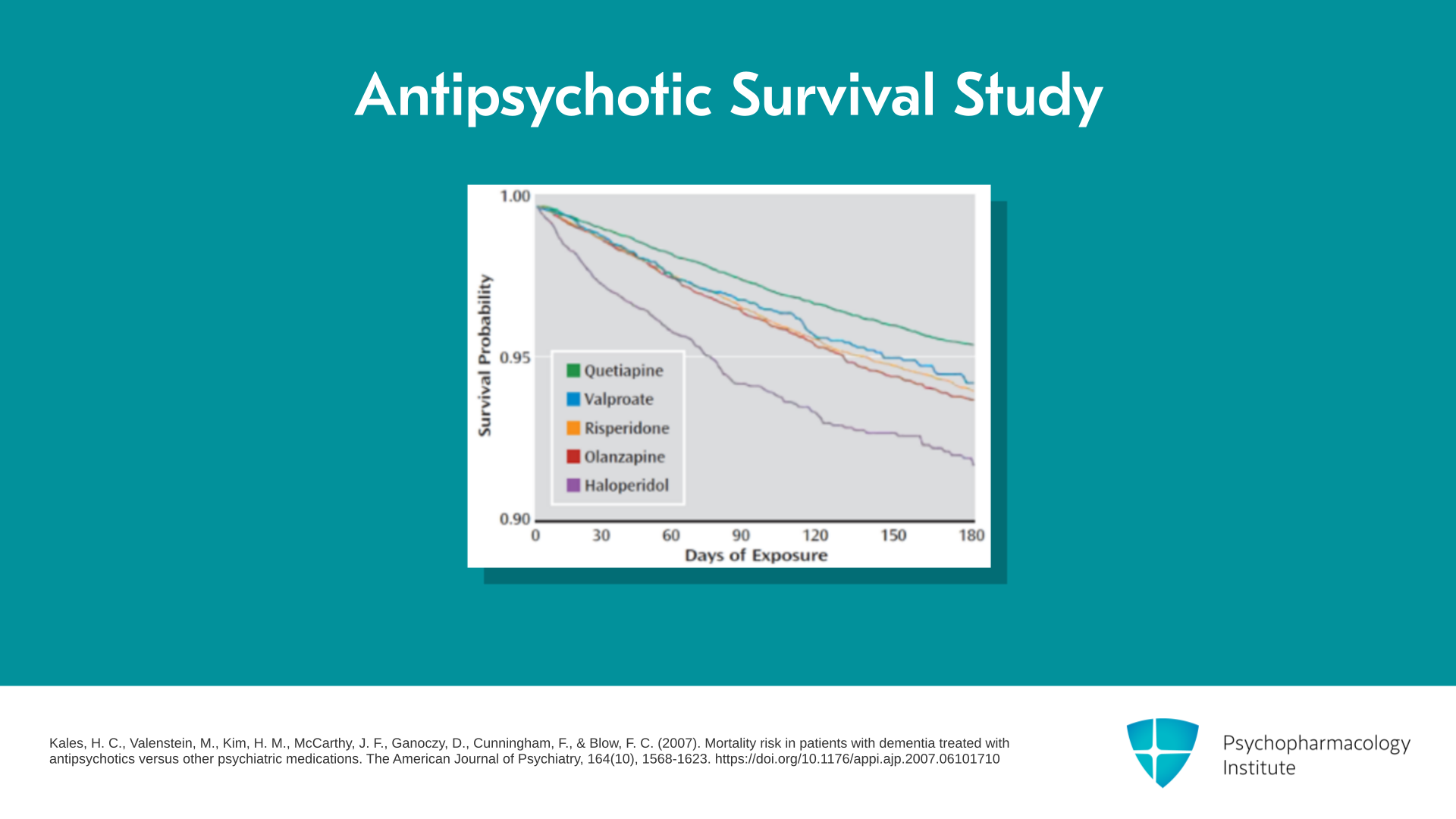
In a study done by Helen Kales, it looked at survival after being newly exposed to an antipsychotic medication and you can see these survival curves all going down after initiation. A little bit worse for medications like haloperidol and olanzapine. Maybe a little bit better with medications like quetiapine.
References:
- Kales, H. C., Valenstein, M., Kim, H. M., McCarthy, J. F., Ganoczy, D., Cunningham, F., & Blow, F. C. (2007). Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. The American Journal of Psychiatry, 164(10), 1568-1623. https://doi.org/10.1176/appi.ajp.2007.06101710
Slide 10 of 15
I’ll mention a couple of unique antipsychotics as it relates to prescribing in older adults. Pimavanserin or Nuplazid is an atypical antipsychotic indicated for treatment of hallucinations and delusions associated with Parkinson’s disease psychosis. It’s an inverse agonist and also has antagonist activity at the serotonin receptor, and has very little to no D2 blockade. It still carries the black box warning for increased mortality in dementia and also can cause QT prolongation. Common side effects include GI symptoms, peripheral edema, and confusion.
References:
- Cummings, J., Ballard, C., Tariot, P., Owen, R., Foff, E., Youakim, J., Norton, J., & Stankovic, S. (2018). Pimavanserin: Potential treatment for dementia-related psychosis. The Journal of Prevention of Alzheimer's Disease, 5(4), 253–258. https://doi.org/10.14283/jpad.2018.29
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
And some people might ask, are there any advantages to using pimavanserin over quetiapine in the treatment of hallucinations associated with Parkinson’s disease? And I think it can be helpful for patients who still develop extrapyramidal side effects with quetiapine or have excessive sedation with that medication. It also avoids the blood monitoring required with Clozaril.
References:
- Cummings, J., Ballard, C., Tariot, P., Owen, R., Foff, E., Youakim, J., Norton, J., & Stankovic, S. (2018). Pimavanserin: Potential treatment for dementia-related psychosis. The Journal of Prevention of Alzheimer's Disease, 5(4), 253–258. https://doi.org/10.14283/jpad.2018.29
Slide 12 of 15
Another medication is brexpiprazole or Rexulti, which is an atypical antipsychotic that was recently approved by the US FDA in May 2023 and became the first FDA-approved medication for treatment of agitation associated with Alzheimer’s disease. This is a medication that is quite pricey, it can cost about $1400 per month. I will mention that the studies that were done looked at a change in the Cohen-Mansfield Agitation Inventory score and found that it had about a 5-point improvement over placebo. This is a scale though that goes from 0 to 203. So a statistically significant improvement but unclear on the clinical improvement.
References:
- Whitaker, R. (2023). How the FDA approved an antipsychotic that failed to show a meaningful benefit but raised the risk of death. BMJ (Clinical Research Ed.), 382, Article 1801. https://doi.org/10.1136/bmj.p1801
- Lee, D., Slomkowski, M., Hefting, N., Chen, D., Larsen, K. G., Kohegyi, E., Hobart, M., Cummings, J. L., & Grossberg, G. T. (2023). Brexpiprazole for the treatment of agitation in Alzheimer dementia: A randomized clinical trial. JAMA Neurology, 80(12), 1307-1316. https://doi.org/10.1001/jamaneurol.2023.3810
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
So thinking about how that compares to some of the antipsychotics that are used to treat behavioral disturbances in dementia but are not FDA approved, that 5-point improvement is no better than the other medications. And in fact, it may be actually worse than some of the data that we have for risperidone. This medication still carries a black box warning for increased mortality in dementia, and in these studies, the risk of death was about 4 times higher in patients taking brexpiprazole versus placebo over a 16-week period. These medications are also associated with QTc prolongation as well.
References:
- Whitaker, R. (2023). How the FDA approved an antipsychotic that failed to show a meaningful benefit but raised the risk of death. BMJ (Clinical Research Ed.), 382, Article 1801. https://doi.org/10.1136/bmj.p1801
- Lee, D., Slomkowski, M., Hefting, N., Chen, D., Larsen, K. G., Kohegyi, E., Hobart, M., Cummings, J. L., & Grossberg, G. T. (2023). Brexpiprazole for the treatment of agitation in Alzheimer dementia: A randomized clinical trial. JAMA Neurology, 80(12), 1307-1316. https://doi.org/10.1001/jamaneurol.2023.3810
Slide 14 of 15
So some key points for this section: Antipsychotics come with a host of side effects including metabolic side effects, QT prolongation and motor disturbances that need to be monitored. Antipsychotics are associated with an increased risk of mortality when used to treat dementia-related psychosis.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 15
Pimavanserin is a novel antipsychotic indicated to treat psychosis associated with Parkinson’s disease but it carries the same black box warning for increased mortality risk. Brexpiprazole is the first antipsychotic approved by the US Food and Drug Administration for treatment of agitation associated with Alzheimer’s disease. However, the treatment effect is modest.