Slides and Transcript
Slide 1 of 17
Welcome back those who are auditing this algorithm for the pharmacotherapy of OCD. And this is video 2 of that algorithm and it’s about comorbidities and other circumstances that could lead to variations in the treatment algorithm.
Slide 2 of 17
Now, I haven’t presented the algorithm in detail as yet but as you proceed to the second step of the algorithm after diagnosing OCD you do also need to consider what comorbidities that might be present could affect the choices in the algorithm and could lead to deviations from the standard recommendations for the case that has no comorbidities.
So screen for and treat medical comorbidities to start with. There may be some that could significantly impact the capacity to respond to treatment.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 17
A few that I’m going to discuss in more detail though start with women of childbearing potential which isn’t a comorbidity. It’s really like a circumstance and pregnant women are included in this category.
So, they have some special considerations because late exposure to SSRIs may increase risks of neonatal complications including premature delivery, decreased body weight of the infants, and persistent pulmonary hypertension.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
Slide 4 of 17
So this is an association that has been found with late prescription of SSRIs and these outcomes.
But that doesn’t mean it’s a cause-and-effect relationship. There’s confounding by indication. In other words, the reason that people were prescribed an antidepressant may be the reason why they’re at higher risk for these outcomes and not the use of the antidepressant itself.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 17
Now in these various observational studies that are done in pregnant women, they usually try to have a control group that they compare to the pregnant women getting the medication to see if there are differences in their outcomes versus the ones getting the SSRIs.
We have to go by these observational studies as the best that we have and they are confounded by indication.
There were no differences in neonatal outcomes including birth weight, gestational age, or need for a neonatal ICU admission though in women treated with pharmacotherapy. So at least, some of the major concerns associated with medication in pregnancy did not seem to occur with SSRIs.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.5
Slide 6 of 17
We would though avoid paroxetine. It has a D rating in the old rating system that the FDA used for pregnancy risk. D used to mean that there are some known risks, significant risks of fetal harm.
And with paroxetine, the fetal harm was atrial septal cardiac defects being found at higher incidence than expected.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 17
So we think you should not use paroxetine in pregnancy or if a woman is on it, happens to be on it and gets pregnant, we would consider switching off it to something that might be safer.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 8 of 17
Overall though, the risk to the newborn of untreated OCD and having the pregnant woman go through pregnancy while exhibiting significant OCD symptoms may outweigh the risks of medication treatment of that OCD.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 17
That’s a tough decision to make. It certainly should be made in collaboration with the patient and significant others of the patient as well as the prescriber.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 10 of 17
A psychiatric comorbidity that I want you to identify immediately before starting treatment is bipolar disorder, a disorder which by the way is frequently misdiagnosed and missed.
Especially when people are having depressions, there’s a failure to recognize that there may also be hypomanias going on and these are really bipolar depressions.
References:
- Pacchiarotti, I., Bond, D. J., Baldessarini, R. J., Nolen, W. A., Grunze, H., Licht, R. W., Post, R. M., Berk, M., Goodwin, G. M., Sachs, G. S., Tondo, L., Findling, R. L., Youngstrom, E. A., Tohen, M., Undurraga, J., González-Pinto, A., Goldberg, J. F., Yildiz, A., Altshuler, L. L., … Vieta, E. (2013). The international society for bipolar disorders (ISBD) task force report on antidepressant use in bipolar disorders. American Journal of Psychiatry, 170(11), 1249-1262.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 17
So carefully diagnose whether there’s bipolar disorder before commencing treatment for OCD with an antidepressant because we don’t recommend antidepressants if you have bipolar disorder.
They may shift euthymic patients with bipolar disorder toward more manic episodes especially in the second six months of treatment even if they’re also on a mood stabilizer.
And also, there are recurring depressions in people with bipolar. SSRIs may cause more cycling back to depression. So we prefer not to use them even though they’re prominent in the algorithm.
References:
- Pacchiarotti, I., Bond, D. J., Baldessarini, R. J., Nolen, W. A., Grunze, H., Licht, R. W., Post, R. M., Berk, M., Goodwin, G. M., Sachs, G. S., Tondo, L., Findling, R. L., Youngstrom, E. A., Tohen, M., Undurraga, J., González-Pinto, A., Goldberg, J. F., Yildiz, A., Altshuler, L. L., … Vieta, E. (2013). The international society for bipolar disorders (ISBD) task force report on antidepressant use in bipolar disorders. American Journal of Psychiatry, 170(11), 1249-1262.
- El-Mallakh, R. S., Vöhringer, P. A., Ostacher, M. M., Baldassano, C. F., Holtzman, N. S., Whitham, E. A., Thommi, S. B., Goodwin, F. K., & Ghaemi, S. N. (2015). Antidepressants worsen rapid-cycling course in bipolar depression: A STEP-BD randomized clinical trial. Journal of Affective Disorders, 184, 318-321.
Slide 12 of 17
So what do we have for bipolar patients with OCD?
Well, what we have is psychosocial treatments, psychotherapy. CBT is well established as effective. I think that would be first line. And we would not use antidepressants.
References:
- Pacchiarotti, I., Bond, D. J., Baldessarini, R. J., Nolen, W. A., Grunze, H., Licht, R. W., Post, R. M., Berk, M., Goodwin, G. M., Sachs, G. S., Tondo, L., Findling, R. L., Youngstrom, E. A., Tohen, M., Undurraga, J., González-Pinto, A., Goldberg, J. F., Yildiz, A., Altshuler, L. L., … Vieta, E. (2013). The international society for bipolar disorders (ISBD) task force report on antidepressant use in bipolar disorders. American Journal of Psychiatry, 170(11), 1249-1262.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 17
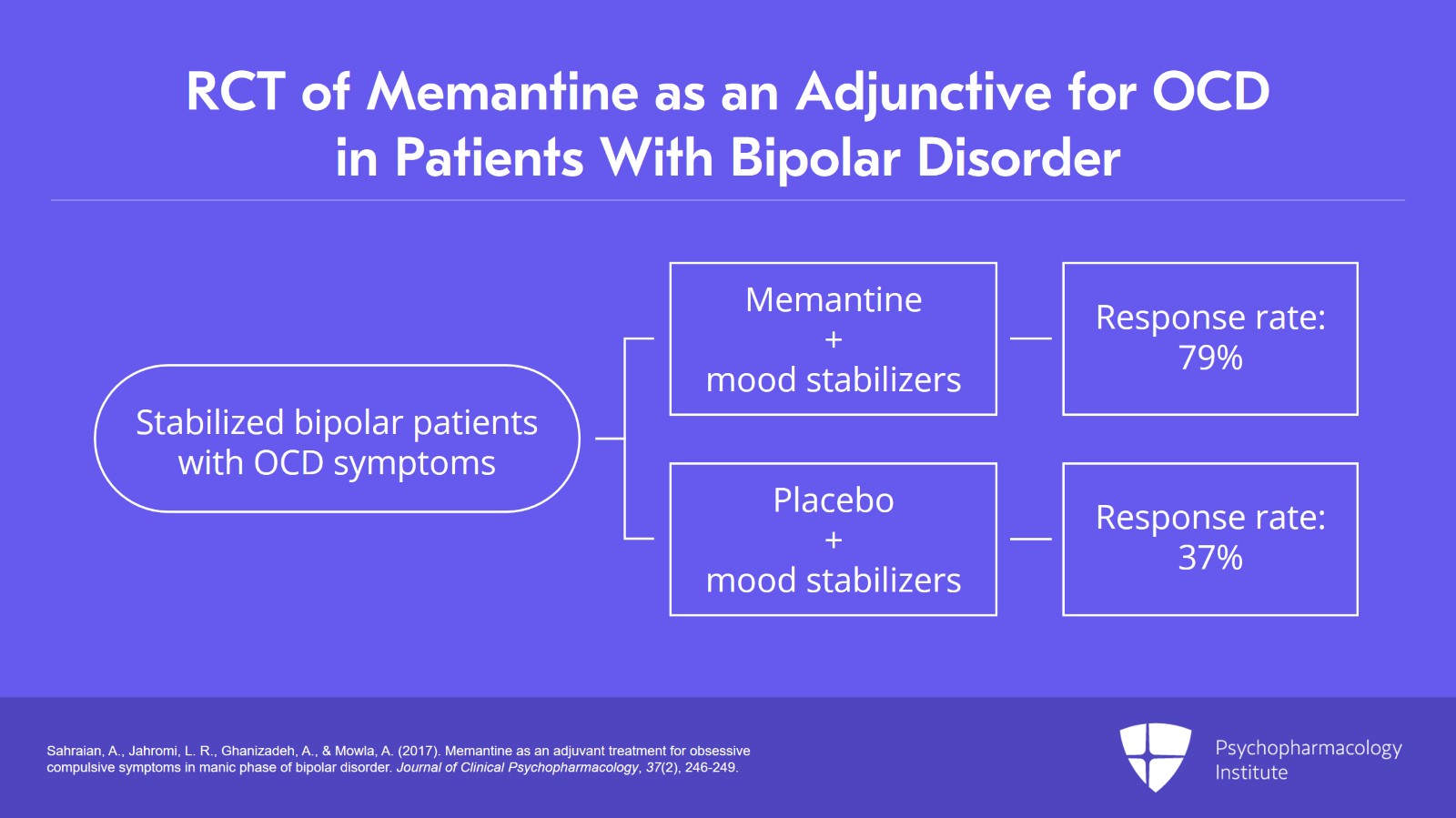
Now as far as what medication you could use, we have one randomized controlled trial with memantine 20 mg a day added to mood stabilizers as an adjunctive agent to the OCD in treating OCD symptoms in manic patients.
They had a response rate of 79% in the memantine group and 37% in the placebo group. There were a few side effects but it was a small study, only 38 patients. So that’s the evidence base that we have for pharmacotherapy of OCD in people with bipolar disorder.
References:
- Sahraian, A., Jahromi, L. R., Ghanizadeh, A., & Mowla, A. (2017). Memantine as an adjuvant treatment for obsessive compulsive symptoms in manic phase of bipolar disorder. Journal of Clinical Psychopharmacology, 37(2), 246-249.
Slide 14 of 17
So to conclude this second video, the key points that were made, number one, as you prepare to choose treatment for your OCD patient consider various medical and psychiatric comorbidities.
Regarding women who could become pregnant the risks are mild on fetal defects except for paroxetine which has significant risks of fetal harm.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 17
Generally, the benefits are worth the risks of SSRI treatment but it’s a collaborative decision with the prescriber, the patient, and family.
Slide 16 of 17
And regarding bipolar disorder as a comorbidity, we do not recommend using any antidepressants.
Instead, we recommend cognitive behavioral psychotherapy.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.