Slides and Transcript
Slide 1 of 15
Next, we’re going to spend some time talking about both pharmacologic and nonpharmacologic treatment approaches.
Slide 2 of 15
And when trying to understand how to best address a behavioral and psychological symptom in dementia, it’s really important to understand what the underlying etiology is and that will really help you direct treatment. So a urinary tract infection, pain, issues with the caregiver, or psychosis should all be addressed very differently.
References:
- Schneider, L. S., Pollock, V. E., & Lyness, S. A. (1990). A Metaanalysis of controlled trials of neuroleptic treatment in dementia. Journal of the American Geriatrics Society, 38(5), 553-563
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
However, in real-world treatment, patients with behavioral and psychological symptoms of dementia often receive antipsychotics.
Now, while antipsychotics do have the best evidence for treating these symptoms, their effects, meaning the magnitude of their treatment size, are moderate at best and they have an effect size of 0.13 to 0.16.
And any benefits with an antipsychotic must be balanced against the risk of adverse events including mortality as outlined by the US FDA box warning.
References:
- Schneider, L. S., Pollock, V. E., & Lyness, S. A. (1990). A Metaanalysis of controlled trials of neuroleptic treatment in dementia. Journal of the American Geriatrics Society, 38(5), 553-563
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 4 of 15
So many of you are probably aware of the US FDA black box warning related to use of the antipsychotics for dementia-related behaviors.
And that’s based off of numerous randomized clinical trials that showed that elderly patients with dementia-related psychosis who are treated with antipsychotic drugs are at an increased risk, and generally we say 1.6 to 1.7 times increased risk of death, as compared to placebo.
References:
- Schneider, L. S., Pollock, V. E., & Lyness, S. A. (1990). A Metaanalysis of controlled trials of neuroleptic treatment in dementia. Journal of the American Geriatrics Society, 38(5), 553-563.
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
And folks often ask, what are the causes of death related to antipsychotic treatment?
And generally, that tends to be a cardiovascular event like a ventricular arrythmia or prolonged QTc. It can be a cerebrovascular event like a stroke or a pneumonia like an aspiration event.
References:
- Schneider, L. S., Pollock, V. E., & Lyness, S. A. (1990). A Metaanalysis of controlled trials of neuroleptic treatment in dementia. Journal of the American Geriatrics Society, 38(5), 553-563.
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Slide 6 of 15
It’s important to remember though that antipsychotics have many other side effects other than just the increased mortality risk which can also cause distress for patients.
And those can include things like extrapyramidal side effects, falls, sedation as well as worsening cognition.
References:
- Schneider, L. S., Pollock, V. E., & Lyness, S. A. (1990). A Metaanalysis of controlled trials of neuroleptic treatment in dementia. Journal of the American Geriatrics Society, 38(5), 553-563.
- Gerlach, L. B., & Kales, H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315-327.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
So I’ll highlight some findings from a few studies here.
The first study was done by Donovan Maust which took a look at patients with dementia who received antipsychotic medications as well as valproic acid and looked at the number needed to harm for each of these medications. So they looked at how many patients had to be treated to cause one episode of death or what they called harm.
References:
- Maust, D. T., Kim, H. M., Seyfried, L. S., Chiang, C., Kavanagh, J., Schneider, L. S., & Kales, H. C. (2015). Antipsychotics, other psychotropics, and the risk of death in patients with dementia. JAMA Psychiatry, 72(5), 438.
Slide 8 of 15
And the numbers are far too small for these medications. And for haloperidol, it can take only eight patients treated with this medication to be associated with one death. And even for valproic acid, there is still an increased risk.
References:
- Maust, D. T., Kim, H. M., Seyfried, L. S., Chiang, C., Kavanagh, J., Schneider, L. S., & Kales, H. C. (2015). Antipsychotics, other psychotropics, and the risk of death in patients with dementia. JAMA Psychiatry, 72(5), 438.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
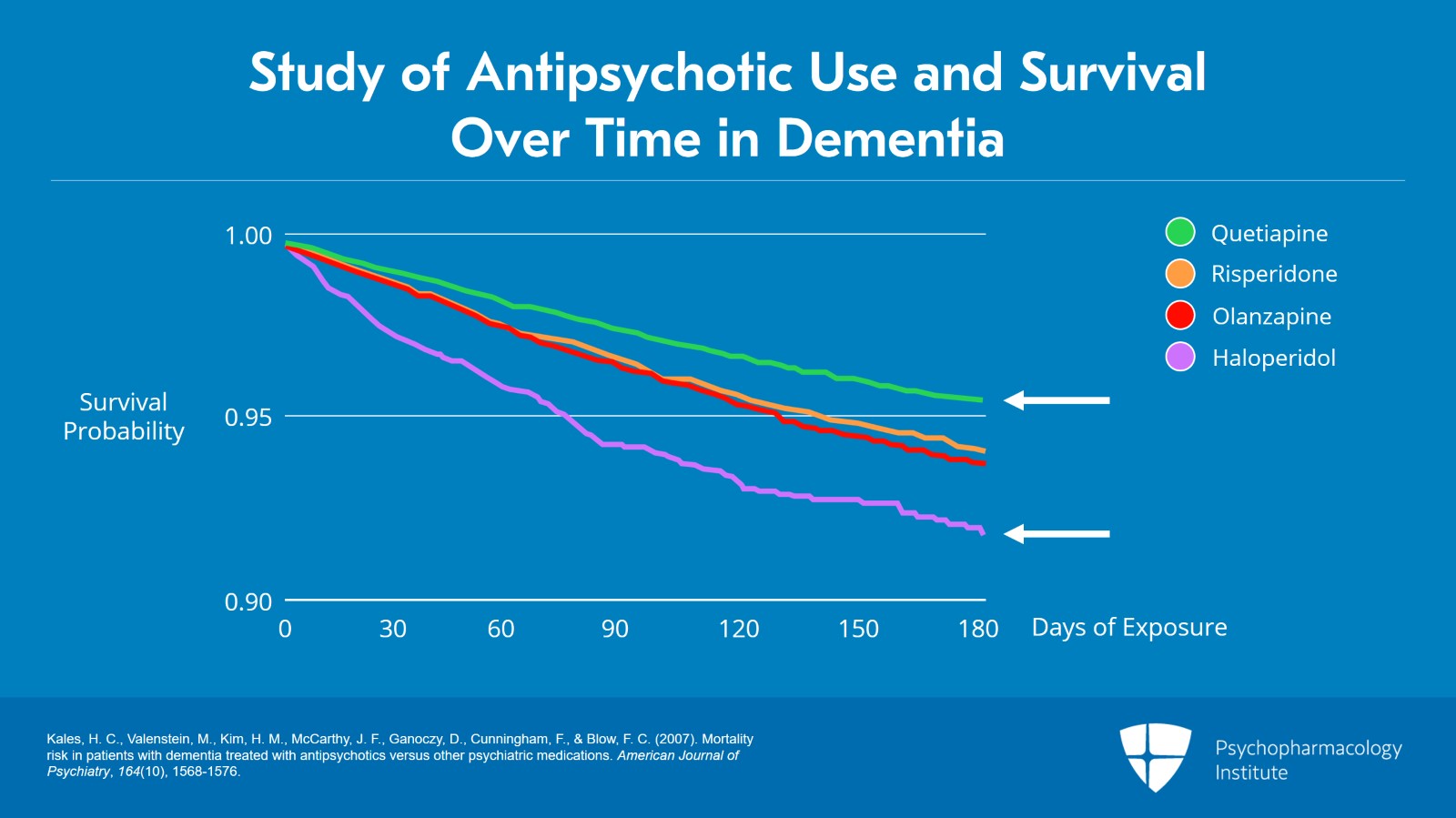
The figure here shows a graph from a study from Helen Kales looking at veterans with dementia who were prescribed different antipsychotic medications and survival over time.
And as we can see, patients with dementia who are prescribed these medications have decreased survival curves, meaning that each of these medications is associated with mortality. Haloperidol is the purple line here which has a steeper slope and associated with greater mortality. Quetiapine is the green line on top, a little bit less but still an increased mortality risk.
References:
- Kales, H. C., Valenstein, M., Kim, H. M., McCarthy, J. F., Ganoczy, D., Cunningham, F., & Blow, F. C. (2007). Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. American Journal of Psychiatry, 164(10), 1568-1576.
Slide 10 of 15
So we know that these antipsychotic medications come with significant risk.
So it’s important to think about what are other evidence-based approaches to detecting and managing these behaviors. And it’s really important to think about what are the possible etiologies that are contributing, to include caregivers in the process.
References:
- Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ, 350(27), h369-h369.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
As well as to think about how to integrate pharmacologic and nonpharmacologic treatment options as well as the built-in flexibility to use these types of treatments in a variety of care settings where patients are.
References:
- Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ, 350(27), h369-h369.
Slide 12 of 15
And really, the goal is to try to avoid knee jerk prescribing of medications without an assessment of underlying causes.
And in the next section, I’ll kind of walk through how we think about nonpharmacologic treatment options for behavioral disturbances in dementia.
References:
- Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ, 350(27), h369-h369.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
All right. So our key points.
So similar to the treatment of delirium, knowing the underlying causes of behavioral and psychological symptoms of dementia will really help best direct the appropriate treatment. So again, infections, issues with caregivers, trouble with the environment and psychosis should all be approached very differently.
13
Slide 14 of 15
However, in real-world practice, persons with dementia are often prescribed psychotropic medications like antipsychotics despite evidence for a modest treatment effect.
While antipsychotics do have the best evidence for treatment of behavioral and psychological symptoms of dementia, they are associated with significant risk including increased mortality, falls, confusion, sedation as well as motor side effects.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.