Slides and Transcript
Slide 1 of 19
Hi. This is video number six which is pharmacologic strategies for managing agitation, and we'll go over some general recommendations and our destination treatment goals that we have for intervening with agitated patients.
Slide 2 of 19
So, number one, recognize that when we give medications for somebody in agitation, especially when we are using parenteral medications, those are not chemical restraints. And this is far too often a thought that a lot of our colleagues and especially physicians and providers working in emergency settings often they think that anytime we give an injectable psychiatric medication that that's chemical restraints.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology Workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 19
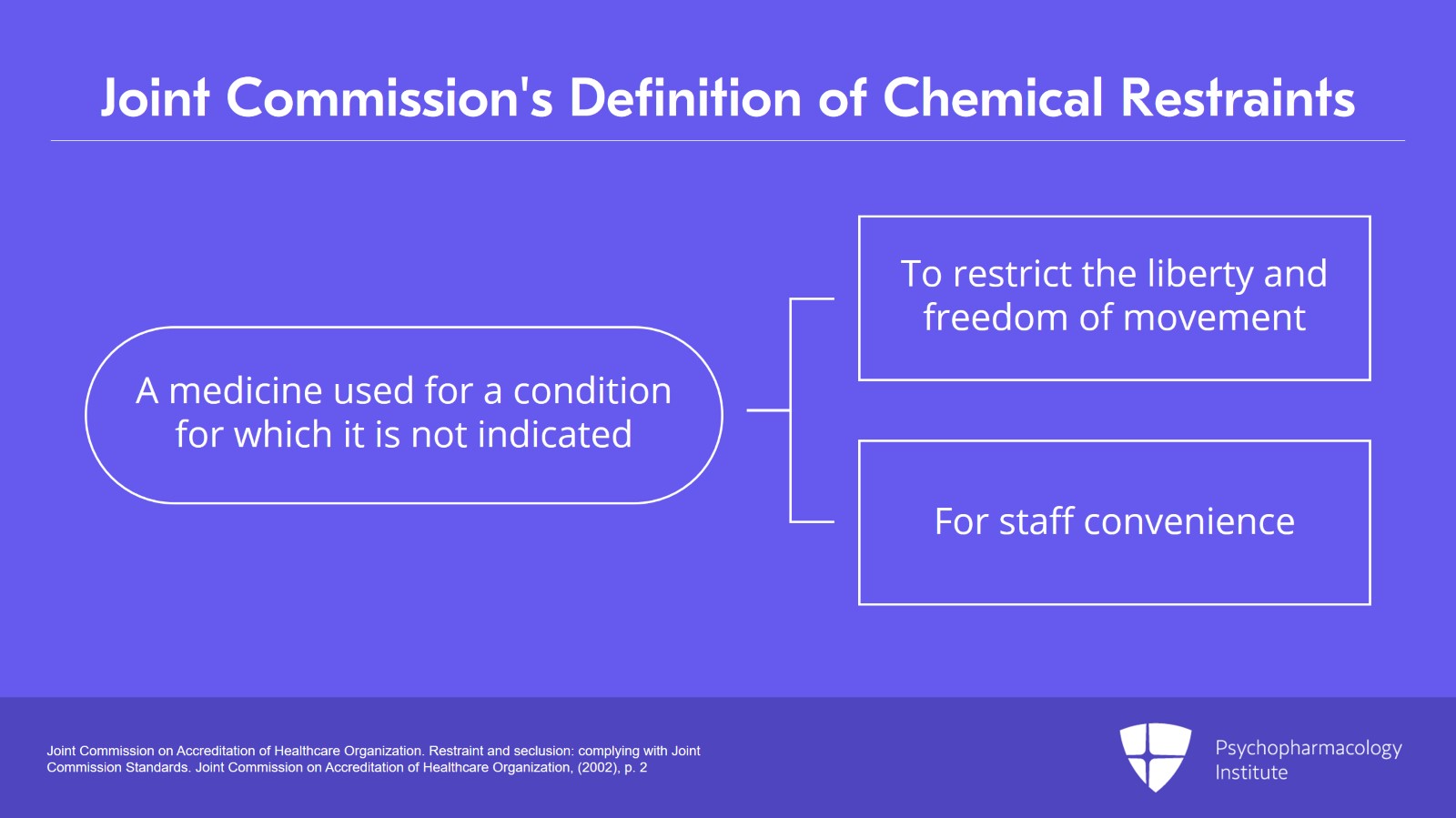
Well, understand that The Joint Commission's definition of chemical restraints is, paraphrased here, a medication used for a condition it is not indicated for solely to restrict the liberty and freedom of movement of an individual or for staff convenience. That doesn't sound very good, does it? Because the key phrase there is for condition it's not indicated for.
References:
- Joint Commission on Accreditation of Healthcare Organization. Restraint and seclusion: complying with Joint Commission Standards. Joint Commission on Accreditation of Healthcare Organization, (2002), p. 2
Slide 4 of 19
When you're actually treating agitation, that's not a chemical restraint. We should throw that term out because it's a little bit derogatory. And when we think about the stigma of mental illness, how many conditions do we say, let's give that person chemicals too? We don't chemically treat a diabetic patient. We don't chemically treat a person with asthma. We give them medications. Well, we're giving medications to people with agitation as well and that's the way we should look at it. We're treating a condition of agitation. We're not chemically restraining anybody, and we need to get that out of our lexicon and not use it anymore.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 19
We know that the medications that we're using in agitation that there's a number of them that are approved by the FDA specifically for treatment of agitation. And the other ones that we use may not be specifically FDA approved but there are community standards that they've been used for these conditions for years and years and years. So that automatically eliminates the definition that it's a medication used outside of its indication.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Slide 6 of 19
At that same time when we're treating agitation, we should go with our non-pharmacologic approaches first like verbal de-escalation, calming techniques, getting people in low-stimulation areas. And then we use medication.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 19
And another key point, is that patients should be involved in the process of determining what medication they are when they're agitated.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Slide 8 of 19
Remember that the average agitated person is not incoherent. They're just agitated.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 19
So, they can actually answer questions, and you can ask them if they might be willing to take oral meds instead of being forced to take a shot, and that can actually be very, very useful A lot of them can tell you what medication is helpful for them in this stage because it's usually a very distressing situation for them, and they'd prefer not to be agitated as well. It's always worth, if possible, to ask somebody, hey, is there a medication that helps you when things are like they are right now? And you might be surprised the way people respond.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Slide 10 of 19
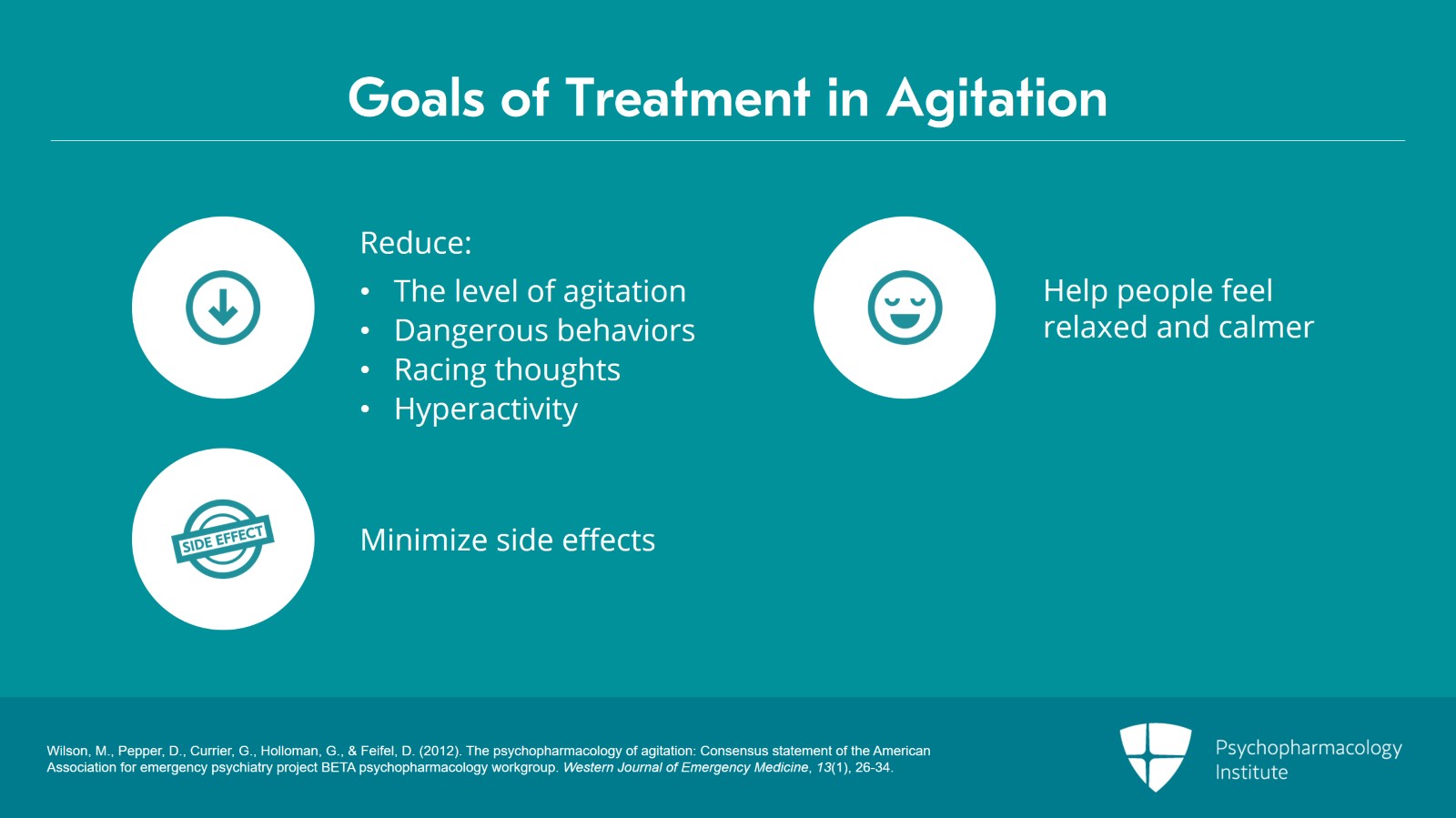
So, when we're thinking of agitation medications in general, what are our goals? What are we trying to do when we treat agitation? Well, number one, and this is almost obvious, we want to reduce that level of agitation; reduce those dangerous behaviors, the distress, the anguish that the agitation is causing; reduce the racing thoughts, the hyperactivity; help people feel relaxed, calmer, better control. We want to do that in such a way, though, where there are as few side effects as possible, just like we do with any medication.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 19
And, let's remember that our goal is for people to calm down, not be unconscious. That's a big difference. There's a lot of folks that think when there's a person with acute agitation, our goal is to see how heavily we can sedate them, but that's really not very useful. Our goal is to calm people, not to knock them out; calm them to tranquility, not to unconsciousness. Do it in such a way that, hopefully, you don't have to use physical restraints but instead create a therapeutic alliance with your patient. And by doing so, that will hopefully help people from getting into those emergency conditions again.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Slide 12 of 19
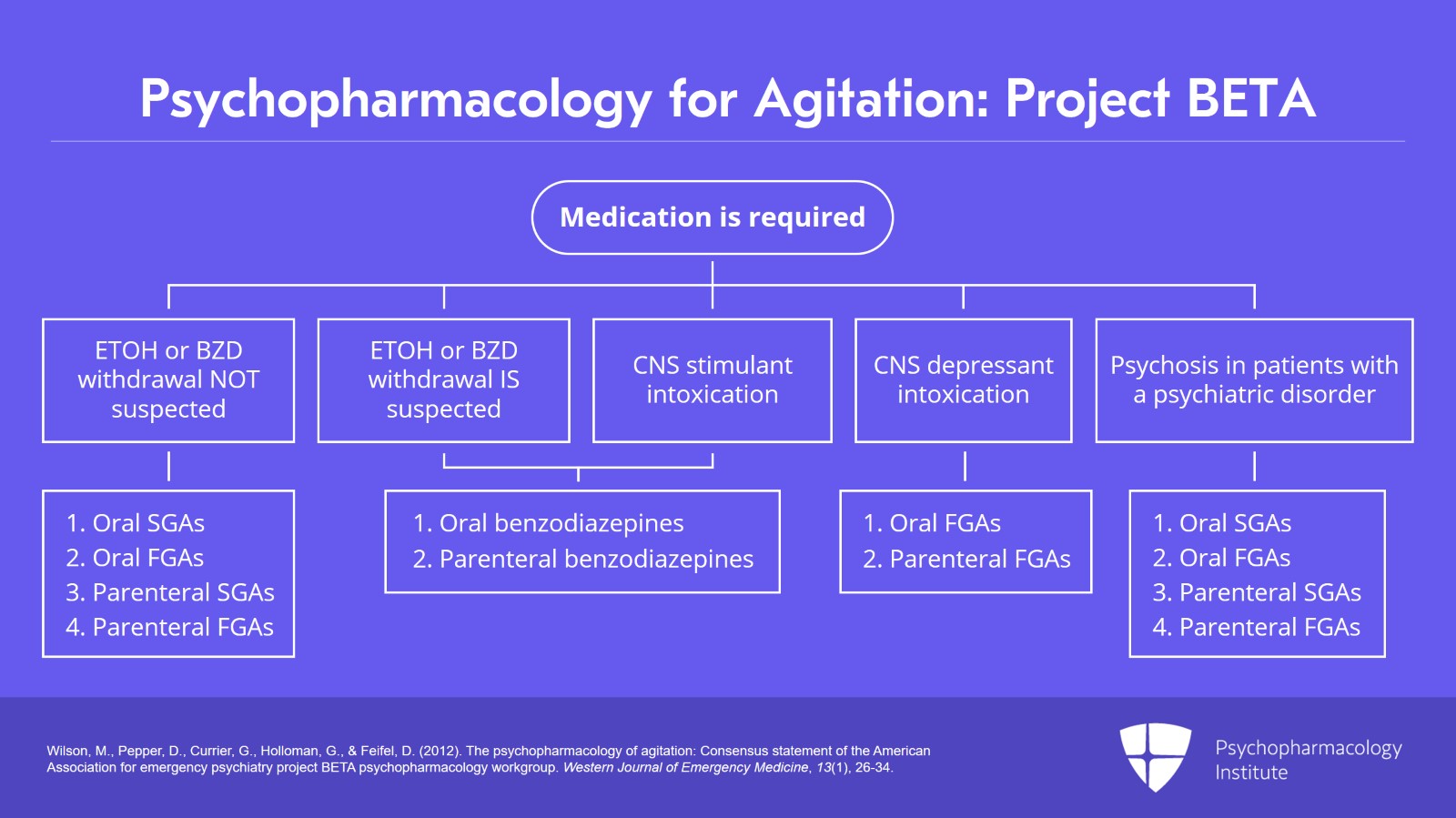
What you're seeing now is an algorithm flowchart that was created as part of the Project BETA, Best Practices in Evaluation and Treatment of Agitation, medication consideration for the pharmacologic treatment of agitation. This is about 10 years old now, but it's surprisingly still contemporary and up to date.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 19
And basically, we really want to offer oral medications for people in all these conditions before resorting to parenteral meds. And some folks might say yes, but the parenteral meds work faster. Well, not in every situation. Actually, p.o. lorazepam and IM lorazepam have just about the same time of onset.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Slide 14 of 19
But even in those situations, like many of the antipsychotic medications where there is a faster onset for intramuscular administration than there is for oral, sometimes we're only talking about minutes of difference. And the time that it takes to get all the things going, like get the team together, draw up the medications into the syringe, all the kind of things that are involved with administering an intramuscular med, that takes a lot of time.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 19
And if you get somebody to willingly take an oral med in a matter of minutes, they could already be well on their way to being in control of their agitation, while if you're thinking that your only alternative was IM, you'd still be working on drawing that up into the syringe. And as I've said before, nobody ever got a needlestick from offering oral medications.
References:
- Wilson, M., Pepper, D., Currier, G., Holloman, G., & Feifel, D. (2012). The psychopharmacology of agitation: Consensus statement of the American Association for emergency psychiatry project BETA psychopharmacology workgroup. Western Journal of Emergency Medicine, 13(1), 26-34.
Slide 16 of 19
So, our key points when we're thinking about using medications to treat agitation is medications are not chemical restraints, but they're appropriate agents that are chosen to treat the disease state of acute agitation. In many cases, these are FDA approved treatments for agitation, or these are treatments for agitation that meet community standards.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 19
Medication goal in agitation is calmness, calming people to tranquility, not to see how heavily you can sedate them. And if you're working in an emergency setting, you have a limited amount of space-time opportunity to treat the individuals you're seeing. You don't have the luxury of knocking somebody unconscious for 16 hours because that's denying the opportunity for other people to get help, and you're not helping the person who is unconscious anyway. So, treating with the goal of calmness is going to be far more ethical, humane, and beneficial for our patients, and it's also going to benefit our overall emergency setting and system as a whole.
Slide 18 of 19
Finally, remember that offering medication is not a separate part of de-escalation but it's part of de-escalation and you're doing it as you're using de-escalation techniques. When you can get people to voluntarily accept medication, that's usually far, far preferred. That's a win. Everybody's getting along. There’s far less risk of violence or aggression, and you're going to have a much better opportunity to get people to that next level of care than you would if you just defaulted to putting people into physical restraints and forcibly medicating them.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.