Slides and Transcript
Slide 2 of 9
Postpartum psychosis is generally considered a rare condition occurring among every 1 to 2 out of 1000 pregnancies. But considering the number of pregnancies that occur within the US each year, it represents a large number of women who are at risk for this very serious illness. It generally has a rapid dramatic onset within the first two weeks of delivery but can sometimes occur later on. And there’s a very high risk of harm to the woman and to her baby in the case of postpartum psychosis. So it’s very important that cases are identified as early as possible and that women are hospitalized for treatment and assessment.
References:
- Nonacs, R., & Cohen, L. S. (1998). Postpartum mood disorders: diagnosis and treatment guidelines. The Journal of Clinical Psychiatry.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 9
The diagnosis that’s most associated with postpartum psychosis is bipolar disorder.
We suspect bipolar disorder as the underlying etiology for a postpartum psychotic episode whether or not a woman has had a history of it before and that’s really important in terms of treatment considerations.
So for the majority of women, it will be an affective disorder. Bipolar disorder is schizoaffective. And risk factors for postpartum psychosis include a history of postpartum psychosis, it’s a highly recurrent condition, having had psychosis before, a diagnosis of bipolar disorder and also previous psychiatric hospitalizations even if not for psychosis.
References:
- Jones, I., & Craddock, N. (2001). Familiality of the puerperal trigger in bipolar disorder: results of a family study. American Journal of Psychiatry, 158(6), 913-917.
Slide 4 of 9
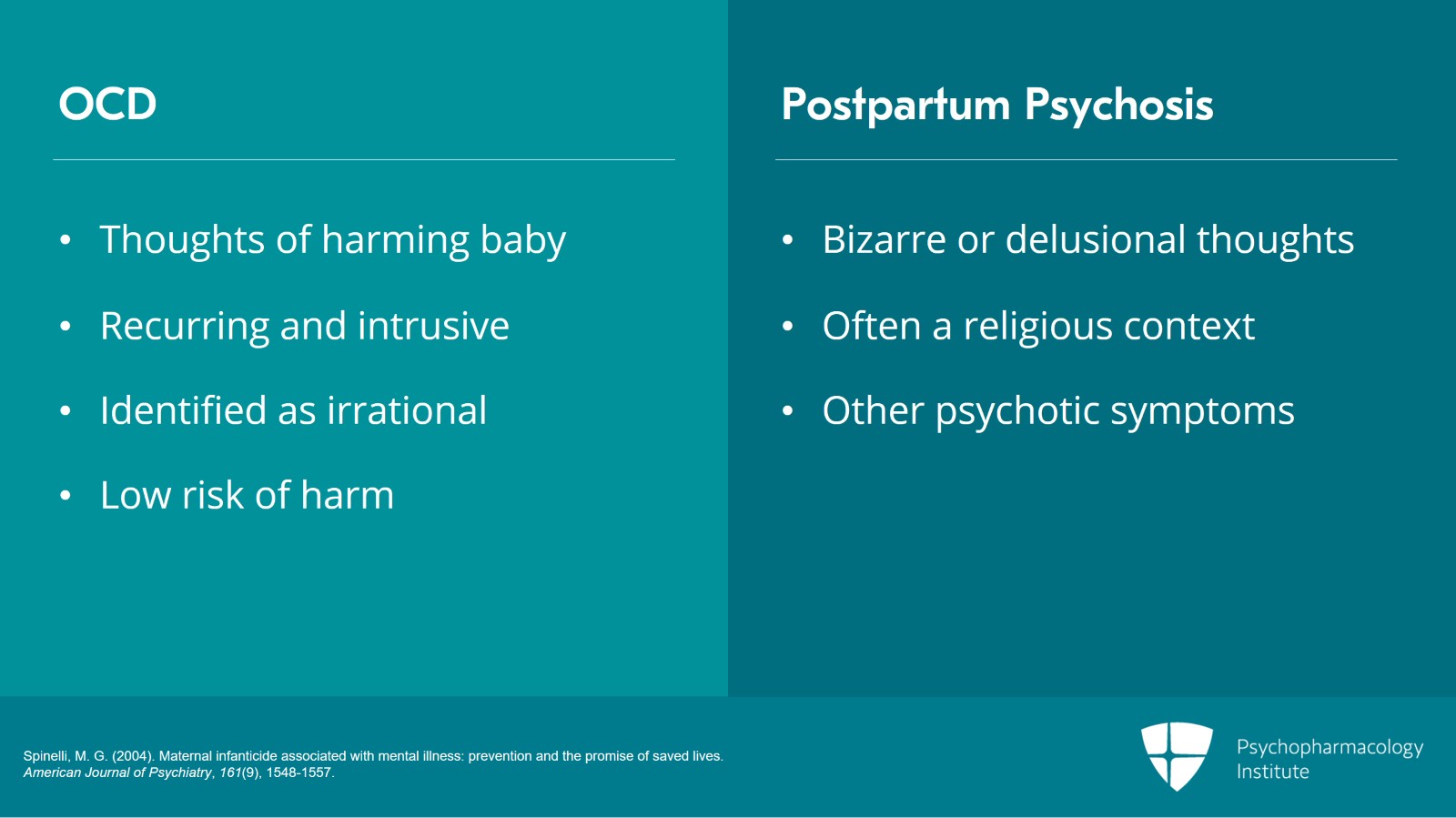
On the frontlines, for example, in an emergency room setting, it can be difficult to differentiate obsessive-compulsive disorder in the postpartum and psychosis. So if women present specifically with disturbing thoughts about harming the baby, this may require some differentiation because most of the time when women have disturbing thoughts about harming the baby, it goes along with an OCD diagnosis. So when women experience obsessions in the postpartum, they typically are very textbook in terms of the diagnosis of obsession, so recurrent disturbing intrusive thoughts that women can’t stop having even though they know they aren’t rational. So women are generally very bothered by these thoughts. They’re frightened. Sometimes, they’re very ashamed. Sometimes, they avoid being alone with their baby. But it’s important to know that these kinds of thoughts are very common and get better with treatment. And there’s actually a very low risk of harm to the baby.
Now, this is in sharp contrast with postpartum psychosis where women may have thoughts of harming the baby but the quality of those thoughts is notably different. So women with postpartum psychosis are experiencing by definition a break with reality and may have bizarre or delusional thoughts about the baby or about what harming the baby might mean. So for example, there might be altruistic delusions about harming the baby. It may actually be saving the baby. Very often, there’s a religious context to the delusions. And generally, women don’t report that these are egodystonic or disturbing thoughts the way that they would report obsessions being experienced that way. Now, postpartum psychosis and thoughts like that generally occur in the context of other symptoms. So women may be having hallucinations. They may be having other delusions. But very often, the delusions do take form around the baby and the baby is at grave risk if a mom has postpartum psychosis. Women with postpartum psychosis are also at risk of harming themselves or other children in the household.
References:
- Spinelli, M. G. (2004). Maternal infanticide associated with mental illness: prevention and the promise of saved lives. American Journal of Psychiatry, 161(9), 1548-1557.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 9
Now, although postpartum psychosis is not common, it can be the first episode of a psychiatric disorder. And so the family and the friends around the new mother may not know what’s going on and may delay in seeking treatment. But it’s very important that if a woman is found to have any symptoms of postpartum psychosis that she is brought to care immediately. It’s generally recommended that women go for hospitalization or present to an emergency room. And postpartum psychosis is definitely a psychiatric emergency. And it’s estimated that women with postpartum psychosis commit infanticide at a rate of about 4%. And it’s really actually just an estimate because rates are hard to estimate as postpartum psychosis itself may be underestimated as are cases of harm to the baby or the mother. But importantly, it is an emergency and inpatient care is recommended.
References:
- Spinelli, M. G. (2004). Maternal infanticide associated with mental illness: prevention and the promise of saved lives. American Journal of Psychiatry, 161(9), 1548-1557.
Slide 6 of 9
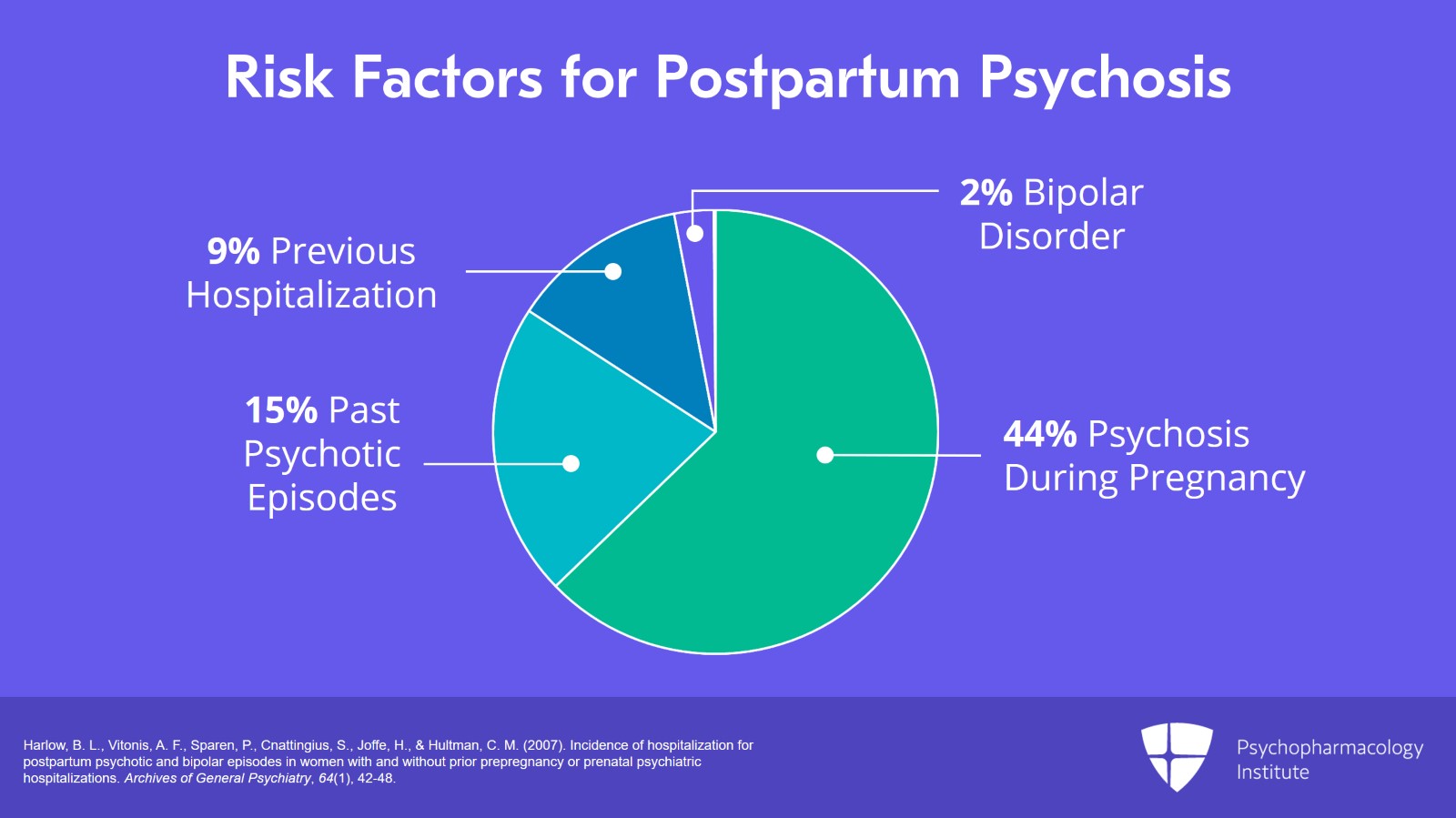
So some of the risk factors specifically studied and looked at in terms of quantifiable risk include hospitalization for a psychotic episode during the pregnancy. That’s associated with a very high risk of 44% risk of postpartum psychosis.
Hospitalization for a past psychotic episode is associated with an almost 15% risk of postpartum psychosis.
Any previous psychiatric hospitalization is at a rate of about 9%.
Previous hospitalization for bipolar disorder 2%.
And this is all in contrast to the baseline population risk which is less than 0.1%.
References:
- Harlow, B. L., Vitonis, A. F., Sparen, P., Cnattingius, S., Joffe, H., & Hultman, C. M. (2007). Incidence of hospitalization for postpartum psychotic and bipolar episodes in women with and without prior prepregnancy or prenatal psychiatric hospitalizations. Archives of General Psychiatry, 64(1), 42-48.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 9
And it’s important if we can identify those women during pregnancy that we can educate women and their families about the risk for postpartum psychosis.
So because psychosis involves a lack of good insight, it’s very important that family members or friends that are close to the woman are educated about the disorder so that they can help her seek treatment at the immediate onset of a postpartum psychotic episode.
References:
- Spinelli, M. G. (2009). Postpartum psychosis: detection of risk and management. American Journal of Psychiatry, 166(4), 405-408.
Slide 8 of 9
So some of the key points about postpartum psychosis is that it is indeed a psychiatric emergency requiring hospitalization for safety. And although it’s rare at baseline, there are psychiatric factors that increase risk substantially. And in many cases, we can identify the women who would be at greatest risk.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.