Slides and Transcript
Slide 1 of 17
Hi everybody. This is video 5 of the algorithm for the pharmacotherapy of obsessive-compulsive disorder.
Slide 2 of 17
We are looking at the parameters of an adequate trial of an SSRI for OCD and we're recommending that you would first titrate to a standard dose as we defined in video 4, standard dose, not high dose. And for sertraline, for example, that would be 50 to 100. Continue it for five to seven weeks.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 17
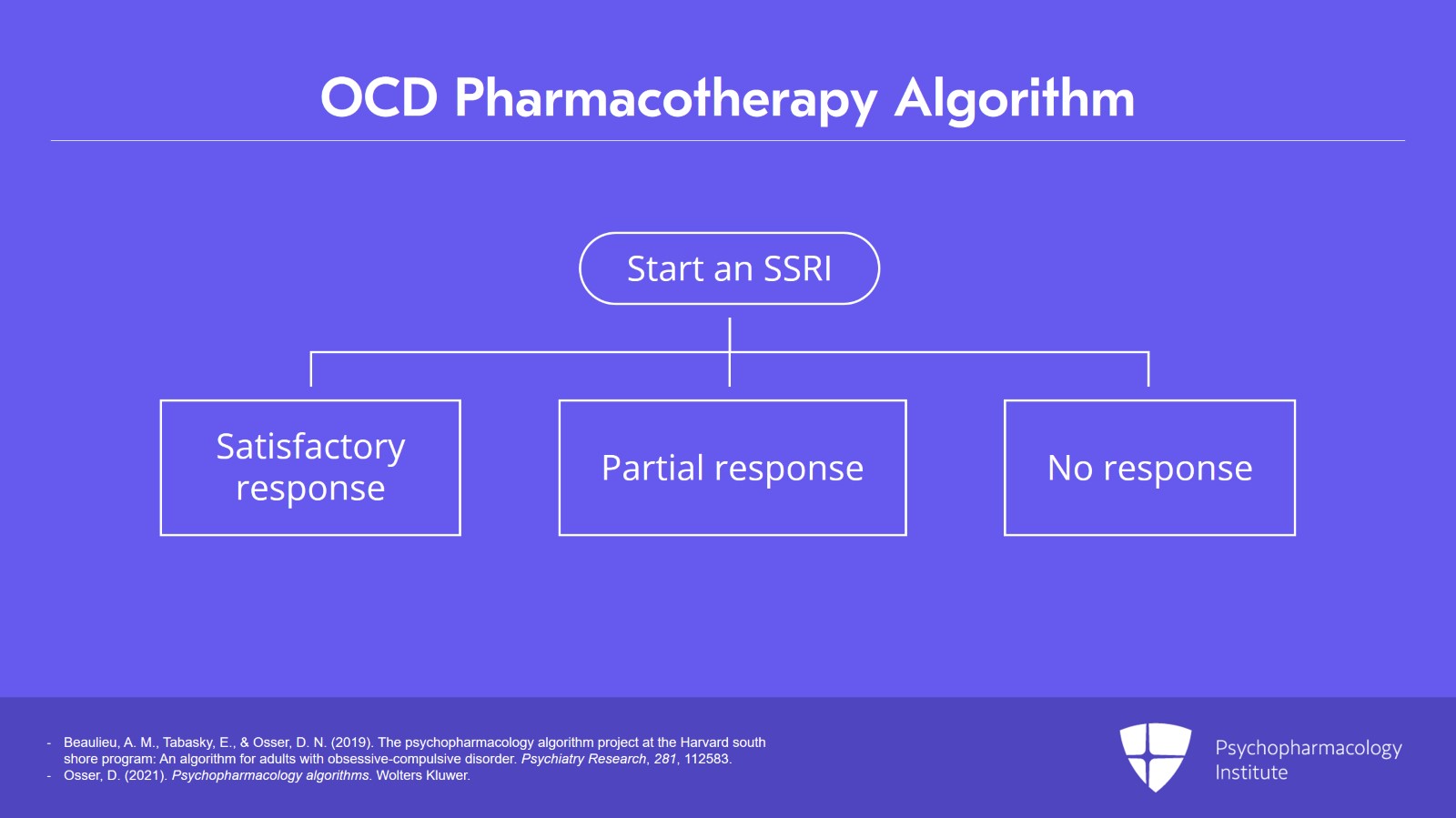
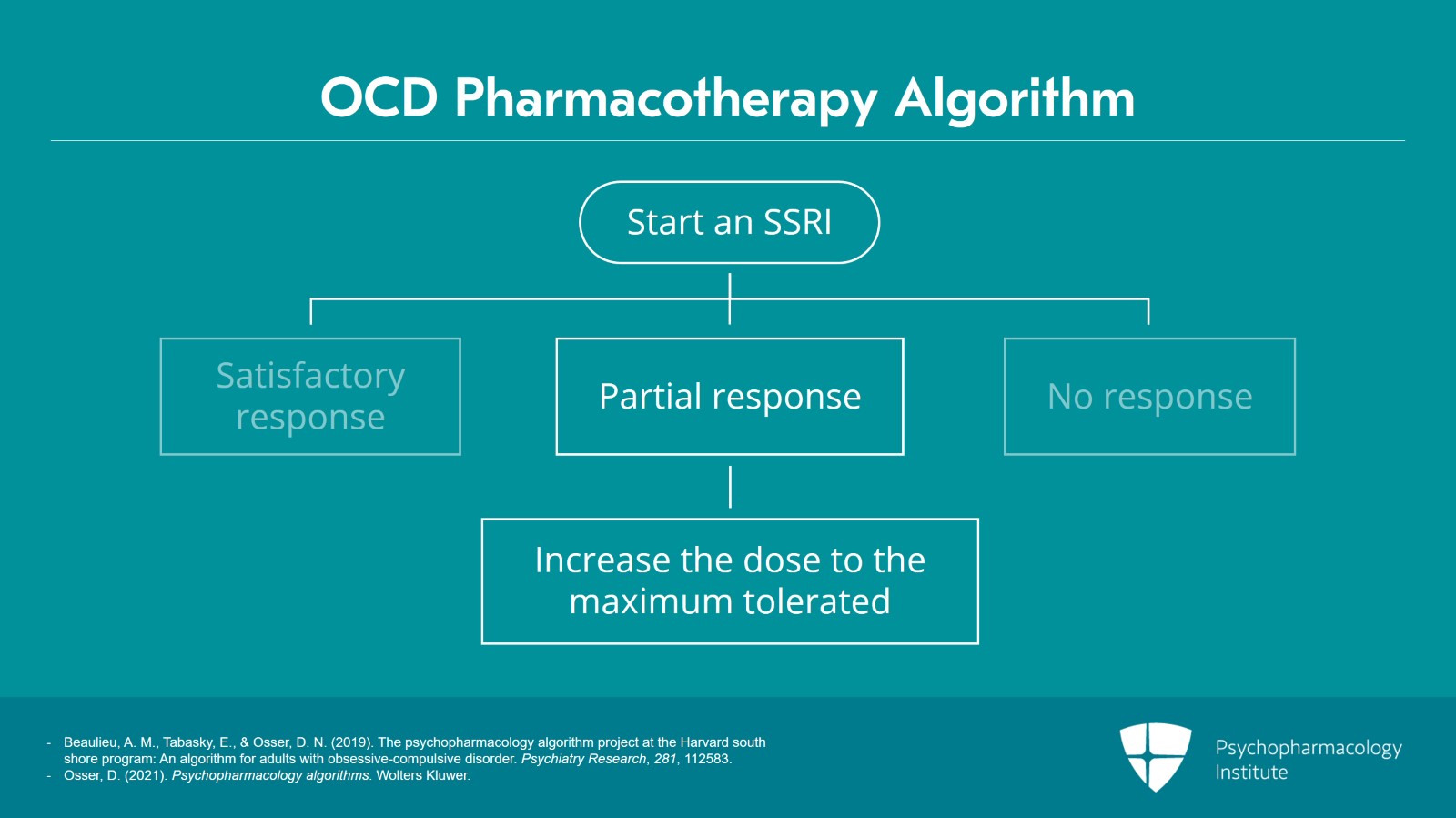
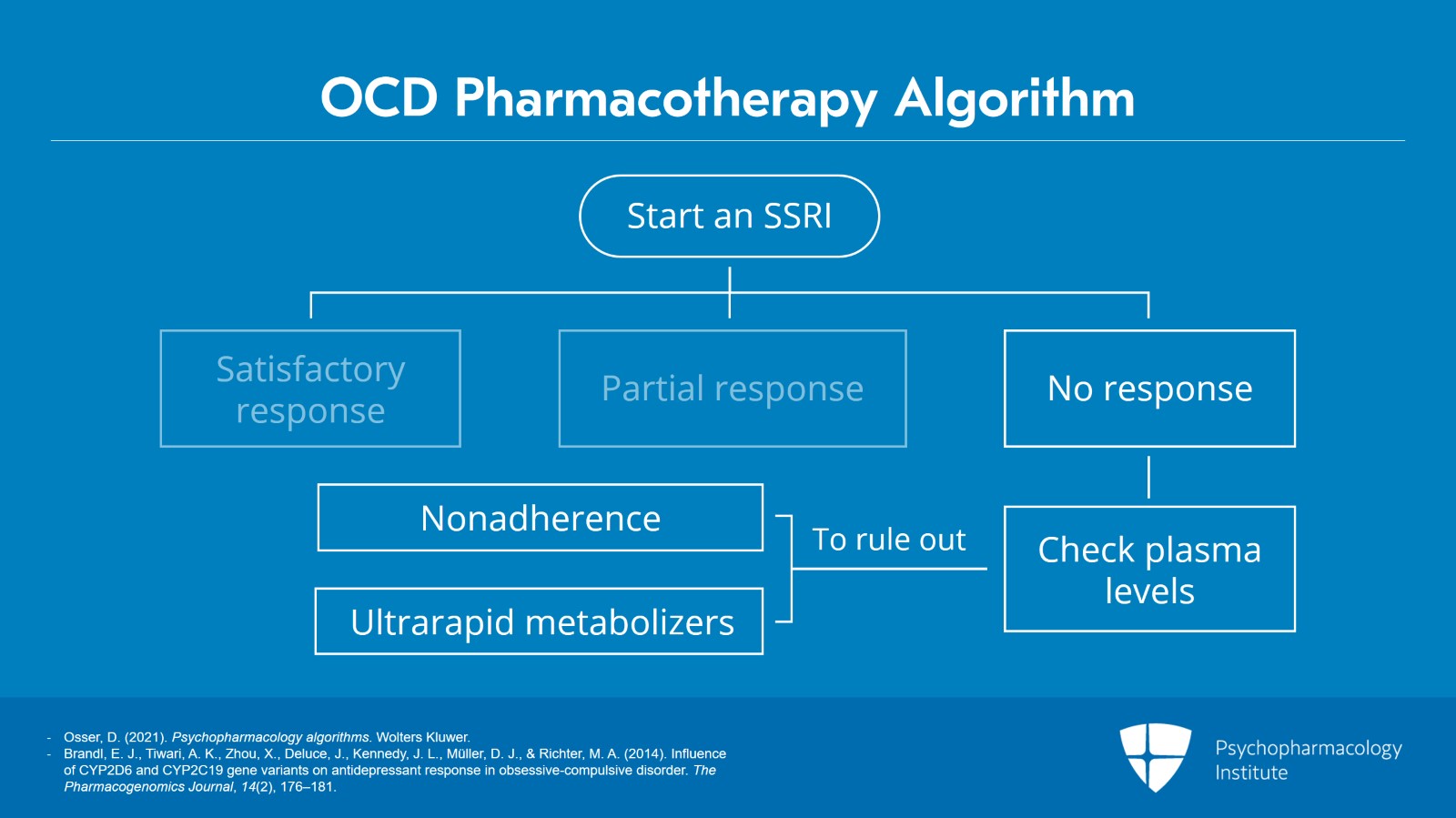
And we have gotten to the point where you have started an SSRI and you are proceeding with standard dosing, the dosing you would use for a major depression treatment and the difference being though that it's longer. There are three possibilities of what could happen as you're proceeding with this trial. You could get a satisfactory response that is adequate and good enough and you're ready to maintain the patient. You also could have a partial response. They're somewhat better but the level of improvement is not deemed adequate or satisfactory. And the third option is you have no response at all. So we're going to discuss each of those options.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 4 of 17
Let's say they had a satisfactory response with the current SSRI. As noted earlier, only 40% achieve improvement that is satisfactory.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 17
There are different definitions of satisfactory if you go by rating scale, Y-BOCS scores. Some will use a 20% improvement in the scale as a good response or satisfactory. Some use 30% or 40%. What's important though is if the patient finds it satisfactory and feel they can live more effectively with this improvement that they've had.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 6 of 17
Limited evidence suggests maintaining improvement for at least one or two years before considering tapering and we support that evidence that you should urge the patient to stay on it for one to two years once they've had this satisfactory response and then they could consider going off it to see if they still need it.
References:
- Ravizza, L., Barzega, G., Bellino, S., Bogetto, F., & Maina, G. (1996). Drug treatment of obsessive-compulsive disorder (OCD): Long-term trial with clomipramine and selective serotonin reuptake inhibitors (SSRIs). Psychopharmacology Bulletin, 32(1), 167–173.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 17
Now, another outcome could be a partial but unsatisfactory improvement. So in these cases, the SSRI may now be gradually increased to the PDR maximum dose if the patient tolerates it. In other words, we are trying to treat them with the standard dose and see if they can get a satisfactory response to that first before going to the high dose. You don't always need higher doses and it's better if you can have success at a lower dose because side effects will be less.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 8 of 17
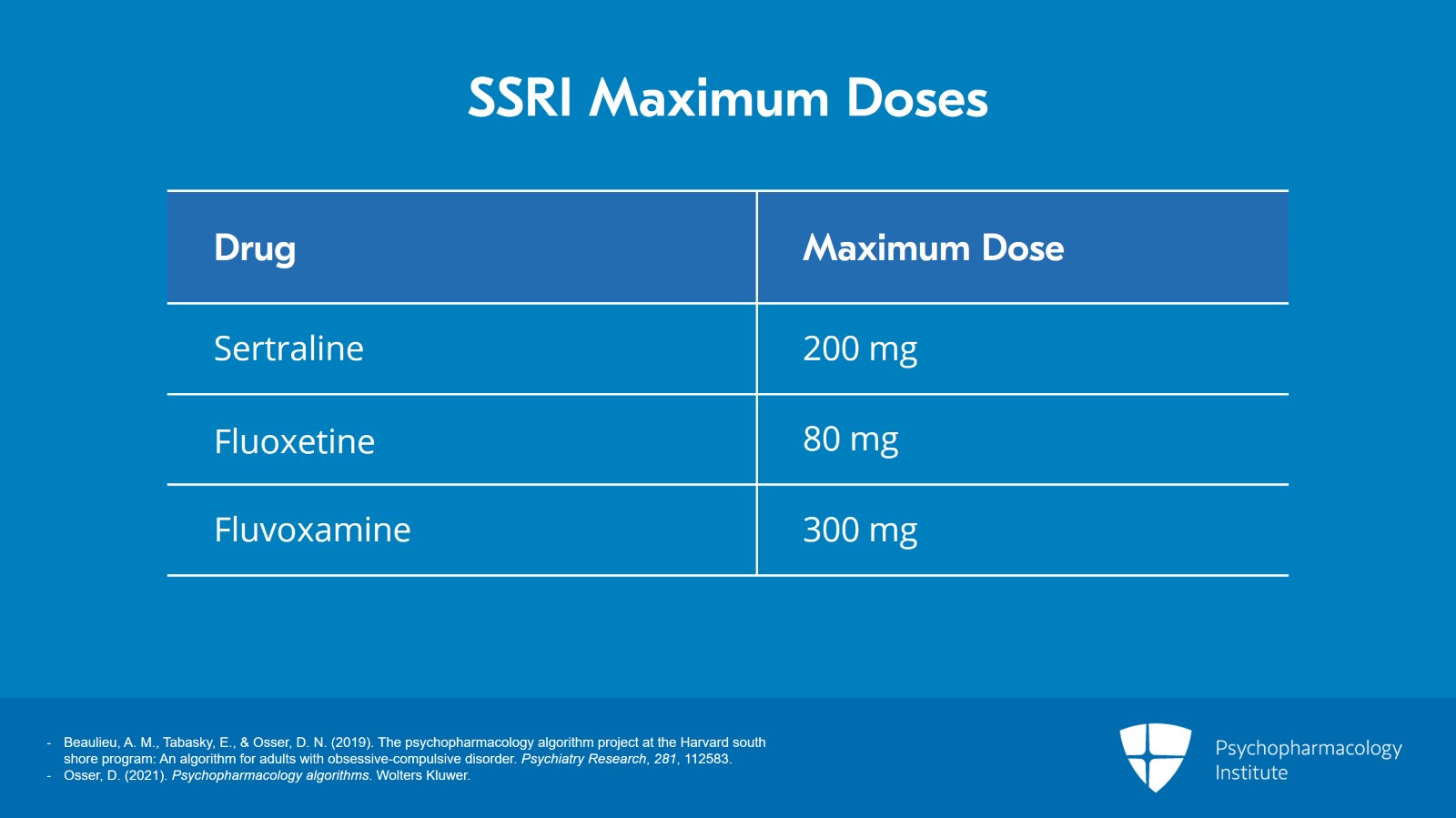
So you can go up to the PDR max which would be 200 for sertraline, 80 for fluoxetine, and 300 for fluvoxamine if tolerated.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 17
But how much better are you going to get with this increase? There was a meta-analysis of the dose-response relationships of SSRIs in OCD by Bloch et al. 10 years ago. And they showed that patients experience a 7% to 9% improvement in their OCD symptoms on the highest dose SSRI. That's probably not a significant difference, the 9 and the 7. But in short, somewhere in that area, 7% to 9%, that's what you can hope for on average for how much more improvement you're going to get from the higher dose.
References:
- Bloch, M. H., McGuire, J., Landeros-Weisenberger, A., Leckman, J. F., & Pittenger, C. (2009). Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder. Molecular Psychiatry, 15(8), 850-855.
Slide 10 of 17
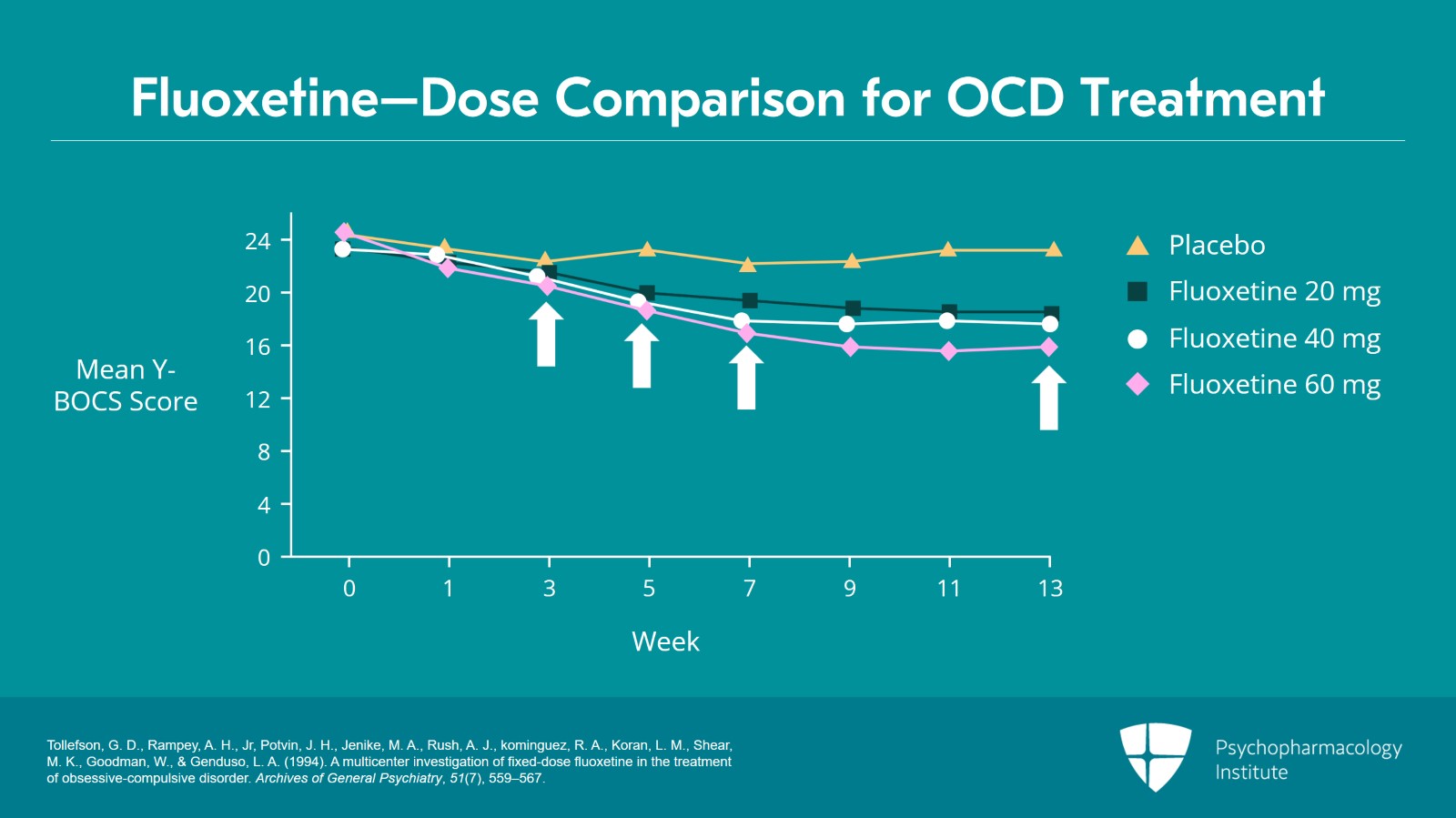
This is the comparison over 13 weeks of three doses of fluoxetine versus placebo. And if you can see the graph, you would notice that over the first three weeks there's absolutely no difference from placebo. But at five weeks, we start to see a separation of the three doses. All three are better than the placebo by several Y-BOCS points at week 5 but the three – the high, low, and medium dose – are all exactly the same. It's only when you get to week 7 that there's a little bit of pulling ahead of the Y-BOCS improvement from the 40 and 60 mg fluoxetine versus the 20. And then between week 7 and 13, things stayed pretty much the same. The three doses are all actually improving versus the placebo to an equal degree but the difference between the three doses is still only 2 points, maybe 2.5 points on the Y-BOCS which is that 7% to 9% I was talking about.
References:
- Tollefson, G. D., Rampey, A. H., Jr, Potvin, J. H., Jenike, M. A., Rush, A. J., kominguez, R. A., Koran, L. M., Shear, M. K., Goodman, W., & Genduso, L. A. (1994). A multicenter investigation of fixed-dose fluoxetine in the treatment of obsessive-compulsive disorder. Archives of General Psychiatry, 51(7), 559–567.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 17
The third possibility is that you got no response at all. Nothing's happening after five or six weeks. We recommend getting a plasma level to rule out a number of things that could be going on for why you're getting no response. Number one is nonadherence. Many patients don't take the medications that we give them and don't tell you that they're not taking it. The second reason is that you could be dealing with an ultrarapid metabolizer of your SSRI which is present in, depending on the ethnic population you're seeing it could be present in up to 10% of patients depending on the cytochrome enzyme involved.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
- Brandl, E. J., Tiwari, A. K., Zhou, X., Deluce, J., Kennedy, J. L., Müller, D. J., & Richter, M. A. (2014). Influence of CYP2D6 and CYP2C19 gene variants on antidepressant response in obsessive-compulsive disorder. The Pharmacogenomics Journal, 14(2), 176–181.
Slide 12 of 17
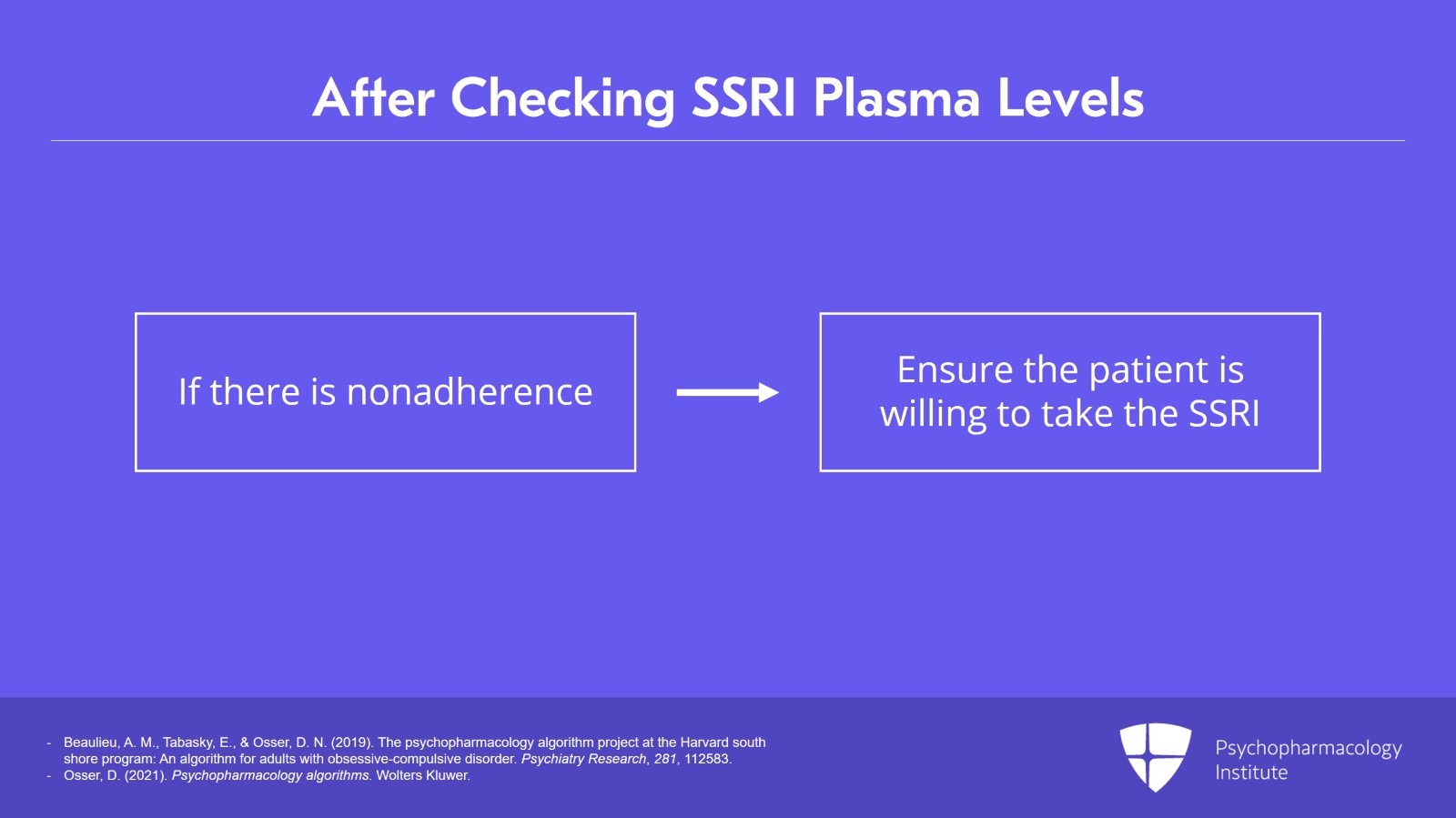
If it turns out to be nonadherence then clearly a discussion with the patient will ensue and either the patient will be now willing to take it or you'll proceed accordingly.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 17
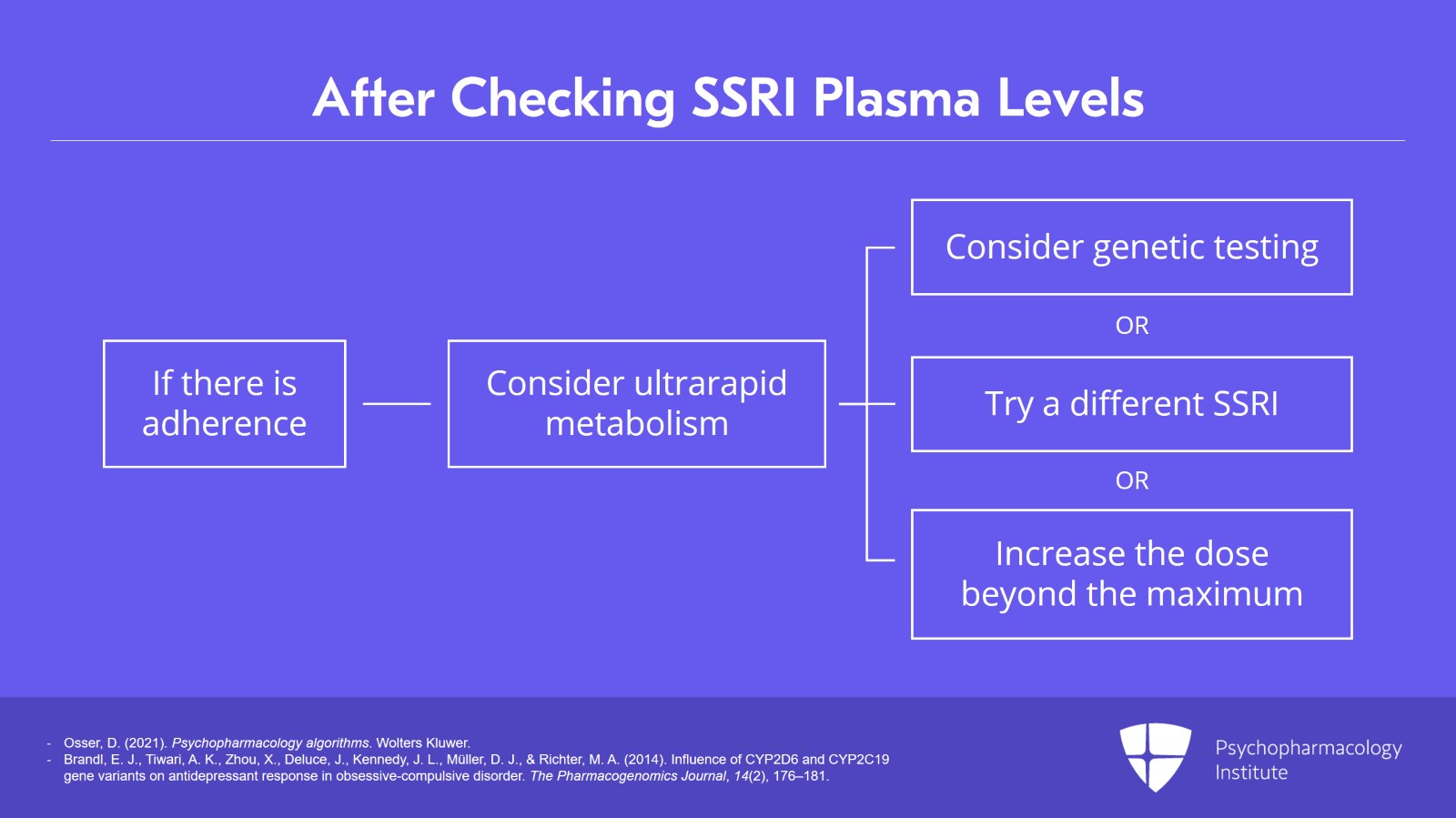
If they insist on strong adherence, then the idea of them being an ultrarapid metabolizer becomes a serious possibility. You may want to get genetic testing to confirm it or you may want to try a different SSRI at that point or possibly increase the one you have going to a much higher dose even beyond the PDR max to see if you can get the level up and overtake the effect of the metabolic process going on.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
- Brandl, E. J., Tiwari, A. K., Zhou, X., Deluce, J., Kennedy, J. L., Müller, D. J., & Richter, M. A. (2014). Influence of CYP2D6 and CYP2C19 gene variants on antidepressant response in obsessive-compulsive disorder. The Pharmacogenomics Journal, 14(2), 176–181.
Slide 14 of 17
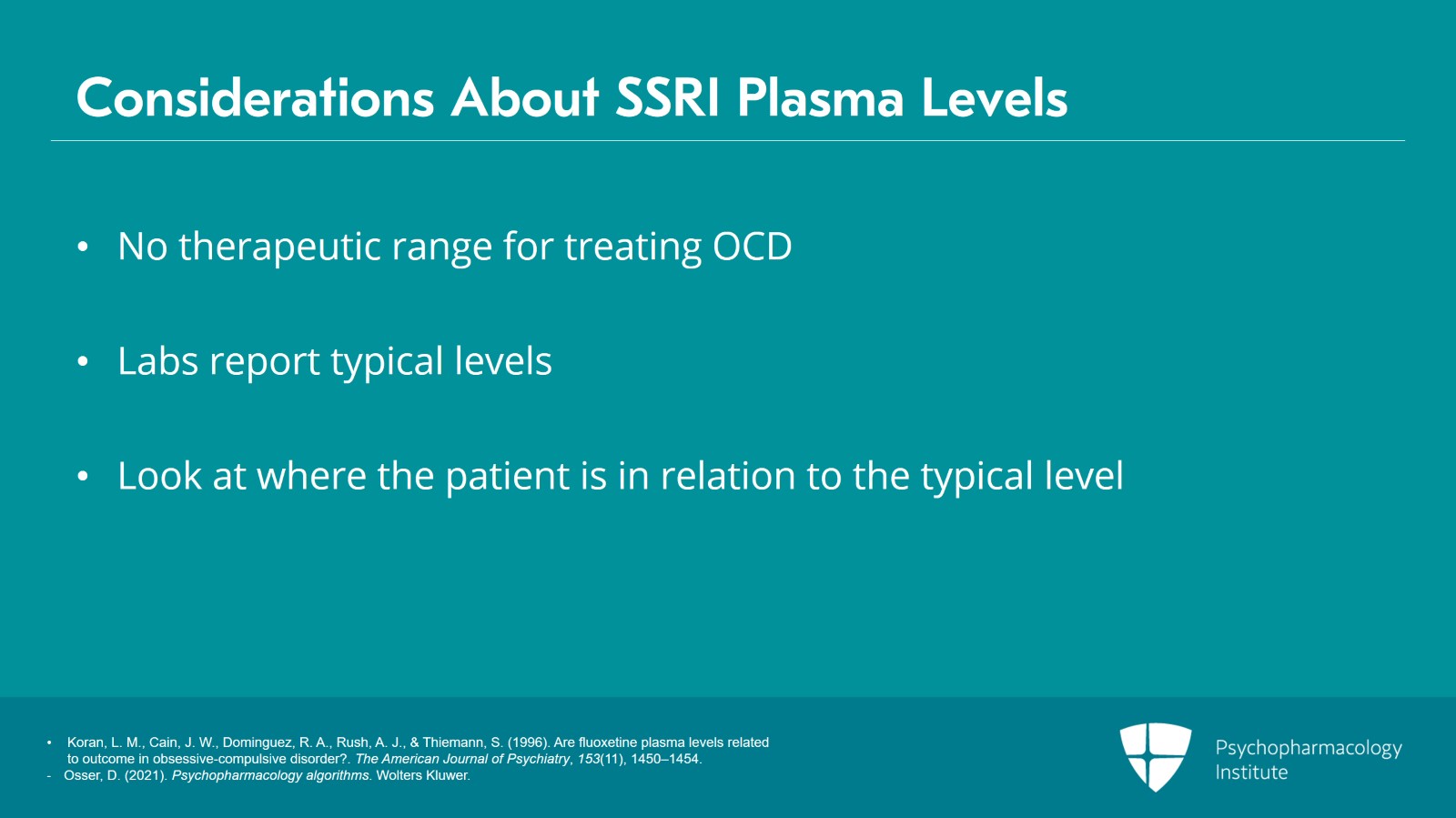
There is no therapeutic range for treating OCD for any of these SSRIs. The level you're going to get from the lab is the typical level seen in people on the particular dose you're using. So the lab will say if you're on a dose of, let's say, 40 of fluoxetine, they get levels ranging from X to Y. So you'll be looking at where the patient is in relation to the typical patient who is getting that quantity of SSRI. And that is useful information and we recommend it.
References:
- Koran, L. M., Cain, J. W., Dominguez, R. A., Rush, A. J., & Thiemann, S. (1996). Are fluoxetine plasma levels related to outcome in obsessive-compulsive disorder?. The American Journal of Psychiatry, 153(11), 1450–1454.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 17
So the key points of this video are that we are looking at the parameters of an adequate trial of an SSRI for OCD and we're recommending that you would first titrate to a standard dose for five to seven weeks. And if the patient is on course for a satisfactory response, you can stay on that dose for maintenance.
Slide 16 of 17
But if it doesn't seem like it's going to be a satisfactory response even with a little more time on the drug, then at this point like seven weeks they've had a partial response you could increase it to the PDR max. If they had no response at all, we're recommending a blood level and a zero level brings up the possibility of poor adherence and zero or low levels also raise the possibility of ultrarapid metabolizer status.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.