Slides and Transcript
Slide 1 of 13
In the next section, we’re going to talk about some novel medication approaches that have been used in borderline personality disorder.
The reason to do this really is to talk about some future directions that research is taking as they may have important value for understanding mechanisms leading to borderline personality disorder but none of these medications have sufficient evidence to really apply them clinically at this point. And there’s a whole host of medications that have been tried and we’ll go through some of them in this section.
Slide 2 of 13
Perhaps one of the most interesting is omega-3 fatty acids such as eicosapentaenoic acid and docosahexaenoic acid have been used in borderline patients.
There has been some evidence they can decrease depression, suicidality, or affective instability. And recently, there has been a meta-analysis that summarized across these studies using omega-3 fatty acids and they did suggest that they can be helpful for the impulsive dyscontrol and the affective dysregulation in borderline patients. So they do have some promise when you’re treating borderline patients.
References:
- Bozzatello, P., Rocca, P., & Bellino, S. (2018). Combination of omega-3 fatty acids and Valproic acid in treatment of borderline personality disorder: A follow-up study. Clinical Drug Investigation, 38(4), 367-372.
- Hallahan, B., Hibbeln, J. R., Davis, J. M., & Garland, M. R. (2007). Omega-3 fatty acid supplementation in patients with recurrent self-harm. British Journal of Psychiatry, 190(2), 118-122.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 13
Methylphenidate has been used in borderline patients with comorbid ADHD and they do suggest that methylphenidate can help with the ADHD symptoms with motor impulsivity, anger, and depression.
References:
- Gvirts, H. Z., Lewis, Y. D., Dvora, S., Feffer, K., Nitzan, U., Carmel, Z., Levkovitz, Y., & Maoz, H. (2018). The effect of methylphenidate on decision making in patients with borderline personality disorder and attention-deficit/hyperactivity disorder. International Clinical Psychopharmacology, 33(4), 233-237.
- Golubchik, P., Sever, J., Zalsman, G., & Weizman, A. (2008). Methylphenidate in the treatment of female adolescents with cooccurrence of attention deficit/hyperactivity disorder and borderline personality disorder: A preliminary open-label trial. International Clinical Psychopharmacology, 23(4), 228-231.
Slide 4 of 13
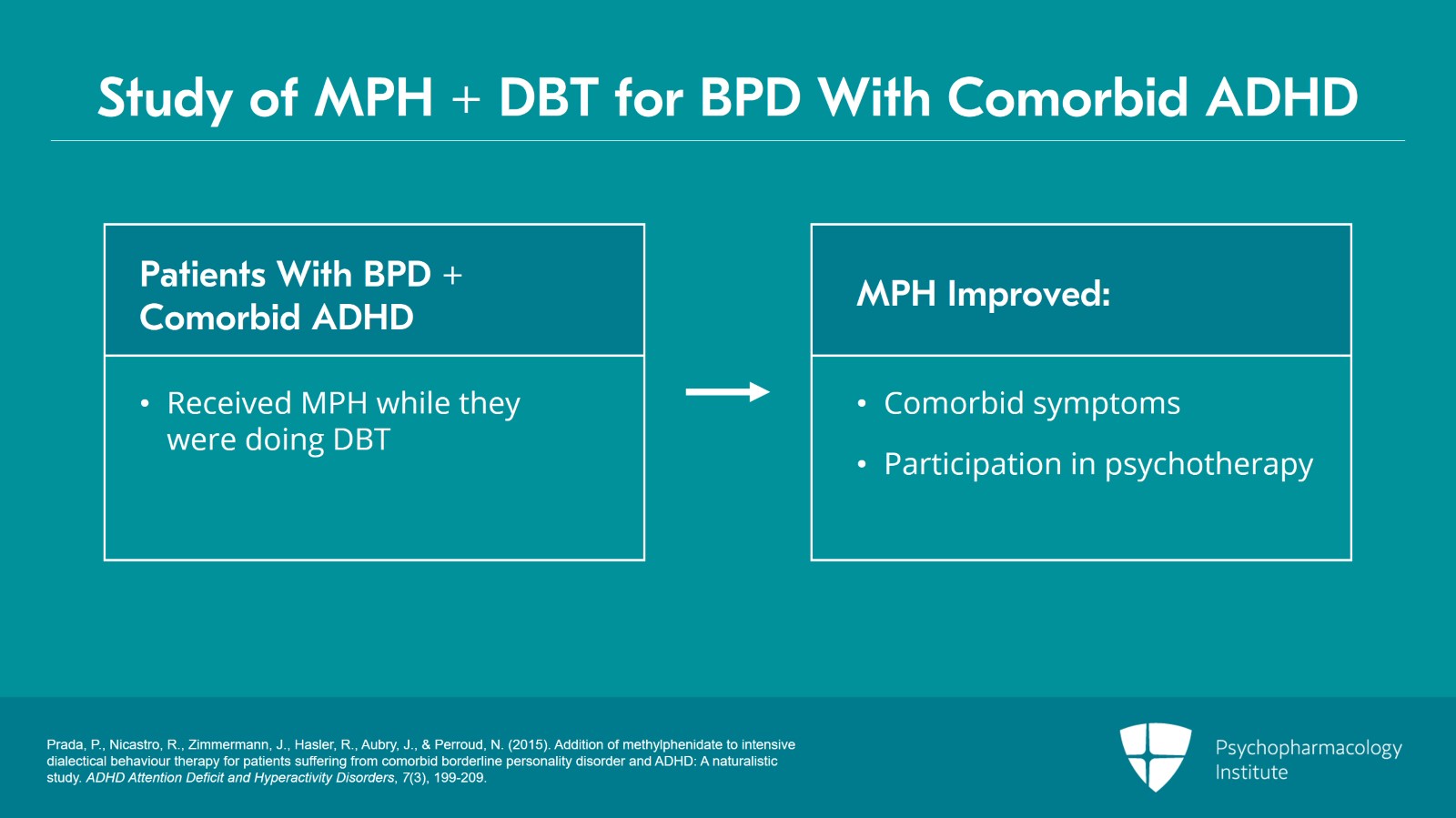
But one of the most interesting studies was by Prada et al., for borderline patients with comorbid ADHD where they used methylphenidate while they were doing dialectic behavior therapy. And the important lesson from that was that the use of methylphenidate helped the comorbid symptoms and improved the patient’s participation in the psychotherapy. And that often can be a useful role of using medications so that the patient can take better benefit of their therapy, their schooling, their work.
References:
- Prada, P., Nicastro, R., Zimmermann, J., Hasler, R., Aubry, J., & Perroud, N. (2015). Addition of methylphenidate to intensive dialectical behaviour therapy for patients suffering from comorbid borderline personality disorder and ADHD: A naturalistic study. ADHD Attention Deficit and Hyperactivity Disorders, 7(3), 199-209.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 13
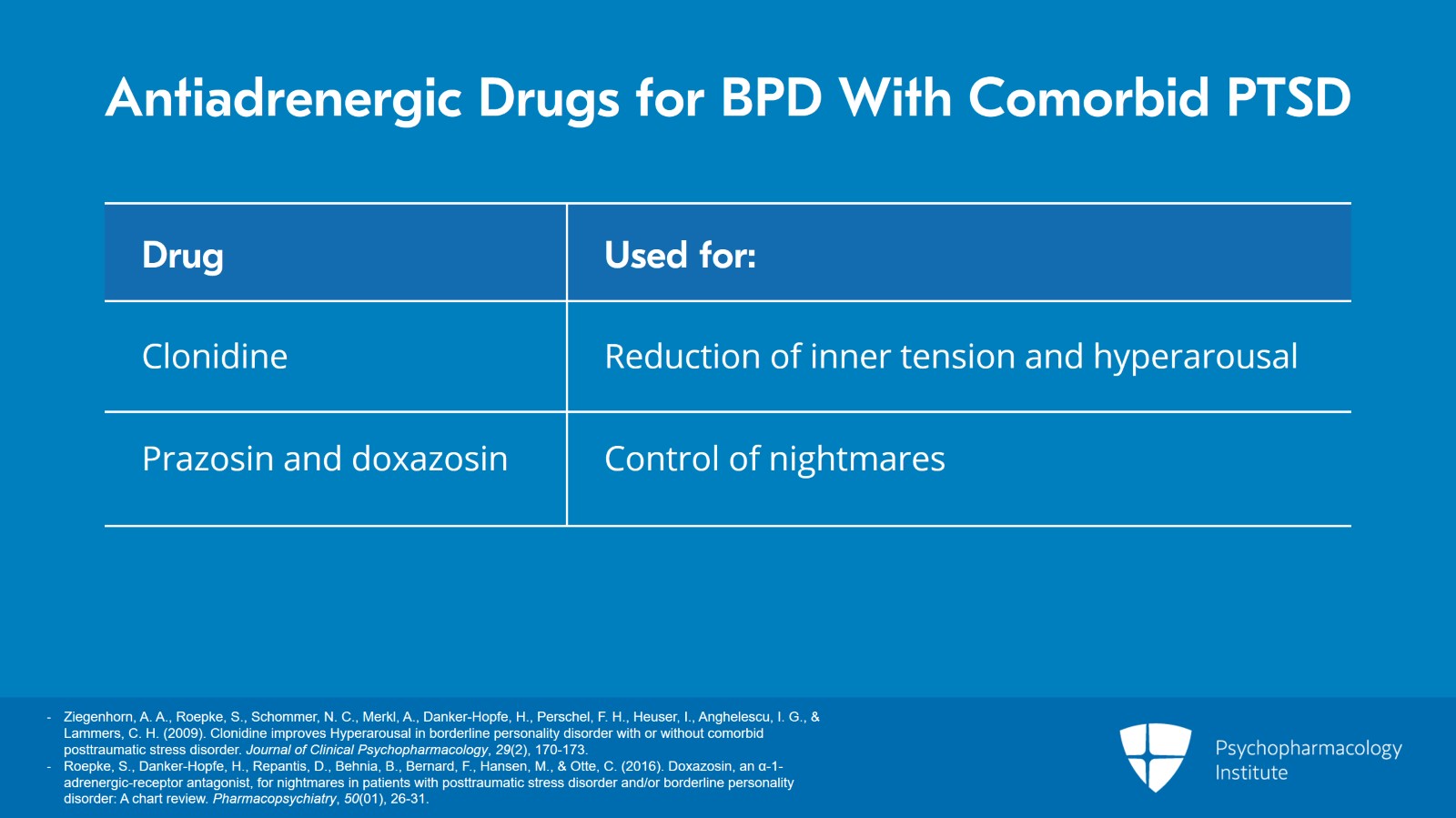
Clonidine has been used in borderline patients with comorbid posttraumatic stress disorder to try to reduce inner tension and hyperarousal.
Prazosin and doxazosin have been used to try to control nightmares that you might find in a borderline patient with comorbid posttraumatic stress disorder.
References:
- Ziegenhorn, A. A., Roepke, S., Schommer, N. C., Merkl, A., Danker-Hopfe, H., Perschel, F. H., Heuser, I., Anghelescu, I. G., & Lammers, C. H. (2009). Clonidine improves Hyperarousal in borderline personality disorder with or without comorbid posttraumatic stress disorder. Journal of Clinical Psychopharmacology, 29(2), 170-173.
- Roepke, S., Danker-Hopfe, H., Repantis, D., Behnia, B., Bernard, F., Hansen, M., & Otte, C. (2016). Doxazosin, an α-1-adrenergic-receptor antagonist, for nightmares in patients with posttraumatic stress disorder and/or borderline personality disorder: A chart review. Pharmacopsychiatry, 50(01), 26-31.
Slide 6 of 13
And memantine has been used for borderline symptoms in an early randomized controlled trial. This is important because it’s suggesting that there might be glutamate mechanisms that are involved in borderline symptoms. So, this is trying to explore other possible pathophysiologic mechanisms leading to borderline personality disorder.
References:
- Kulkarni, J., Thomas, N., Hudaib, A., Gavrilidis, E., Grigg, J., Tan, R., Cheng, J., Arnold, A., & Gurvich, C. (2018). Effect of the glutamate NMDA receptor antagonist Memantine as adjunctive treatment in borderline personality disorder: An exploratory, randomised, double-blind, placebo-controlled trial. CNS Drugs, 32(2), 179-187.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 13
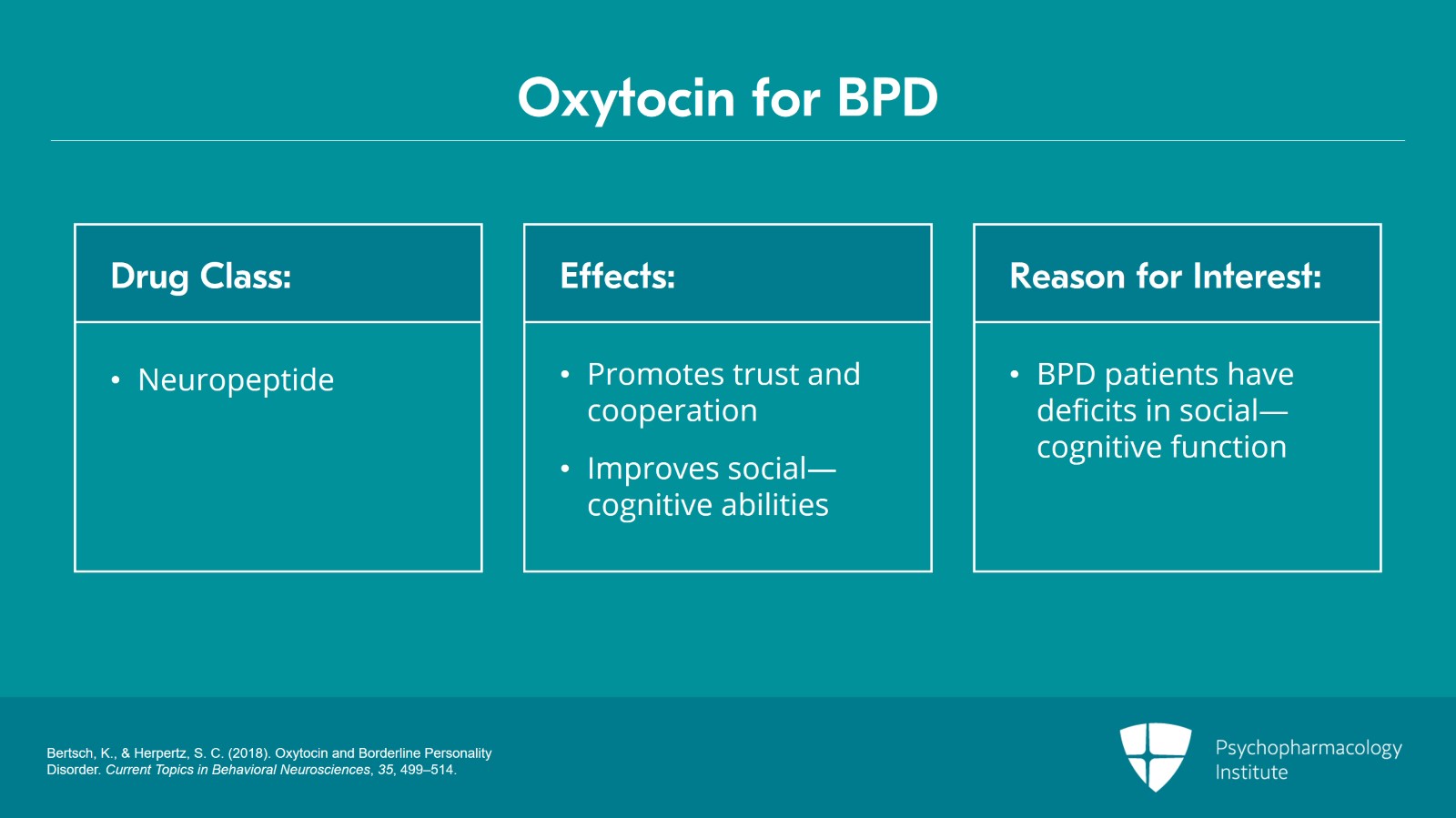
Oxytocin has been studied for borderline personality disorder and that’s a neuropeptide that is excreted from the posterior pituitary. And of course, it’s been found as a compound that can promote trust and cooperation and improved social cognitive abilities. And of course, it’s of interest in patients with borderline personality disorder because we know that they have the deficits in their social cognitive function. They often have deficits in mentalizing and they have a bias towards negative social stimuli. So, it’s certainly a compound of interest.
References:
- Bertsch, K., & Herpertz, S. C. (2018). Oxytocin and Borderline Personality Disorder. Current Topics in Behavioral Neurosciences, 35, 499–514.
Slide 8 of 13
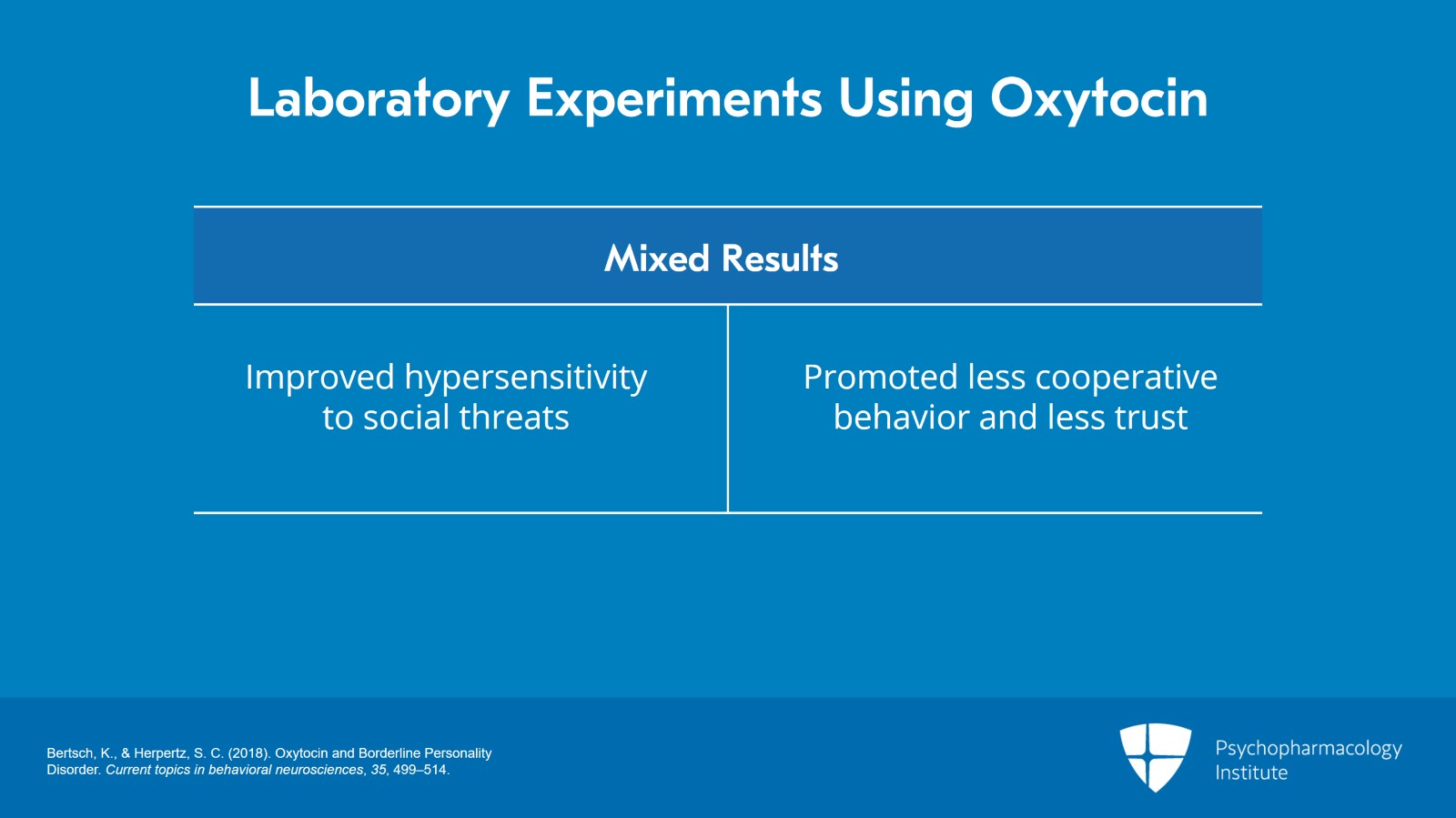
At this point in time, there are no satisfactory clinical trials but there are some laboratory experiments using oxytocin. And it’s interesting that these laboratory experiments provide very mixed results. In some of the studies, they show improved hypersensitivity to social threats so they’re reading them more accurately. But in other situations, oxytocin promoted less cooperative behavior and less trust.
References:
- Bertsch, K., & Herpertz, S. C. (2018). Oxytocin and Borderline Personality Disorder. Current topics in behavioral neurosciences, 35, 499–514.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 13
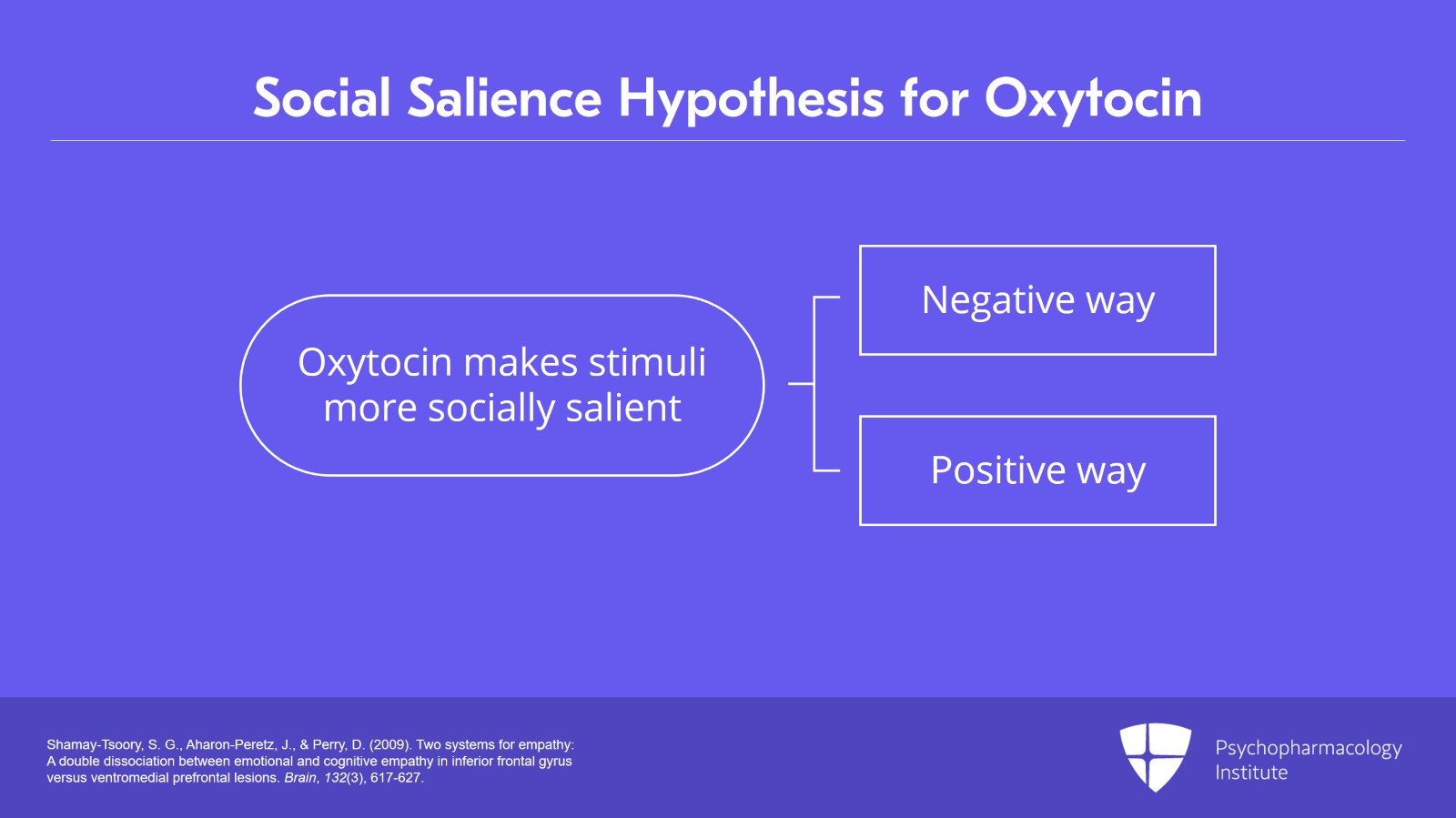
These mixed findings are hard to understand but one possibility is the social salience hypothesis that is that oxytocin makes stimuli more socially salient but obviously they can be salient in a negative or positive way and that may be what happens to borderline patients.
References:
- Shamay-Tsoory, S. G., Aharon-Peretz, J., & Perry, D. (2009). Two systems for empathy: A double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain, 132(3), 617-627.
Slide 10 of 13
But suffice to say that oxytocin for borderline personality disorder is of great interest but there really is no clinical role for the compound at this time.
References:
- Bertsch, K., & Herpertz, S. C. (2018). Oxytocin and Borderline Personality Disorder. Current topics in behavioral neurosciences, 35, 499–514.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 13
So, the key points from this section is that these are medications under investigation for borderline personality disorder.
They may be helpful in the future as they point to new pathologic mechanisms.
For example, glutamate transmission may be important in borderline personality disorder.
Slide 12 of 13
Omega-3 fatty acids are particularly of interest. There has been some evidence they can decrease depression, suicidality, or affective instability in borderline patients.
Stimulant therapy can be useful for borderline patients who have comorbid ADHD and the example given is you really want to pay attention to how much their functioning improves.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.