Slides and Transcript
Slide 1 of 9
Let’s talk now about the pharmacotherapy for insomnia remembering that in general pharmacotherapy is prescribed on a short-term basis depending upon the clinical presentation and is often co-prescribed with behavioral treatments or cognitive behavioral treatments for insomnia as an adjunct to behavioral management.
Slide 2 of 9
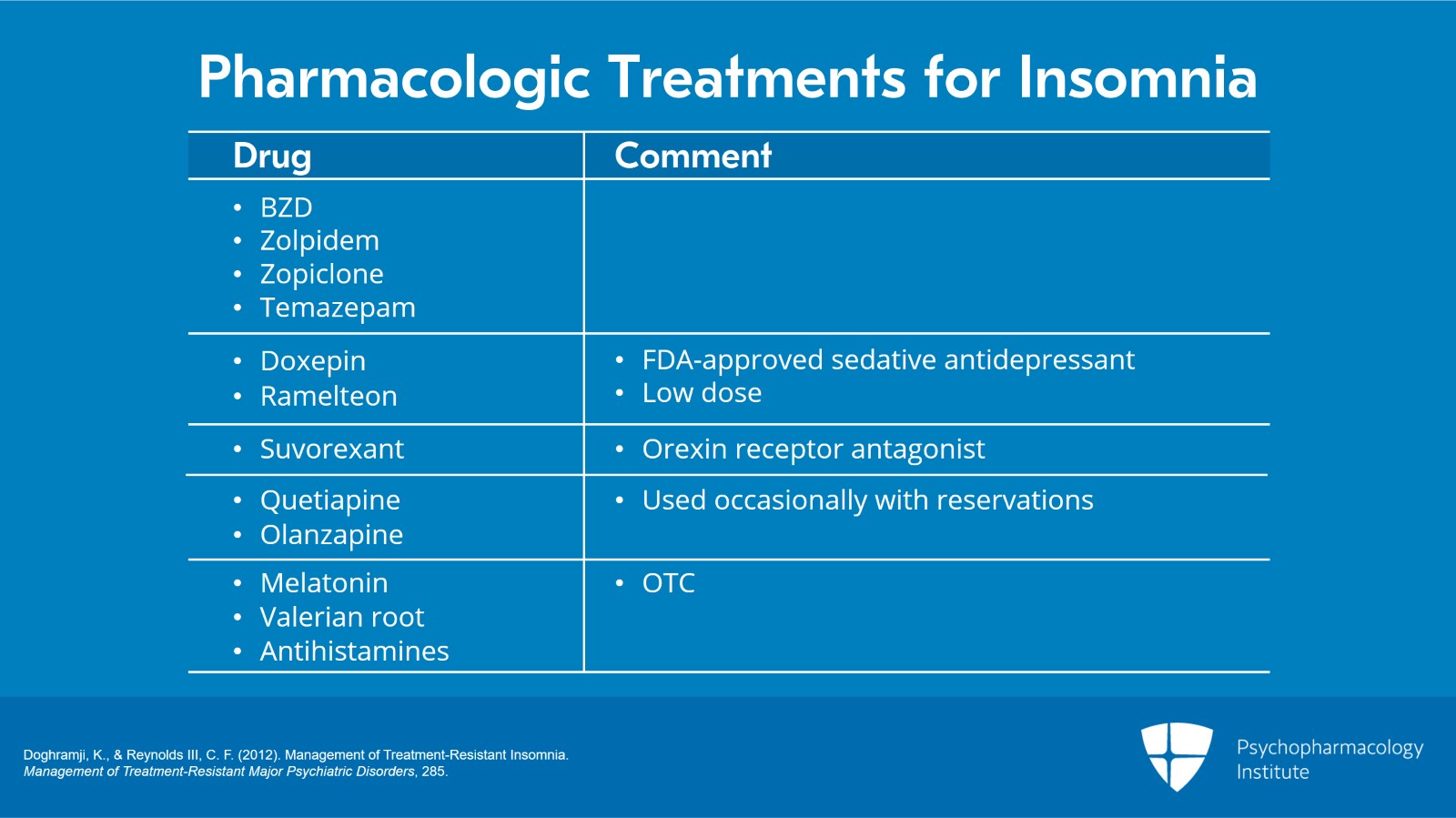
There are several classes of pharmacological treatments for insomnia disorder ranging from benzodiazepine receptor agonists and the so-called Z-drugs like zolpidem or zopiclone, other benzodiazepines specifically for insomnia such as temazepam.
There are also FDA-approved sedative antidepressants such as doxepin and low-dose ramelteon and a newer agent, suvorexant, which is an orexin receptor antagonist.
Sedating antipsychotic medications like quetiapine or olanzapine are occasionally used but many of us have significant reservations about the use of sedating antipsychotic agents and I’ll talk a bit more about that momentarily. Pay attention also to any OTC, over-the-counter, medications that your patient may be using such as melatonin, valerian root or antihistamines like diphenhydramine.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 9
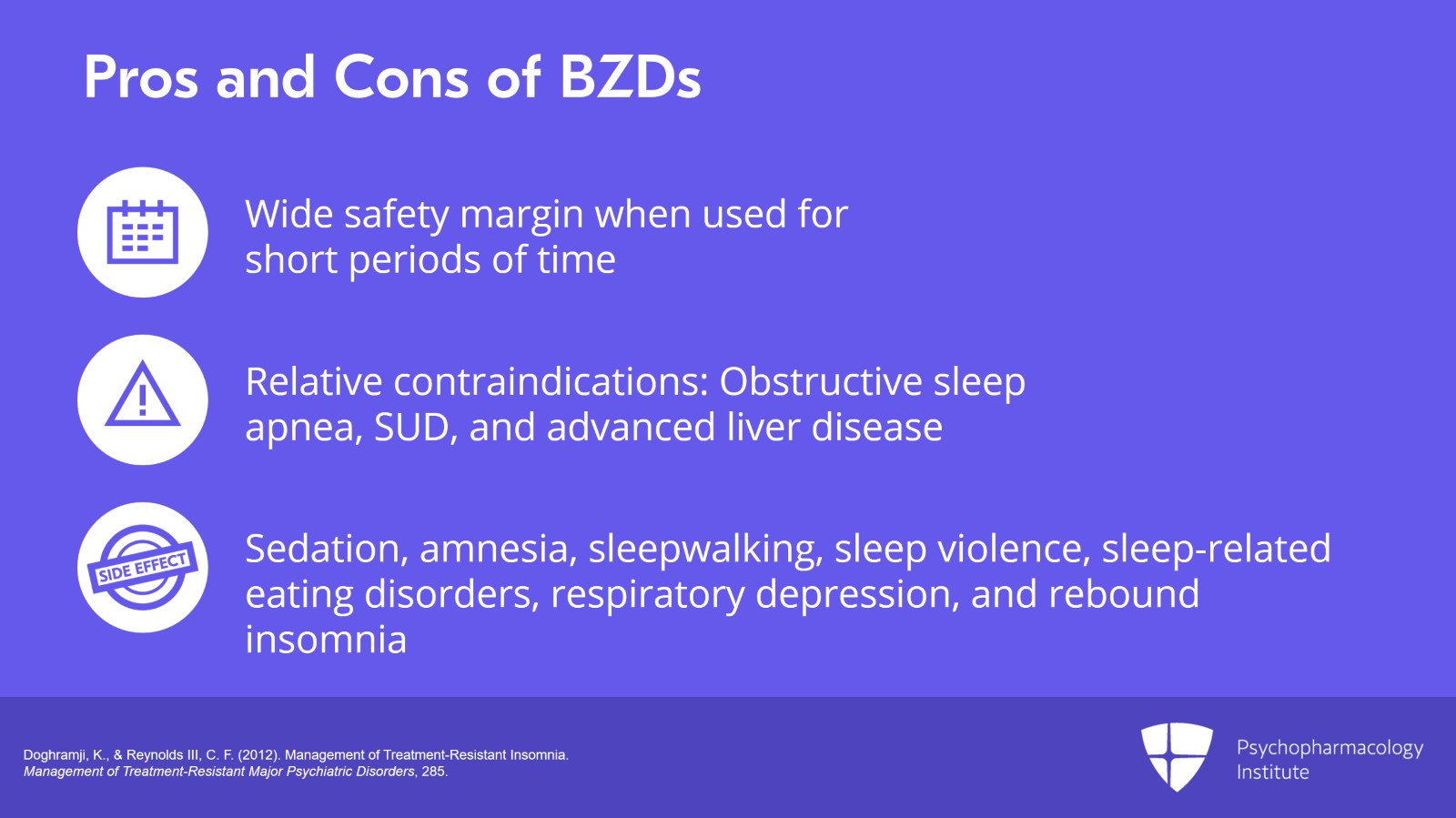
Let’s talk a little bit about each of these classes and their positives and negatives if you will. With respect to the use of benzodiazepines for a short period of time, in general, their margin of safety is wide. They are relatively contraindicated in patients who have obstructive sleep apnea or substance use disorders or advanced liver disease. Be mindful of the adverse side effects of benzodiazepine usage including excessive sedation during the day, anterograde amnesia, some instances of sleepwalking and sleep violence, sleep-related eating disorders and respiratory depression as well as rebound insomnia after their use is discontinued.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285.
Slide 4 of 9
Sedative antidepressants include the FDA-approved agent doxepin and trazodone. These are helpful in patients with co-occurring depression. And as I’ve mentioned, doxepin is FDA approved for sleep maintenance insomnia generally in low doses in the ballpark of 5 to 10 mg.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 9
Suvorexant is a newer agent on the market. It’s a dual orexin receptor antagonist.
And in placebo-controlled clinical trials in adults and in older patients, it’s been found to decrease sleep latency and the amount of wake time after sleep onset.
It increases overall sleep efficiency and sleep time with little evidence of tolerance or rebound.
The usual dose of suvorexant is 10 to 20 mg at the hour of sleep. Its main side effect is excessive sleepiness in a small percentage of patients.
References:
- Herring, W. J., Snyder, E., Budd, K., Hutzelmann, J., Snavely, D., Liu, K., … & Michelson, D. (2012). Orexin receptor antagonism for treatment of insomnia: a randomized clinical trial of suvorexant. Neurology, 79(23), 2265-2274.
Slide 6 of 9
Ramelteon is the first melatonin receptor agonist approved for the treatment of insomnia. Generally valuable in my experience in patients having difficulty falling asleep. It should not be used concurrently with fluvoxamine or severe liver failure.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 9
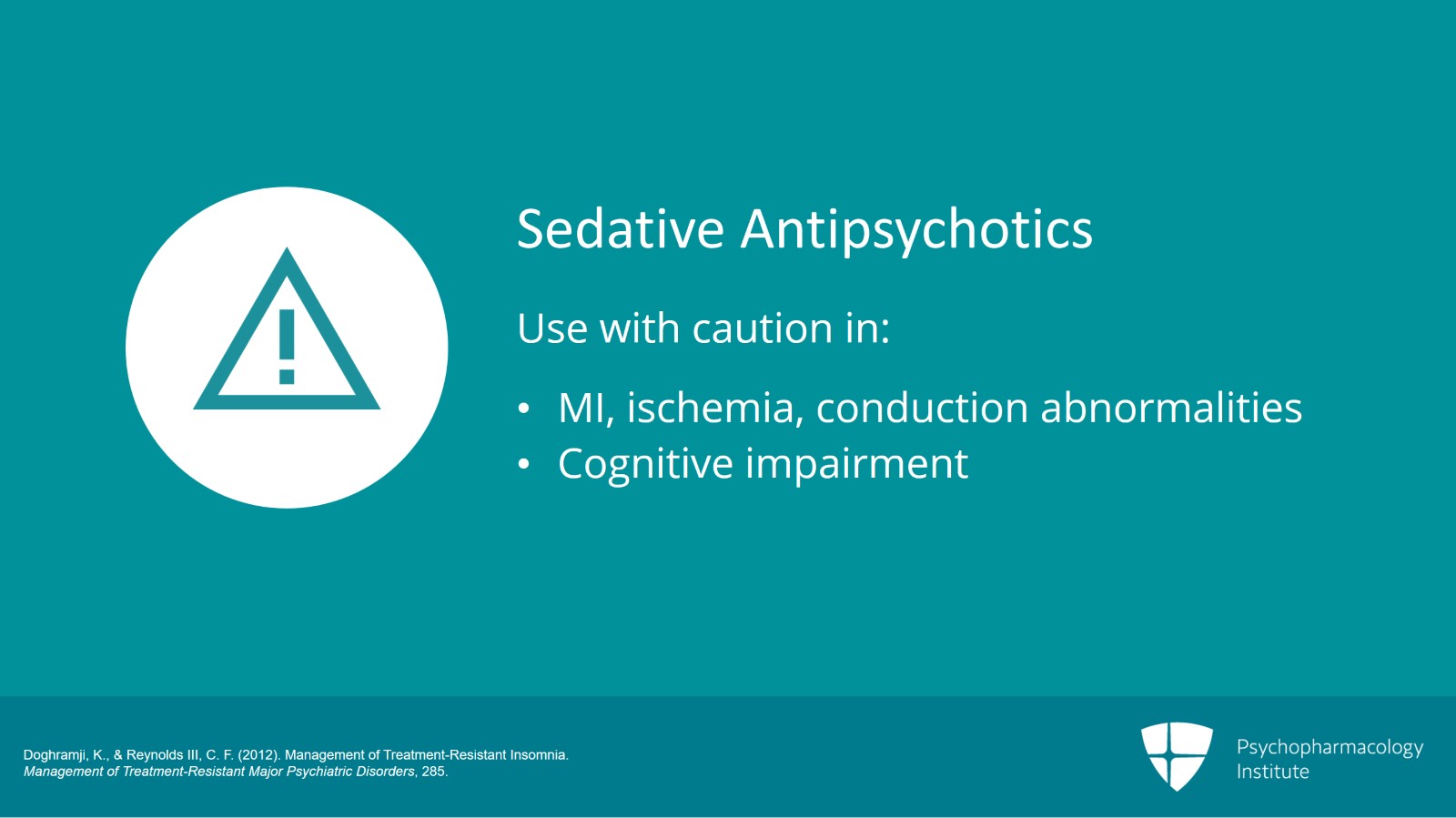
I don’t recommend the use of sedative antipsychotics like quetiapine or olanzapine in patients with sleep issues and they need to be used obviously cautiously in patients with MI, ischemia, conduction abnormalities or cognitive impairment particularly those with dementia.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285.
Slide 8 of 9
Some key take home points here about the pharmacotherapy of insomnia. Ramelteon may be particularly useful in patients with difficulty falling asleep.
Suvorexant may work by a different mechanism of action, orexin receptor antagonism, and appears to be helpful in reducing intermittent wakefulness, wake time after sleep onset but a small percentage of patients do experience daytime sleepiness as a side effect.
With respect to risk-benefit ratio, I do not recommend the use of sedative antipsychotics because of the issues of safety particularly in older adults and those living with dementia.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.