Slides and Transcript
Slide 2 of 20
Stimulants are the most used and considered the most effective medications for the treatment of ADHD both in children and adolescents as well as for the treatment of adults with ADHD.
References:
- Santos, G. M., Santos, E. M., Mendes, G. D., Fragoso, Y. D., Souza, M. R., & Martimbianco, A. L. C. (2021). A review of Cochrane reviews on pharmacological treatment for attention deficit hyperactivity disorder. Dementia & Neuropsychologia, 15(4), 421–427.
- Chaulagain, A., Lyhmann, I., Halmøy, A., et al. (2023). A systematic meta-review of systematic reviews on attention deficit hyperactivity disorder. European Psychiatry, 66(1), e90.
- Madaan, V., Kinnan, S., Daughton, J., & Kratochvil, C. J. (2006). Innovations and recent trends in the treatment of ADHD. Expert review of neurotherapeutics, 6(9), 1375-1385.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 20
Psychostimulants including amphetamines and methylphenidate are a broad class of sympathomimetic drugs. They increase not only movement but arousal, vigilance, wakefulness and attention. Some are considered drugs of abuse such as cocaine. Others are socially acceptable such as caffeine. But we're focused on the therapeutic drugs and again those are amphetamine, methylphenidate, and modafinil. These, at least the former two amphetamines and methylphenidates, have received indications by the FDA through a number of randomized clinical trials.
References:
- Santos, G. M., Santos, E. M., Mendes, G. D., Fragoso, Y. D., Souza, M. R., & Martimbianco, A. L. C. (2021). A review of Cochrane reviews on pharmacological treatment for attention deficit hyperactivity disorder. Dementia & Neuropsychologia, 15(4), 421–427.
- Chaulagain, A., Lyhmann, I., Halmøy, A., et al. (2023). A systematic meta-review of systematic reviews on attention deficit hyperactivity disorder. European Psychiatry, 66(1), e90.
- Madaan, V., Kinnan, S., Daughton, J., & Kratochvil, C. J. (2006). Innovations and recent trends in the treatment of ADHD. Expert review of neurotherapeutics, 6(9), 1375-1385.
Slide 4 of 20
Now, we've been using stimulants for a long time and even a long time in adults and prescribing patterns have changed. For instance, amphetamine is now prescribed over methylphenidate, something that would be hard to know 30 years ago when methylphenidate had a large lead over amphetamines. Adults now exceed children in the proportion of prescribed stimulants. Adult women are more likely to receive stimulants than adult men.
References:
- Asherson, P., Buitelaar, J., Faraone, S. V., & Rohde, L. A. (2016). Adult attention-deficit hyperactivity disorder: Key conceptual issues. The Lancet Psychiatry, 3(6), 568-578.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 20
And not surprisingly, there have been a large increase in the number of stimulants prescribed for any group. Long-acting stimulants are seen for use more in children and adolescents than in adults.
References:
- Asherson, P., Buitelaar, J., Faraone, S. V., & Rohde, L. A. (2016). Adult attention-deficit hyperactivity disorder: Key conceptual issues. The Lancet Psychiatry, 3(6), 568-578.
Slide 6 of 20
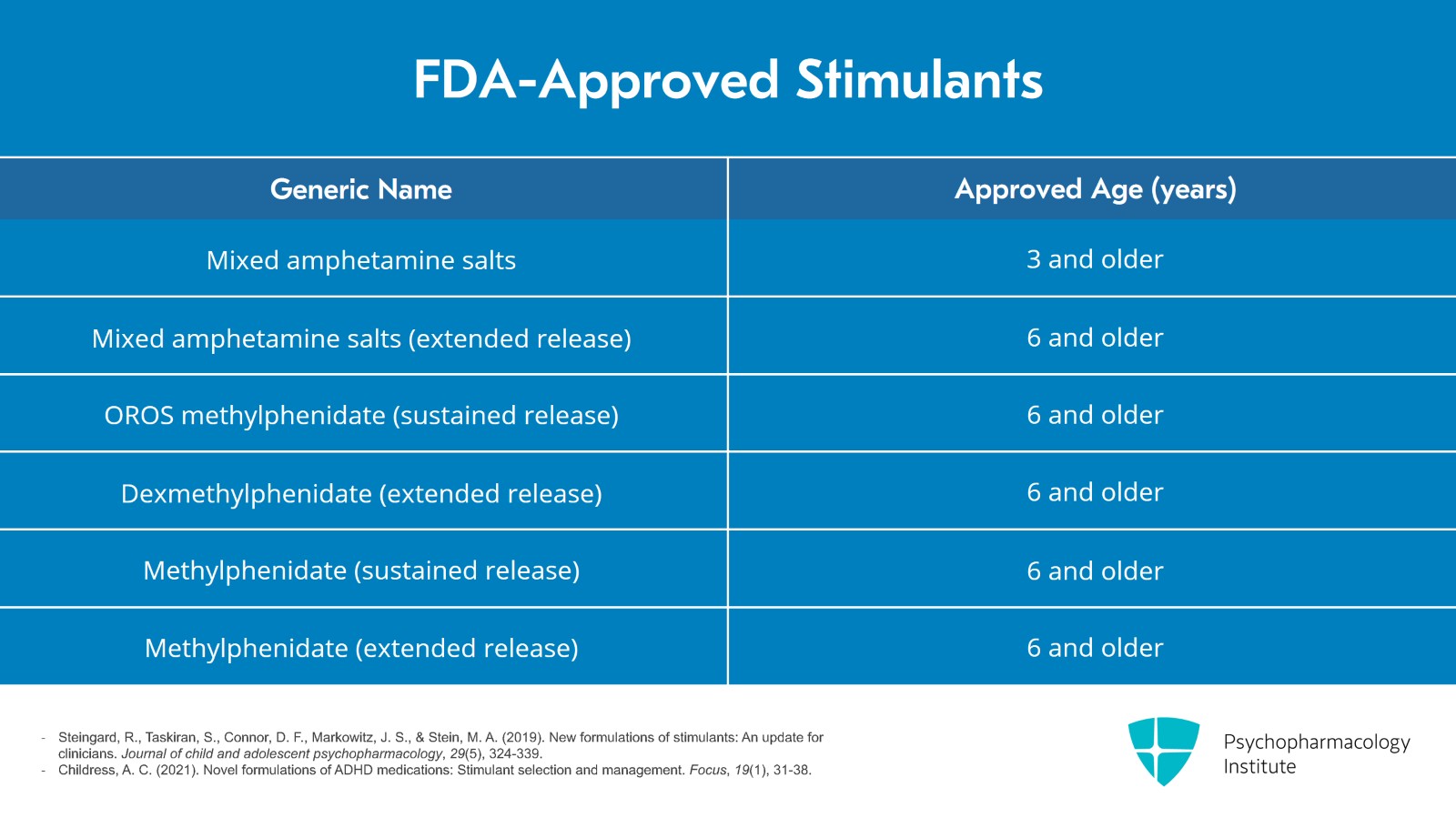
Now, I've provided you with a number of charts of both FDA-approved stimulants including some older agents such as mixed amphetamine salts, mixed amphetamine salts extended release. We've looked at methylphenidate products such as OROS methylphenidate sustained release, dexmethylphenidate extended release and a number of different extended-release methylphenidate preparations including methylphenidate sustained release and methylphenidate extended release.
References:
- Steingard, R., Taskiran, S., Connor, D. F., Markowitz, J. S., & Stein, M. A. (2019). New formulations of stimulants: An update for clinicians. Journal of child and adolescent psychopharmacology, 29(5), 324-339.
- Childress, A. C. (2021). Novel formulations of ADHD medications: Stimulant selection and management. Focus, 19(1), 31-38.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 20
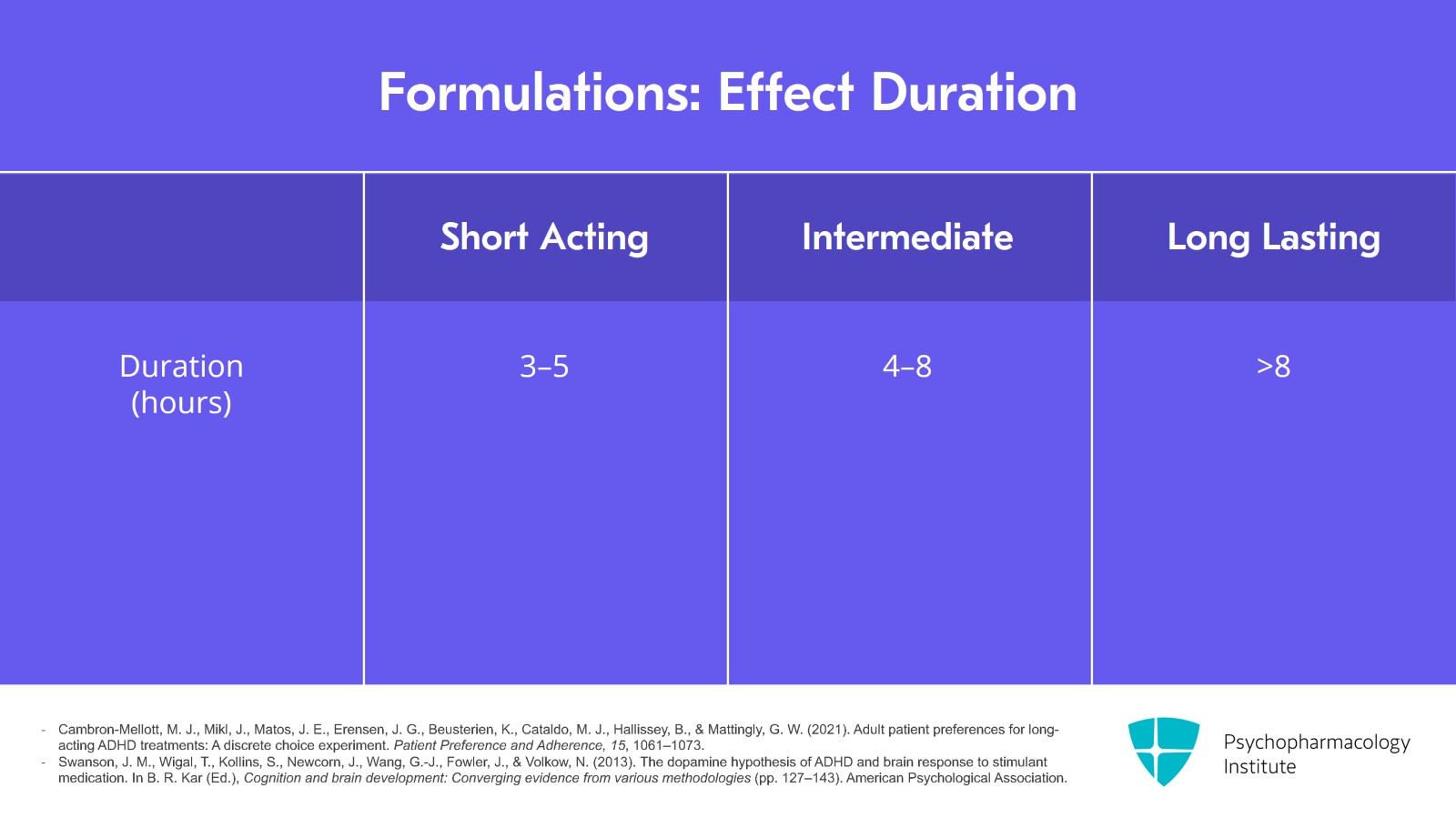
As I implied before, one of the big differences between stimulant preparations is not only the amphetamine-methylphenidate dichotomy but also formulations in terms of the time to onset and the duration of functioning or acting, that is there are short-acting drugs that last three to five hours or intermediate drugs which last from four to eight hours and finally a number of medications that last longer than eight hours. These are certainly preferrable for those individuals who need medication throughout the day and may forget multiple administrations.
References:
- Cambron-Mellott, M. J., Mikl, J., Matos, J. E., Erensen, J. G., Beusterien, K., Cataldo, M. J., Hallissey, B., & Mattingly, G. W. (2021). Adult patient preferences for long-acting ADHD treatments: A discrete choice experiment. Patient Preference and Adherence, 15, 1061–1073.
- Swanson, J. M., Wigal, T., Kollins, S., Newcorn, J., Wang, G.-J., Fowler, J., & Volkow, N. (2013). The dopamine hypothesis of ADHD and brain response to stimulant medication. In B. R. Kar (Ed.), Cognition and brain development: Converging evidence from various methodologies (pp. 127–143). American Psychological Association.
Slide 8 of 20
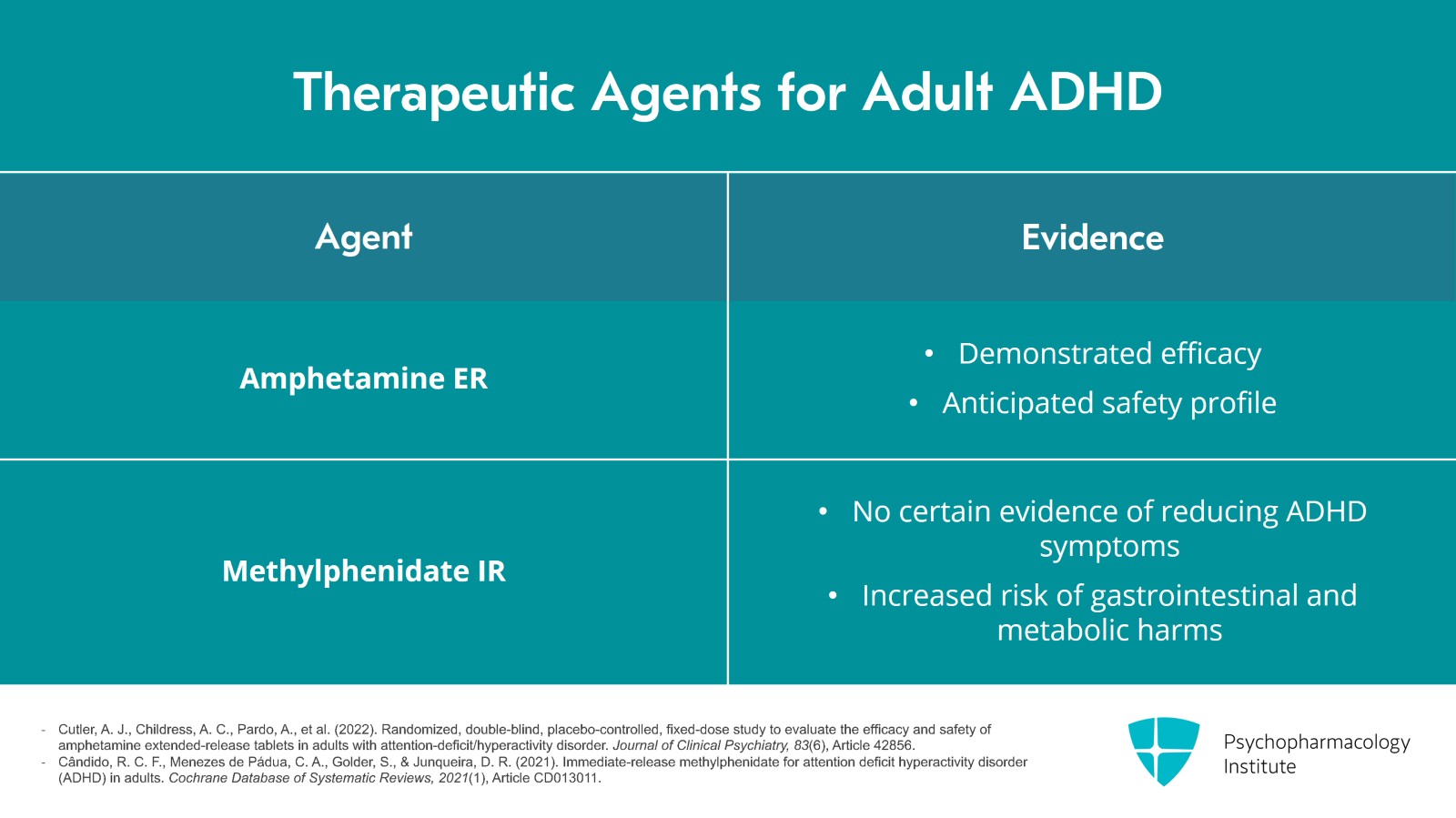
Amphetamine ER tablets demonstrated efficacy in the treatment of ADHD in adults with an anticipated safety profile. They found no certain evidence that IR methylphenidate compared with placebo or lithium can reduce the symptoms of ADHD in adults with low or very low-certainty evidence. Adults treated with IR methylphenidate are at increased risk of gastrointestinal and metabolic harms compared with placebo. Clinicians should consider whether it is appropriate to prescribe IR methylphenidate.
References:
- Cutler, A. J., Childress, A. C., Pardo, A., et al. (2022). Randomized, double-blind, placebo-controlled, fixed-dose study to evaluate the efficacy and safety of amphetamine extended-release tablets in adults with attention-deficit/hyperactivity disorder. Journal of Clinical Psychiatry, 83(6), Article 42856.
- Cândido, R. C. F., Menezes de Pádua, C. A., Golder, S., & Junqueira, D. R. (2021). Immediate-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database of Systematic Reviews, 2021(1), Article CD013011.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 20
Very low-certainty evidence that extended-release methylphenidate compared to placebo improved ADHD symptoms, that is small to moderate effects, measured on rating scales reported by participants, investigators and peers such as family members. Methylphenidate had no effect on days missed at work or serious adverse events, the effect on quality of life was small and it increased the risk of several adverse events. We rated the certainty of the evidence as very low for all outcomes due to high risk of bias, short trial durations and limitations to the generalizability of the results. The benefits and harms of extended-release methylphenidate therefore remains uncertain.
References:
- Boesen, K., Paludan-Müller, A. S., Gøtzsche, P. C., & Jørgensen, K. J. (2022). Extended-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database of Systematic Reviews, 2022(2), Article CD012857.
Slide 10 of 20
A case-control study found that the long-term exposure to ADHD medications was associated with an increased risk of cardiovascular diseases such as hypertension and arterial disease. Longer cumulative ADHD medication use was associated with increased risk of hypertension and arterial disease. Across the 14-year follow-up, each one-year increase of ADHD medication was associated with a 4% increased risk of cardiovascular disease with a larger increased risk in the first three years of cumulative use and stable risk over the remaining follow-up. Similar patterns were observed in children and youth, that is age less than 25 years, and adults, age greater than 25 years.
References:
- Zhang, L., Li, L., Andell, P., et al. (2024). Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry, 81(2), 178–187.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 20
These findings highlight the importance of careful weighing of potential benefits and risks when making treatment decisions about long-term ADHD medication use. Clinicians should regularly and consistently monitor cardiovascular signs and symptoms throughout the course of treatment.
References:
- Zhang, L., Li, L., Andell, P., et al. (2024). Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry, 81(2), 178–187.
Slide 12 of 20
However, other side effects are more common such as irritability, decreased appetite plus or minus weight loss. The present status of being a schedule 2 drug by the DEA indicates a higher risk of misuse or addiction from stimulant medications. The discontinuation rate among adults due to adverse events is about 10%.
References:
- Wilens, T. E., Martelon, M., Joshi, G., Bateman, C., Fried, R., Petty, C., & Biederman, J. (2011). Does ADHD predict substance-use disorders? A 10-year follow-up study of young adults with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry, 50(6), 543-553.
- Nanda, A., Janga, L. S. N., Sambe, H. G., Yasir, M., Man, R. K., Gogikar, A., & Mohammed, L. (2023). Adverse effects of stimulant interventions for attention deficit hyperactivity disorder (ADHD): A comprehensive systematic review. Cureus, 15(9), e45995.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 20
As I mentioned previously, we are likely to consider longer-acting drugs over shorter-acting stimulant medications. These longer-acting drugs result in better functioning during the course of the day and probably have lower abuse potential.
References:
- Habel, L. A., Cooper, W. O., Sox, C. M., Chan, K. A., Fireman, B. H., Arbogast, P. G., … & Andrade, S. E. (2011). ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. Jama, 306(24), 2673-2683.
- Zhang, L., Li, L., Andell, P., et al. (2024). Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry, 81(2), 178–187.
Slide 14 of 20
In considering which preparation to prescribe, the clinician or prescriber should consider patient preference and should start low and progressively increase the medication until there is little or no room for improvement. The clinician should also balance side effects versus clinical effectiveness.
References:
- Habel, L. A., Cooper, W. O., Sox, C. M., Chan, K. A., Fireman, B. H., Arbogast, P. G., … & Andrade, S. E. (2011). ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. Jama, 306(24), 2673-2683.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 20
During the course of treatment, the prescriber should monitor side effects through such things as vital signs, blood pressure, heart rate or weight and should examine neurovegetative symptoms such as sleep, appetite or ask about other somatic ills such as headache or GI distress.
References:
- Habel, L. A., Cooper, W. O., Sox, C. M., Chan, K. A., Fireman, B. H., Arbogast, P. G., … & Andrade, S. E. (2011). ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. Jama, 306(24), 2673-2683.
- Zhang, L., Li, L., Andell, P., et al. (2024). Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry, 81(2), 178–187.
Slide 16 of 20
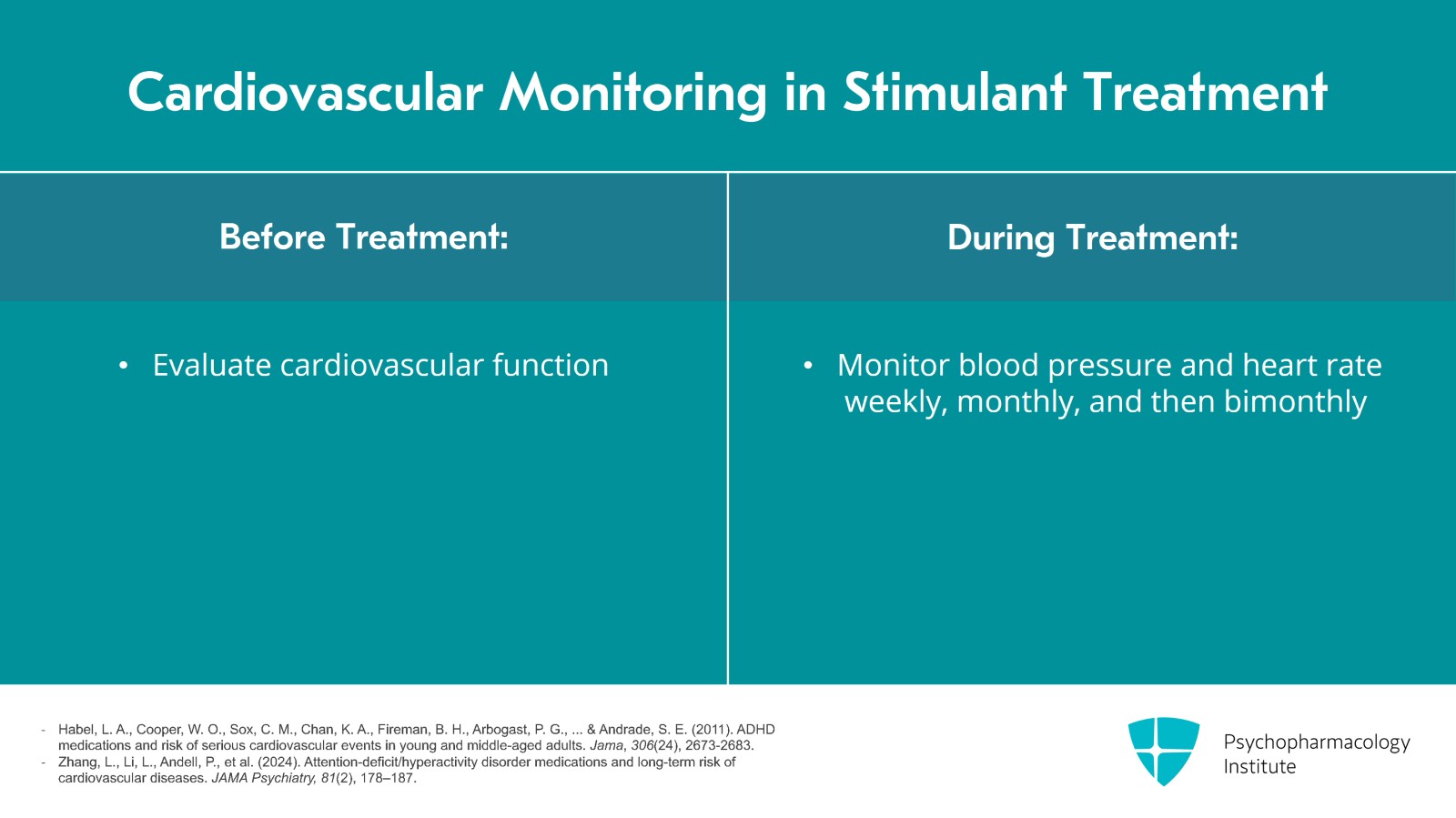
In terms of cardiovascular evaluation and monitoring, we mentioned before that it is important prior to treatment to evaluate cardiovascular function through eliciting of symptoms, a positive cardiovascular history, blood pressure and heart rate. During the course of stimulant treatment, one should monitor blood pressure and heart rate initially weekly, monthly, then bimonthly during maintenance treatment.
References:
- Habel, L. A., Cooper, W. O., Sox, C. M., Chan, K. A., Fireman, B. H., Arbogast, P. G., … & Andrade, S. E. (2011). ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. Jama, 306(24), 2673-2683.
- Zhang, L., Li, L., Andell, P., et al. (2024). Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry, 81(2), 178–187.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 20
Monitoring treatment can be done through the use or rating scales. Some of the rating scales that I mentioned previously or some of the subscales can be administered at intervals to monitor the effectiveness of drug. The lack of effectiveness suggests changing the preparation or specifically changing from amphetamine to methylphenidate or vice versa prior to augmentation to non-stimulant medications.
References:
- Habel, L. A., Cooper, W. O., Sox, C. M., Chan, K. A., Fireman, B. H., Arbogast, P. G., … & Andrade, S. E. (2011). ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. Jama, 306(24), 2673-2683.
- Zhang, L., Li, L., Andell, P., et al. (2024). Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry, 81(2), 178–187.
Slide 18 of 20
The key points to this section are that stimulants including methylphenidate and amphetamine come in several formulations – short acting, intermediate acting and long acting. Common side effects include dry mouth, insomnia, irritability, decreased appetite, weight loss and headaches.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 20
Prescribers should screen for cardiovascular risk factors before beginning stimulants and monitor blood pressure and heart rate during treatment.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.