Slides and Transcript
Slide 1 of 15
Okay. Our next section, section 5, is going to be drilling a little further into the issue of nonadherence and how clinicians might handle different components of that. We’ll talk about adverse drug reactions, measuring perceived side effects. I’m going to talk about FIBSER, a tool that I like, and communication about side effects.
Slide 2 of 15
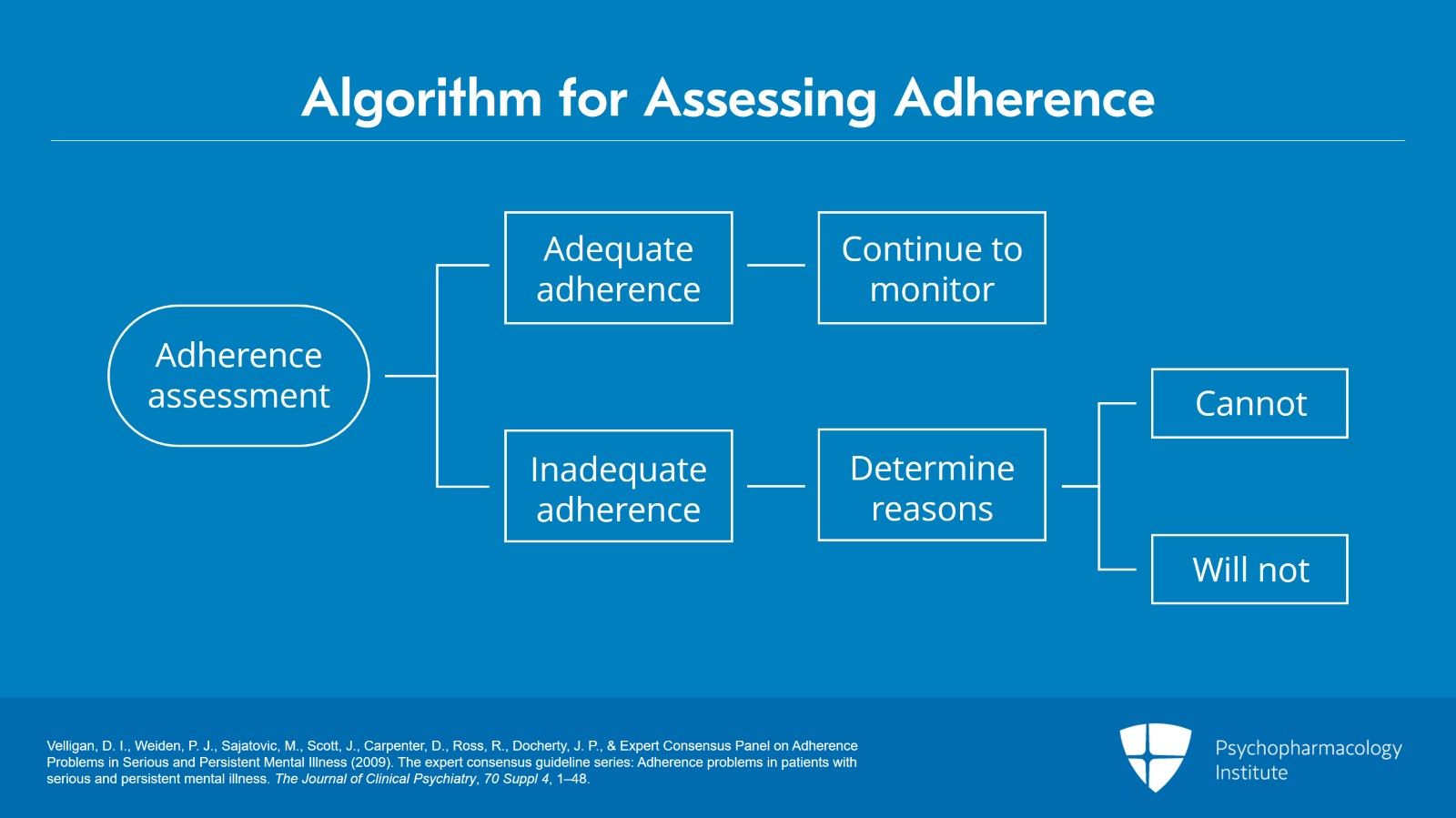
So here in our next slide, we have an adherence algorithm, and this is how a clinician might think about adherence assessment. So, as I’ve mentioned before, assessing adherence is hard and needs to be done repeatedly. One way to think about it is a patient that appears to have adequate adherence in your opinion, in that case, you would just continue to routinely monitor adherence. Or if a person appears to have inadequate adherence, then you might further go into that to try to figure out the reasons for presumed suboptimal adherence.
So, one major way that I think about it is the person can’t versus they won’t take medication.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., Docherty, J. P., & Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009). The expert consensus guideline series: Adherence problems in patients with serious and persistent mental illness. The Journal of Clinical Psychiatry, 70 Suppl 4, 1–48.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
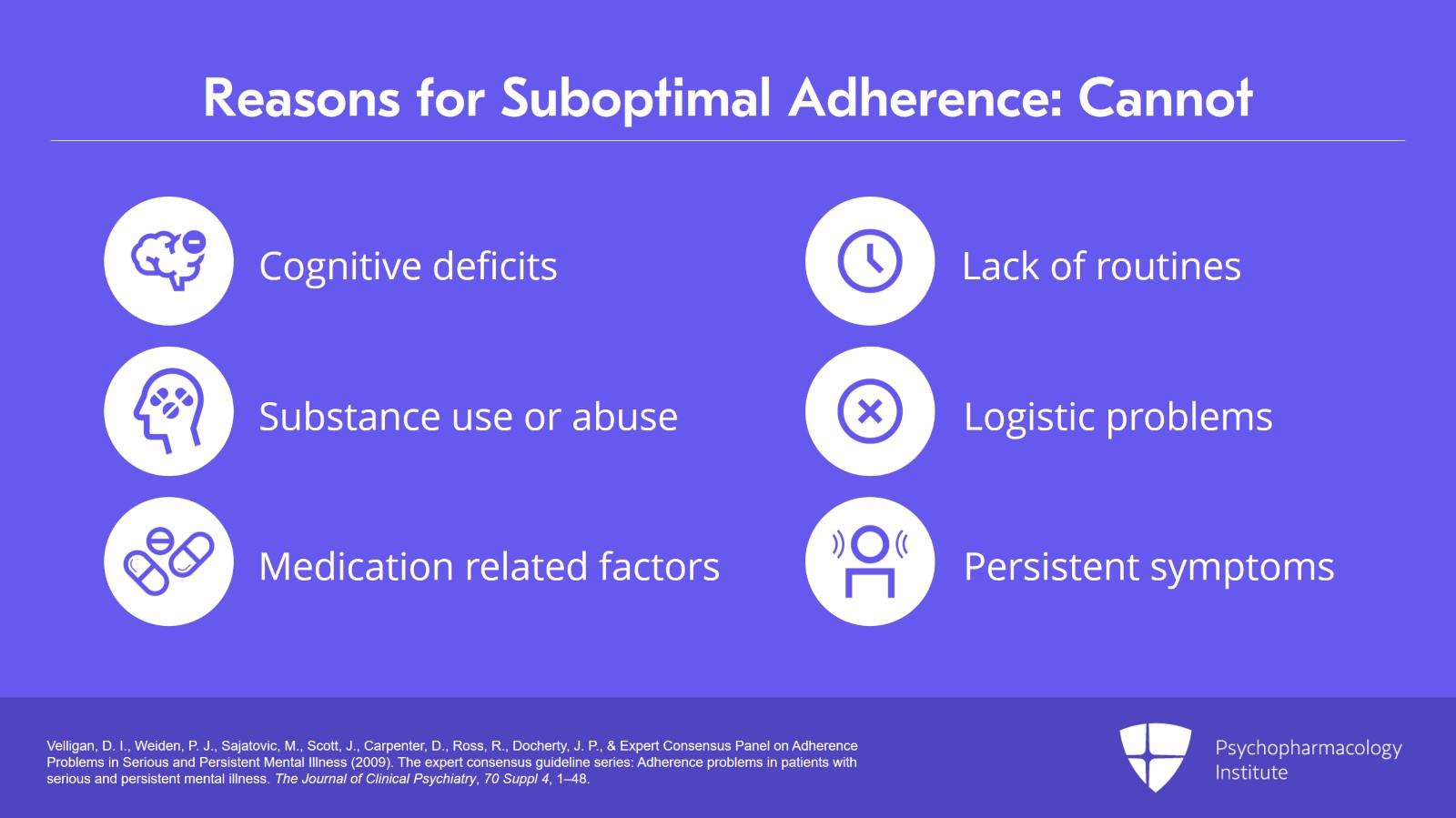
So cannot, those categories could be cognitive deficits, substance use or abuse, medication-related factors. They may have tolerability issues. They just might have adverse events or intolerance to medication. Their life may be very chaotic. They may have a lack of routines. There could be logistic problems. Maybe they can’t afford their medications.
They could have persistent symptoms that might make it tough for them to take medications. Maybe they’re paranoid about the drugs for instance.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., Docherty, J. P., & Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009). The expert consensus guideline series: Adherence problems in patients with serious and persistent mental illness. The Journal of Clinical Psychiatry, 70 Suppl 4, 1–48.
Slide 4 of 15
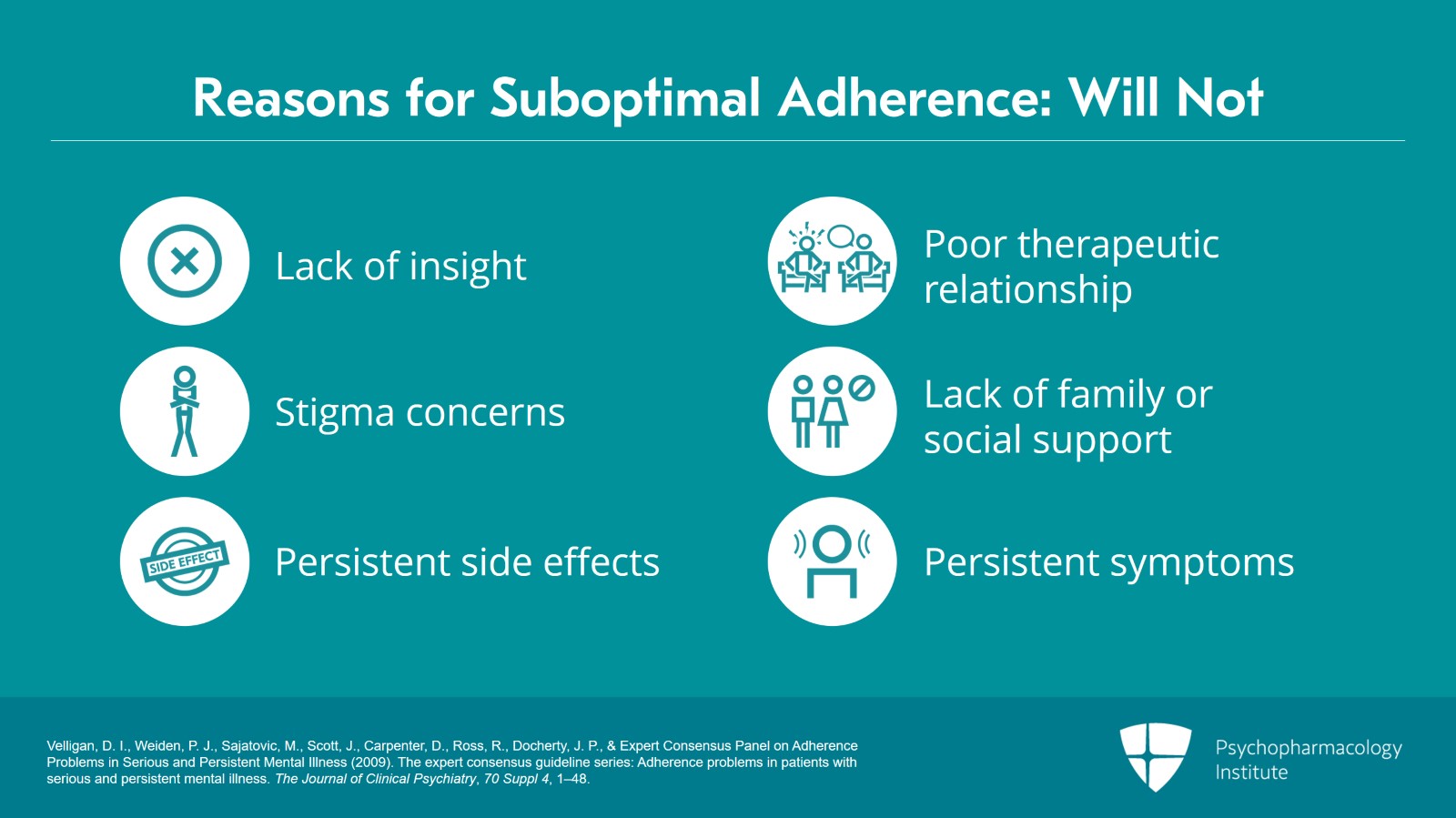
Or they will not take the medication and that could include lack of insight, stigma concerns. Persistent side effects could go into this. A poor therapeutic relationship, lack of family or social supports and again, persistent symptoms also.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., Docherty, J. P., & Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009). The expert consensus guideline series: Adherence problems in patients with serious and persistent mental illness. The Journal of Clinical Psychiatry, 70 Suppl 4, 1–48.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
So ideally, you want to tailor the interventions to address the specific causes of suboptimal adherence based on those variety of factors. And I do want to say that even though we have this nice little algorithm here, often we can have people that might have some reasons for poor adherence that are in the Cannot profile as well as in the Will Not profile. So that makes things a little bit more challenging for the clinician.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., Docherty, J. P., & Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009). The expert consensus guideline series: Adherence problems in patients with serious and persistent mental illness. The Journal of Clinical Psychiatry, 70 Suppl 4, 1–48.
Slide 6 of 15
So, the next thing that I want to talk about in this section is adverse drug reactions as a function of increasing age.
So, side effects often are not significant in younger people.
Right around the age of 50, adverse drug reactions or ADRs per 10,000 of the population really skyrocket. For those of us, yours truly included, who are above that category, we definitely notice that there are aging-related changes and increased likelihood of ADRs is one of those.
So, thinking back to our case reports, you know, in Marie, as she got older, she started to have more problems with taking lithium.
References:
- Ghose, K. (1991). The need for a review Journal of drug use and the elderly. Drugs & Aging, 1(1), 2-5.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
The other thing I want to talk about is measuring perceived side effects so particularly for people that might be in that older age window where they are more likely but also across the full lifespan.
The STAR*D study for unipolar depression used a scale called the Frequency, Intensity and Burden of Side Effects Rating Scale or FIBSER. It can assess and consider tolerability of side effects to weigh the cost and benefit of a dose change.
We know that side effects can impact quality of life and treatment adherence in mood disorders as in any disorder. And FIBSER really can be used if you tweak the words a little bit for any kind of psychotropic medication or psychiatric disorder.
References:
- Wisniewski, S. R., Rush, A. J., Balasubramani, G. K., Trivedi, M. H., Nierenberg, A. A., & STARD Investigators (2006). Self-rated global measure of the frequency, intensity, and burden of side effects. Journal of Psychiatric Practice, 12(2), 71–79.
Slide 8 of 15
So, here’s an example. Number one, choose the response that best describes the frequencies or how often of the side effects of the medication you have taken within the past week for your depression. You could substitute a different psychiatric illness. And so, the person says whether they have no side effects or the other extreme, present all the time.
And then question two, describe the intensity of the side effects, so how severe. Is it trivial, moderate, marked, severe, intolerable?
Third question is choose the response that best describes the degree to which the side effects have occurred and impaired you over the last week. So how much interference has the side effect impacted your functioning, so from no impairment all the way to the extreme of unable to function due to side effects?
References:
- Wisniewski, S. R., Rush, A. J., Balasubramani, G. K., Trivedi, M. H., Nierenberg, A. A., & STARD Investigators (2006). Self-rated global measure of the frequency, intensity, and burden of side effects. Journal of Psychiatric Practice, 12(2), 71–79.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
So, that could be a tool and a point of discussion. It can help you decide with your patient whether a particular side effect is tolerable or not. Is it going to be a key driver in poor adherence? And it really can take the focus away from being judgmental, or whether somebody’s a bad doctor or a bad patient. It really is designed to jumpstart that discussion and can be very helpful in treatment decision making.
References:
- Wisniewski, S. R., Rush, A. J., Balasubramani, G. K., Trivedi, M. H., Nierenberg, A. A., & STARD Investigators (2006). Self-rated global measure of the frequency, intensity, and burden of side effects. Journal of Psychiatric Practice, 12(2), 71–79
Slide 10 of 15
The other thing that could be a tool is helping individuals to communicate with providers about side effects and we do this in some of our adherence promotion programs.
We ask people to be clear on a generic and a chemical name. So, we have definitely seen patients who do not appreciate, especially if they’ve gotten drugs from different pharmacies, that the same drug can have different names. So, it’s important that people understand that what the medication is typically intended to treat as well as the purpose of the medication in their situation. So, is it an antidepressant, is it a general mood stabilizer and so on?
References:
- Sajatovic, M., Levin, J., Fuentes-Casiano, E., Cassidy, K. A., Tatsuoka, C., & Jenkins, J. H. (2011). Illness experience and reasons for nonadherence among individuals with bipolar disorder who are poorly adherent with medication. Comprehensive Psychiatry, 52(3), 280-287.
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
Their personal response to the medication, asking the patient to quantify the side effect or problems.
So, this is a little similar to the FIBSER. Is it a mild, moderate or severe side effect?
Suggestions from their treatment provider about how to manage these side effects. You know, is this something that just needs to be tolerated because there are no other choices? Or you know, is there something that the person can do? You know, maybe they could take it at a different time or other alternatives.
And then side effects that the person has not personally experienced but which they are concerned about or fear may happen in the future.
So, for example, some patients with bipolar disorder are afraid of taking lithium because they’ve heard very bad stories about it and are fearful that those things could happen to them. So basically, good effects, bad effects and, what have you experienced.
References:
- Sajatovic, M., Levin, J., Fuentes-Casiano, E., Cassidy, K. A., Tatsuoka, C., & Jenkins, J. H. (2011). Illness experience and reasons for nonadherence among individuals with bipolar disorder who are poorly adherent with medication. Comprehensive Psychiatry, 52(3), 280-287.
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Slide 12 of 15
There’s no one approach to managing side effects. It really depends on the patient, their circumstance. The number one thing is that patients and clinicians need to communicate about options and potential solutions.
References:
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
So, the key points here are while there are many reasons for poor adherence, and these vary on individual patient circumstances, experience, medications, or side effects that patients are concerned about, they can drive adherence behaviors.
Patients can vote with their feet. They can stop taking medications due to side effects. And there are tools like the FIBSER that clinicians can use to help understand the burden and impact of side effects.
Slide 14 of 15
And then finally, shared decision making between patients and clinicians may help identify how best to balance benefit versus burden of a given medication regimen.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.