Slides and Transcript
Slide 1 of 12
Hi everybody. This is Dr. David Osser again continuing with the video number 7 of the algorithm for the psychopharmacology of obsessive-compulsive disorder.
Slide 2 of 12
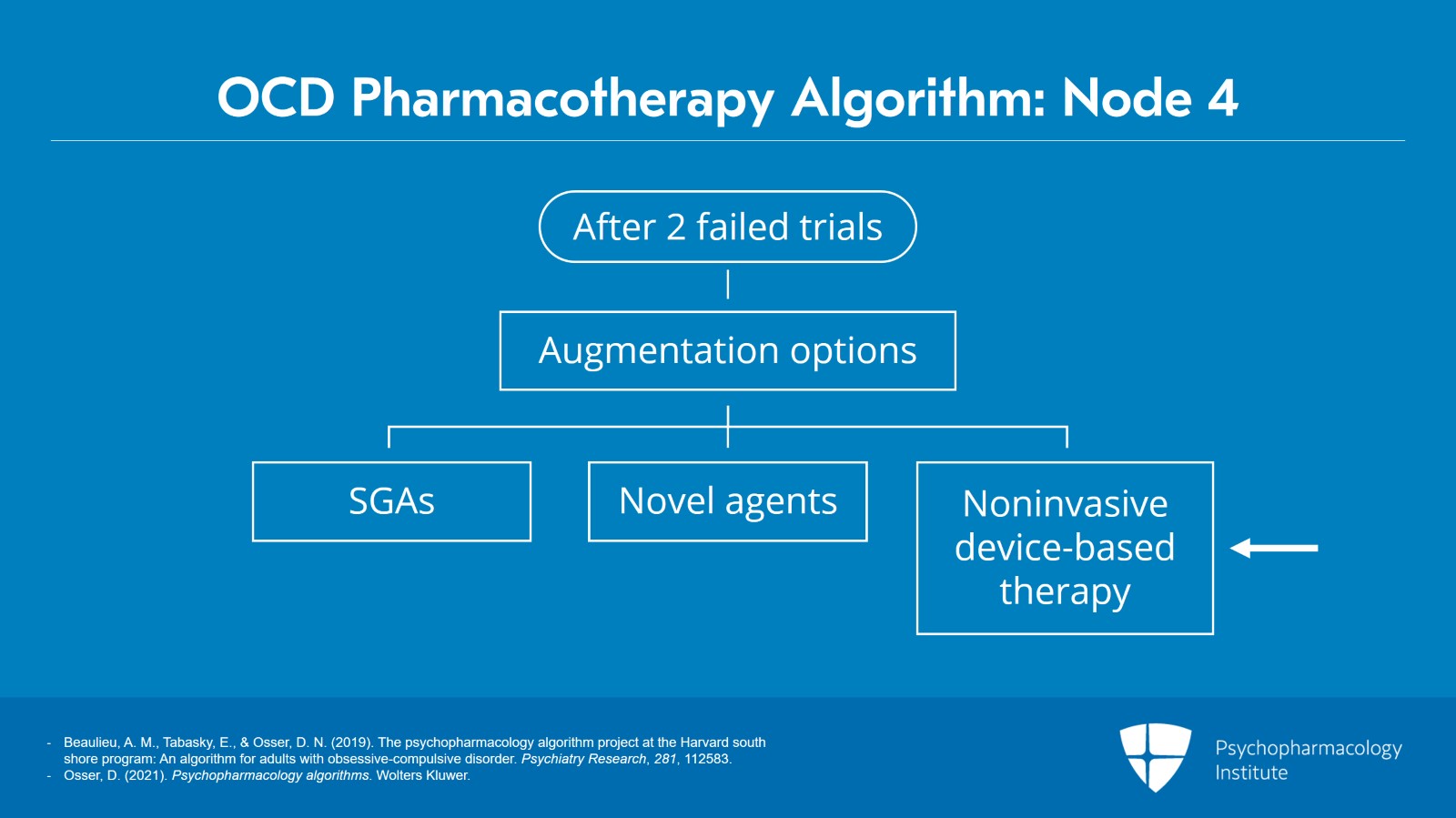
And in the first six videos, we went over in detail how to give two adequate monotherapy trials of medication.
But the evidence that’s available to us on what to do next focuses on augmentations. We have no good evidence that a third monotherapy trial will be helpful.
And we’re at node 4 in the algorithm if you’re following visually on our flowchart which shows with an arrow pointing to the augmentations and we have three kinds of augmentations that we don’t have a preference of one kind versus the other. It’s up to you to decide if you would like to augment with a second-generation antipsychotic, whether you’d like to augment with novel agents, or whether you’d like to augment your SSRI with a noninvasive device-based therapy.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 12
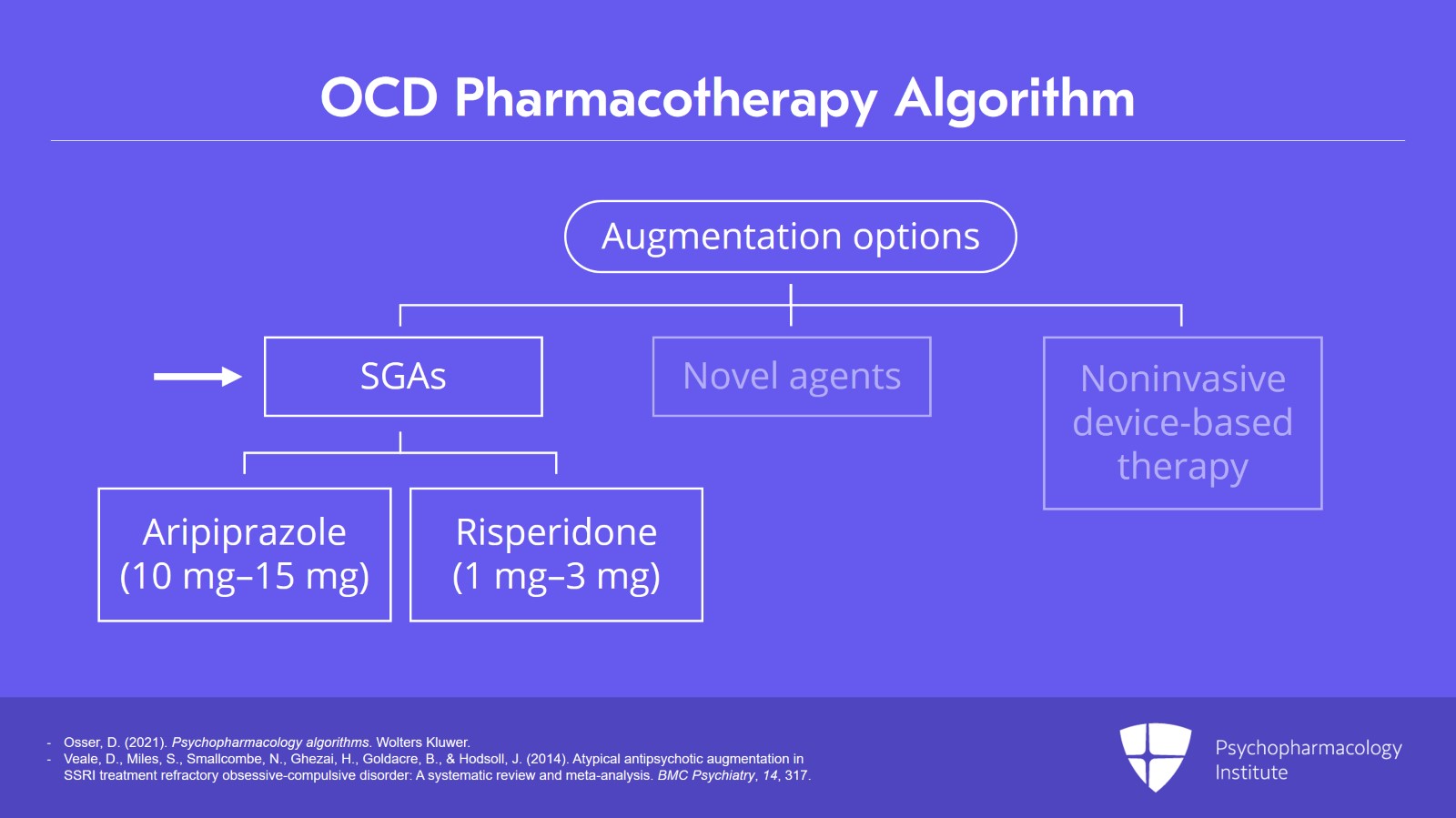
But at node 4, we’ll start with discussing the first type of augmentation which is with an SGA, a second-generation antipsychotic.
The two that have the most evidence of benefit are aripiprazole used at a dose of 10 to 15 mg per day and risperidone used at a dose of 1 to 3 mg per day.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
- Veale, D., Miles, S., Smallcombe, N., Ghezai, H., Goldacre, B., & Hodsoll, J. (2014). Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: A systematic review and meta-analysis. BMC Psychiatry, 14, 317.
Slide 4 of 12
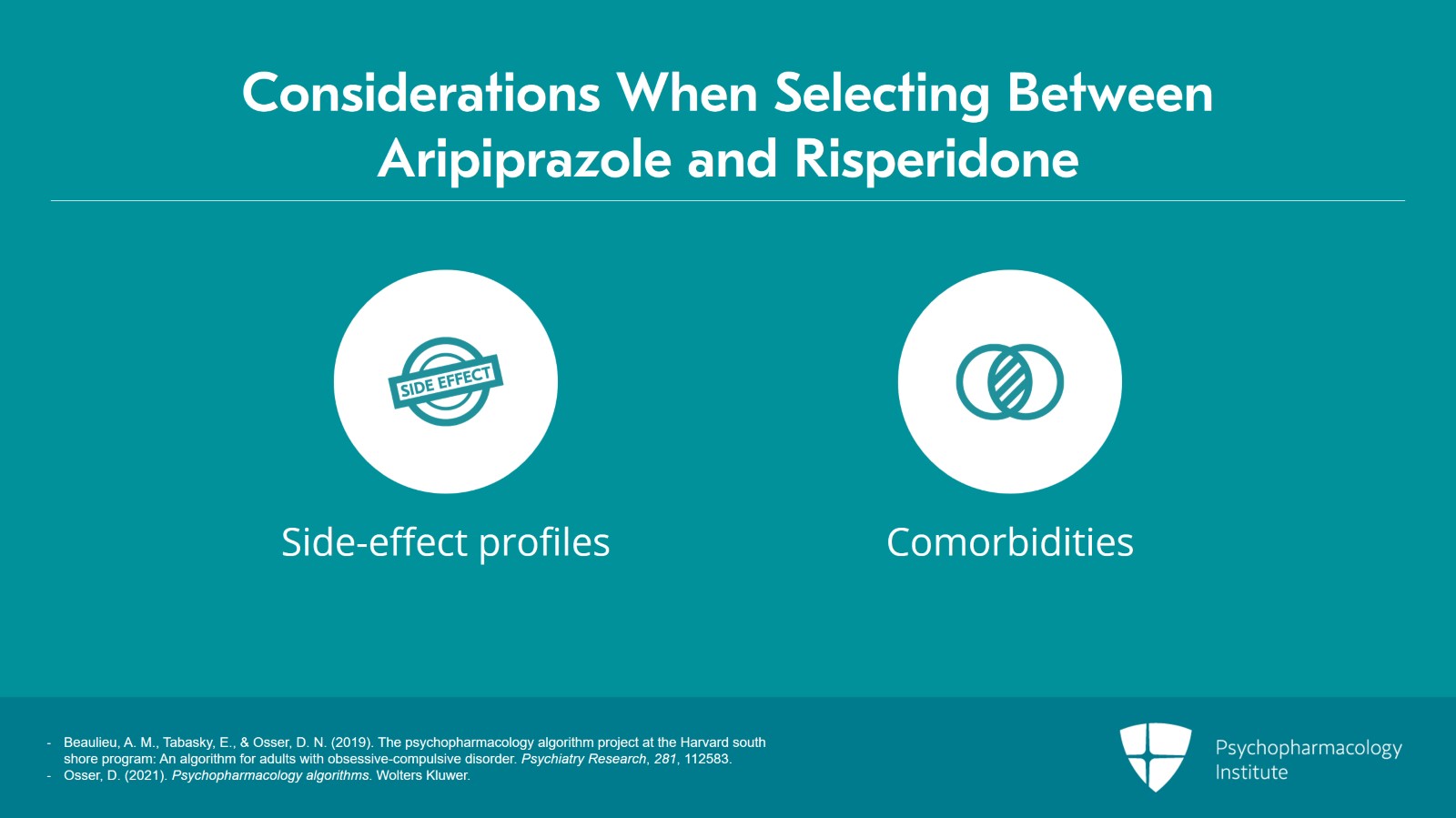
In making your selection between aripiprazole and risperidone consider their side effect profiles and comorbidities they may have when making your selection.
For example, aripiprazole in general has a more tolerable side effect profile although the akathisia could be a problem. It’s got less weight gain than risperidone. That could be a factor in the selection. If they would be vulnerable to dopamine blockade related prolactin elevation side effects that would favor aripiprazole.
So those are the two that have the most benefit to side effect profile.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
Haloperidol has some evidence of efficacy as an augmenter but we do not advise it due to greater long-term concerns with its side effects especially tardive dyskinesia which appears to be greater with haloperidol than with the second-generation products.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 6 of 12
We also will briefly discuss quetiapine and olanzapine.
They both have highly questionable efficacy in studies and both have certainly a moderate to severe amount of side effects.
So we don’t recommend either of them.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
- Diniz, J. B., Shavitt, R. G., Fossaluza, V., Koran, L., Pereira, C. A., & Miguel, E. C. (2011). A double-blind, randomized, controlled trial of fluoxetine plus quetiapine or clomipramine versus fluoxetine plus placebo for obsessive-compulsive disorder. Journal of Clinical Psychopharmacology, 31(6), 763-768.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
Long-term use of antipsychotics in OCD as an augmenter. Beyond short term, there’s very limited effectiveness to the extent that they have done followups of people who have stayed on the augmentation with the antipsychotic. It’s been difficult to demonstrate that it continues to be effective.
But side effects definitely do accumulate over time. So that’s a downside of choosing the antipsychotic augmenters but they have had considerable research.
References:
- Matsunaga, H., Nagata, T., Hayashida, K., Ohya, K., Kiriike, N., & Stein, D. J. (2009). A long-term trial of the effectiveness and safety of atypical antipsychotic agents in augmenting SSRI-refractory obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 70(6), 863–868.
Slide 8 of 12
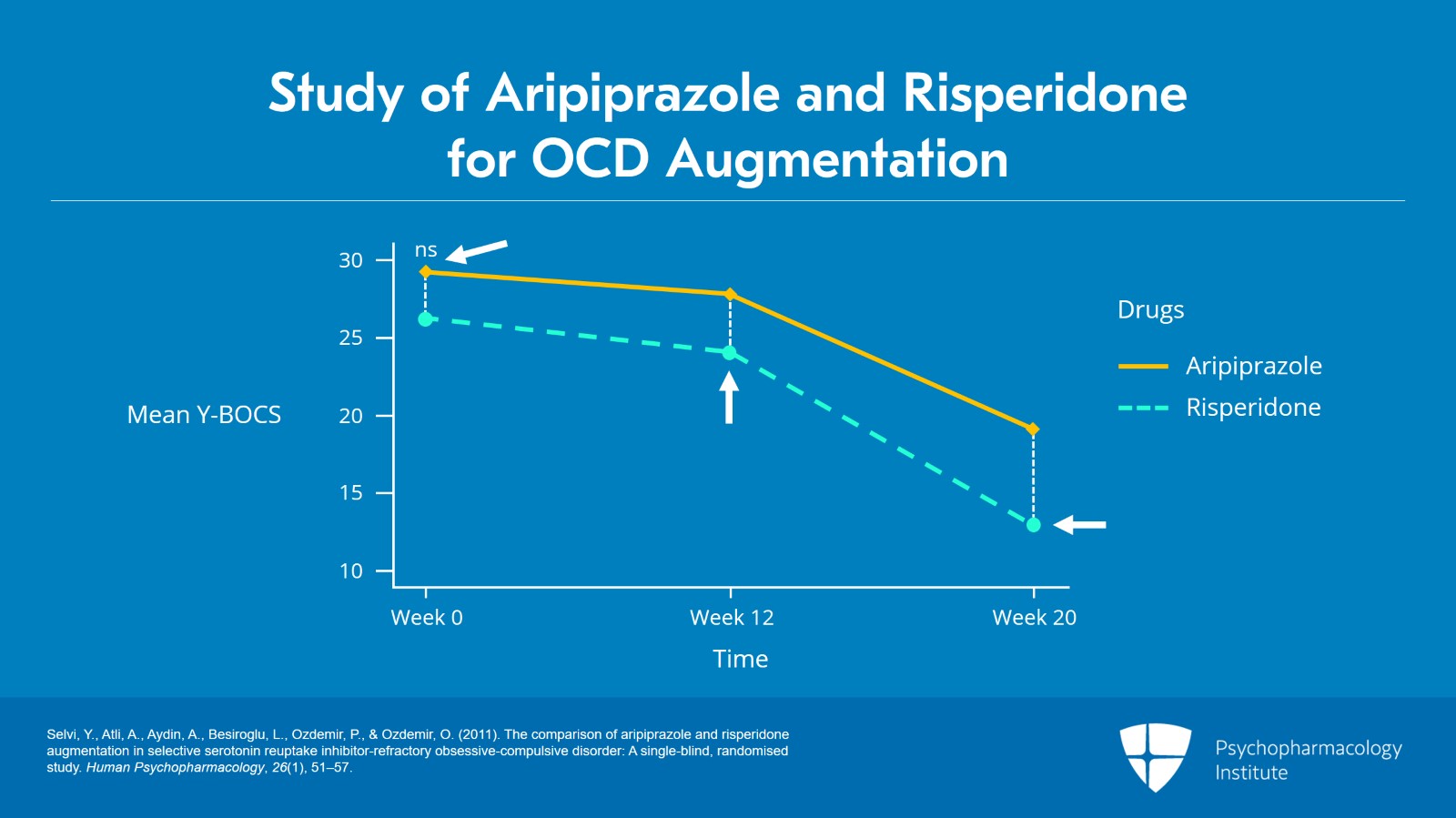
In the next slide, we have a head-to-head study of aripiprazole and risperidone for OCD augmentation.
This study shows that at baseline the group getting aripiprazole was a little sicker. They had 3 points higher in their baseline Y-BOCS scores versus the ones that got risperidone unfortunately so that skews the data a little bit. But yet, by the end of 12 and 20 weeks, there was improvement in both but more improvement in the risperidone group by 1 or 2 Y-BOCS points and it started at a less sick level.
So even though they weren’t as sick, they improved actually a bit more. So with this way of looking at evidence, looking at the one comparative study, risperidone looks a little better.
References:
- Selvi, Y., Atli, A., Aydin, A., Besiroglu, L., Ozdemir, P., & Ozdemir, O. (2011). The comparison of aripiprazole and risperidone augmentation in selective serotonin reuptake inhibitor-refractory obsessive-compulsive disorder: A single-blind, randomised study. Human Psychopharmacology, 26(1), 51–57.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
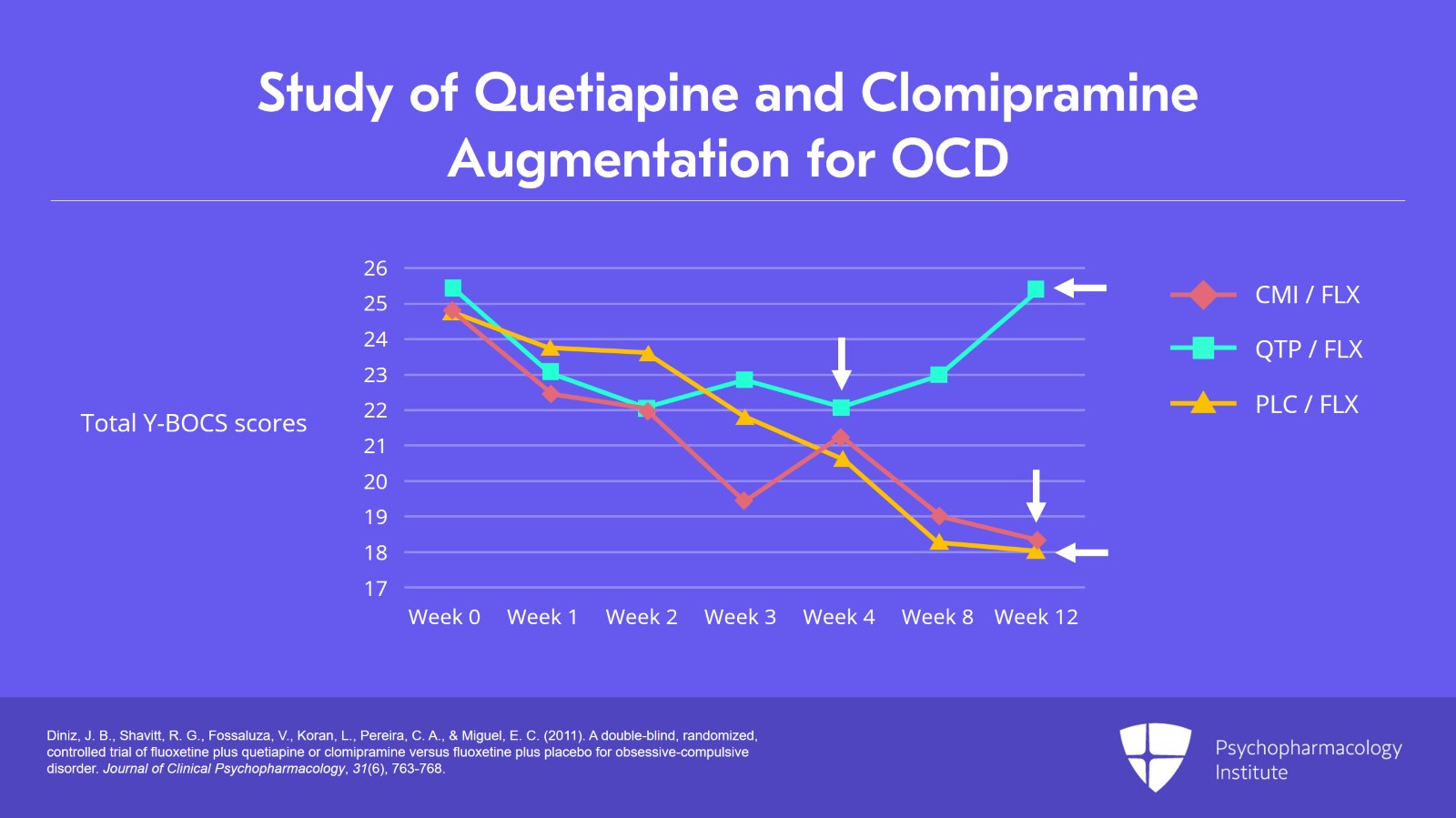
Now, the next slide is important to see because it’s a very interesting three-way augmentation study where they tried two different augmentations and they had a placebo augmentation of SSRI treatment. The two augmenters were quetiapine and clomipramine.
And the slide shows 12 weeks of treatment.
There’s a lot of belief out there that maybe clomipramine added to an SSRI might produce particularly good response.
And as you can see, comparing the placebo line, the placebo patients gradually getting better and remember people do get better on placebo with most of the disorders we treat. So the key thing is whether a drug beats placebo. And you can see the placebo descending nicely over 12 weeks from a Y-BOCS score of 24, 25 at baseline down to 18 by 12 weeks. And you can see the clomipramine patients going in parallel for the most part and winding up at exactly the same spot at 12 weeks as the placebo. No difference on adding clomipramine.
Now, the other augmenter in this study though was the quetiapine. And look what happened to that. Curiously enough after doing just about nothing compared to the placebo for four weeks, when we got to 12 weeks the quetiapine patients are getting worse, much worse. They’re still at baseline at 25 for their score, whereas the placebo people have gone all the way down to 18. What is going on there? I would have to assume the quetiapine is doing something to worsen their OCD compared to what a placebo would do for it.
The bottom line is we don’t recommend quetiapine as an augmenter for OCD.
References:
- Diniz, J. B., Shavitt, R. G., Fossaluza, V., Koran, L., Pereira, C. A., & Miguel, E. C. (2011). A double-blind, randomized, controlled trial of fluoxetine plus quetiapine or clomipramine versus fluoxetine plus placebo for obsessive-compulsive disorder. Journal of Clinical Psychopharmacology, 31(6), 763-768.
Slide 10 of 12
So I’ll summarize the key points of this video which are:
We have three three kinds of augmenters for failed SSRI trials. In this video, we’re concerned with the first of three kinds of augmenters for failed SSRI trials and it’s not necessarily the augmentation of choice.
We talked about risperidone that has the most study and aripiprazole, the second most among SGAs. They both look fairly effective and they both have a significant side effect burden.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
Quetiapine though was inferior to placebo as an augmenter and is best avoided.
Olanzapine was of doubtful effectiveness and has a major side effect and should be avoided as well.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.