Slides and Transcript
Slide 1 of 17
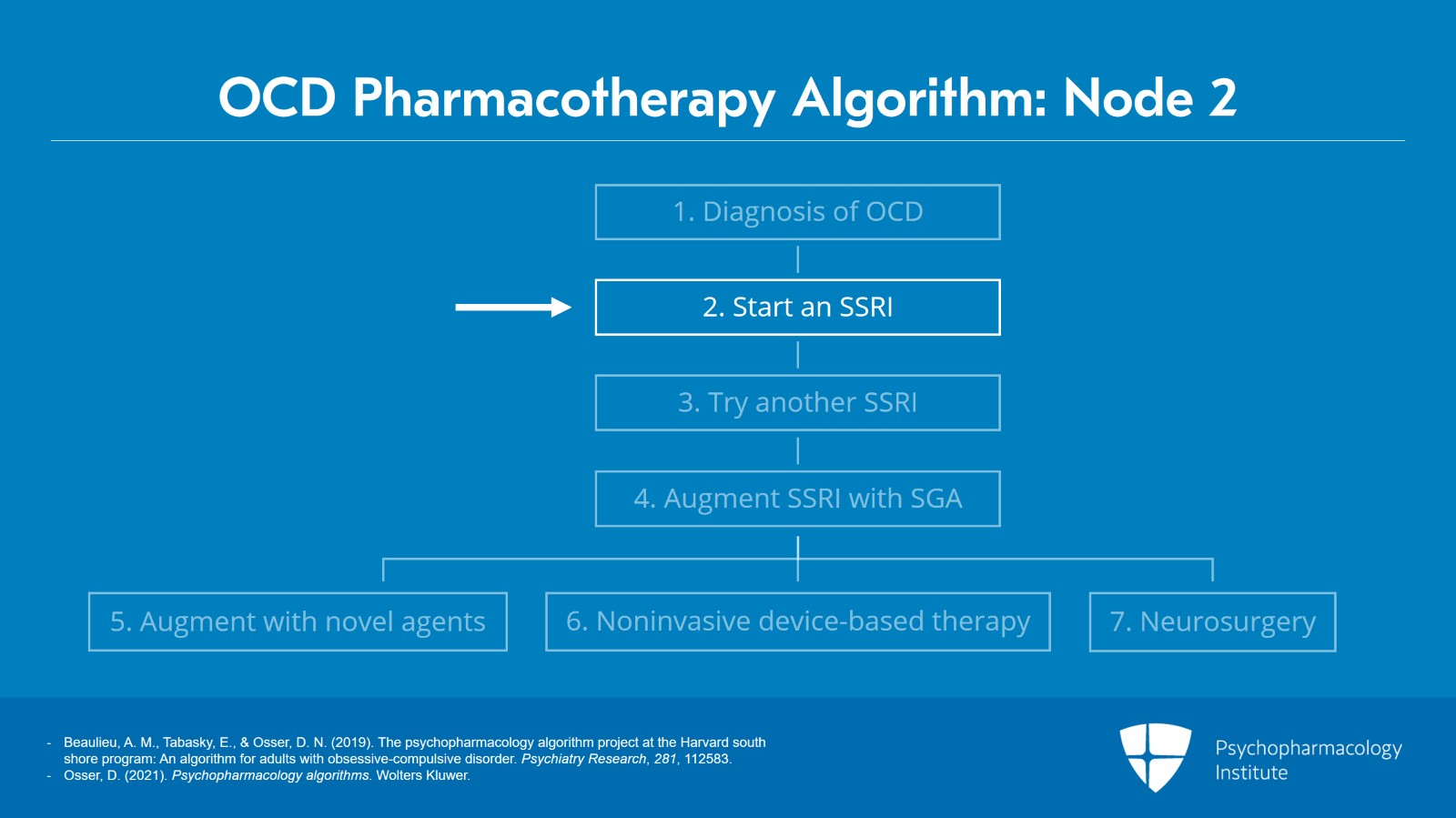
Hi everybody. We are doing video 3 of the psychopharmacology algorithm for OCD. And in this video, we begin talking about the specific recommendations for medication. We are at node 2.
Slide 2 of 17
If you’re following the flowchart and see the little arrow pointing to node 2 and it declares that our first-line recommendation for psychopharmacology of OCD is with an SSRI.
Not a controversial recommendation. It’s pretty much universally recommended in various national and international practice guidelines.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 17
So we start with an SSRI and we gradually titrate to a standard antidepressant dose for 8 to 12 weeks, a standard dose, not a high dose as I will shortly be explaining in detail.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 4 of 17
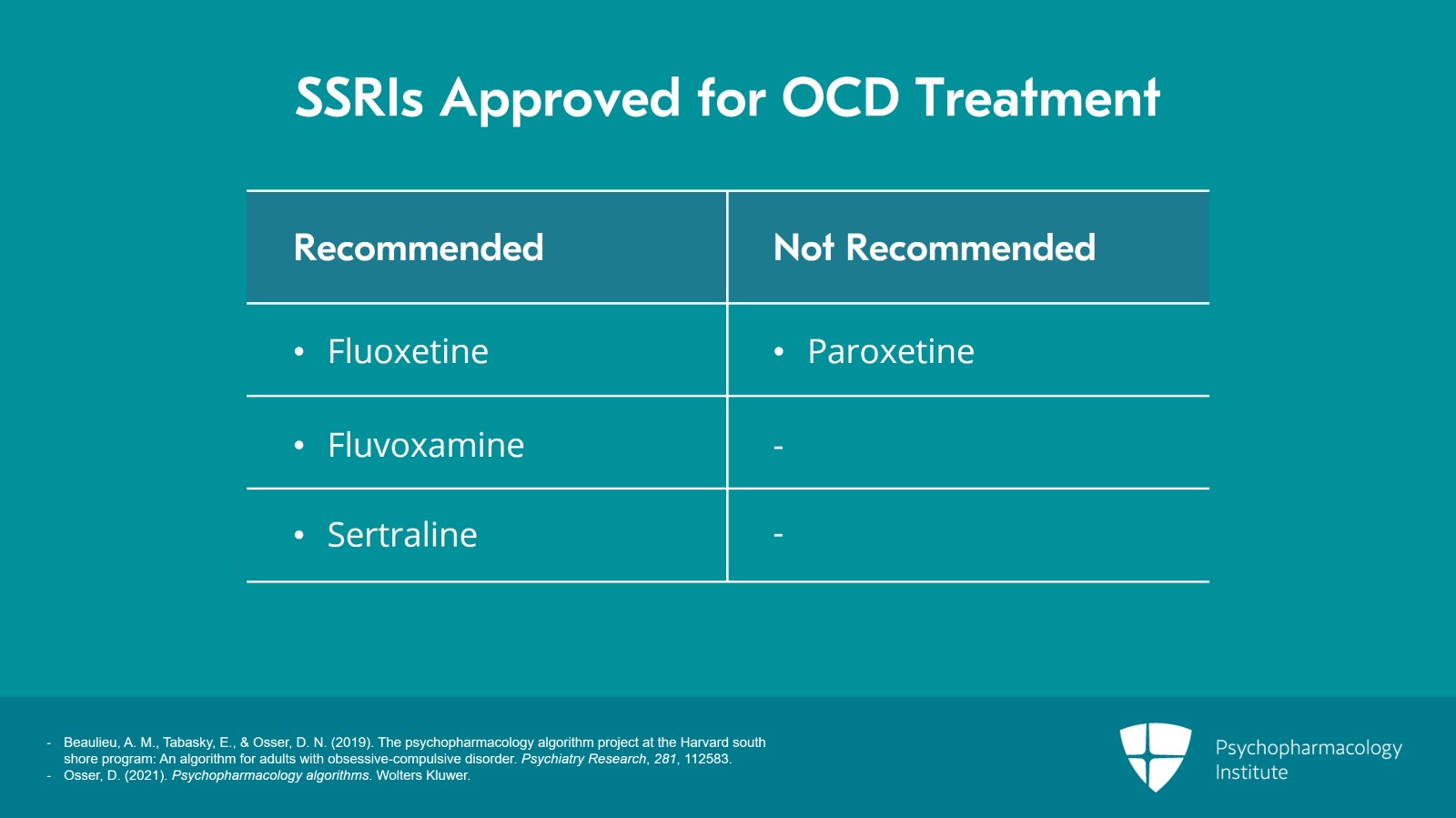
There are four SSRIs that are FDA approved – fluoxetine, fluvoxamine, sertraline, and paroxetine. We recommend three of those, the first three but not paroxetine.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 17
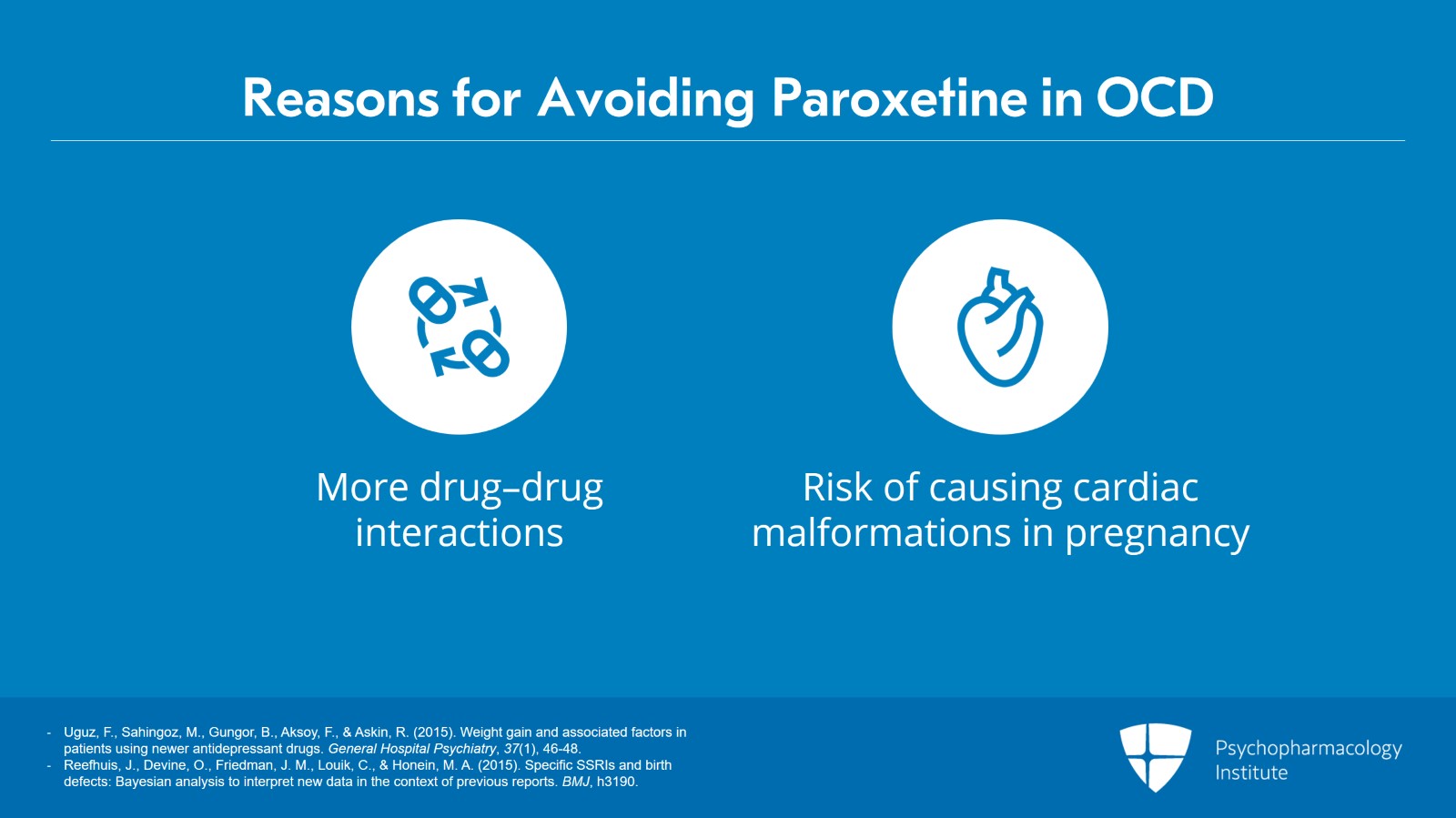
That’s because of its multiple side effects and it’s got the most weight gain, the most constipation. It’s more sedating during the day. It’s got the worst or at the top of the list among the worst sexual side effects.
It’s got the worst discontinuation syndrome problems if you miss a dose or two or stop it.
References:
- Uguz, F., Sahingoz, M., Gungor, B., Aksoy, F., & Askin, R. (2015). Weight gain and associated factors in patients using newer antidepressant drugs. General Hospital Psychiatry, 37(1), 46-48.
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
Slide 6 of 17
It’s got right at the top again of the worst drug-drug interactions.
And as I did discuss in some detail in the previous video, it’s a category D in pregnancy causing cardiac septal malformations. So for all those reasons, we say don’t use it.
References:
- Uguz, F., Sahingoz, M., Gungor, B., Aksoy, F., & Askin, R. (2015). Weight gain and associated factors in patients using newer antidepressant drugs. General Hospital Psychiatry, 37(1), 46-48.
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ, h3190.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 17
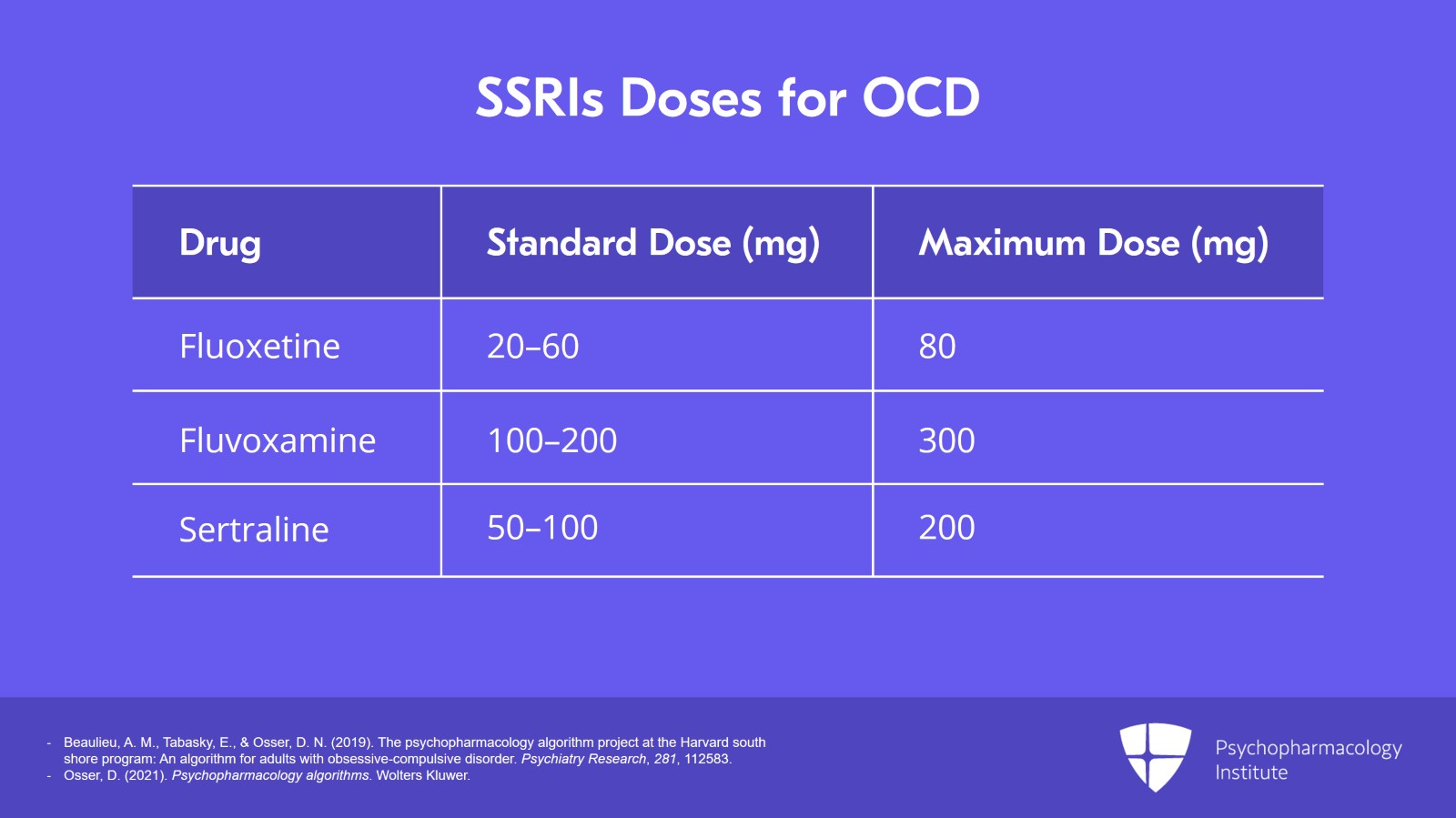
You’ve got three other SSRIs to choose from that all work.
Fluoxetine, the standard dose is 20 to 60 though the PDR max is 80 and I’ll be talking shortly about when you should go up there.
Fluvoxamine has a standard daily dose of 100 to 200 with a maximum of 300.
And sertraline has a usual dose of 50 to 100 with a maximum of 200.
References:
- Beaulieu, A. M., Tabasky, E., & Osser, D. N. (2019). The psychopharmacology algorithm project at the Harvard south shore program: An algorithm for adults with obsessive-compulsive disorder. Psychiatry Research, 281, 112583.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 8 of 17
So we will go into these in some more detail.
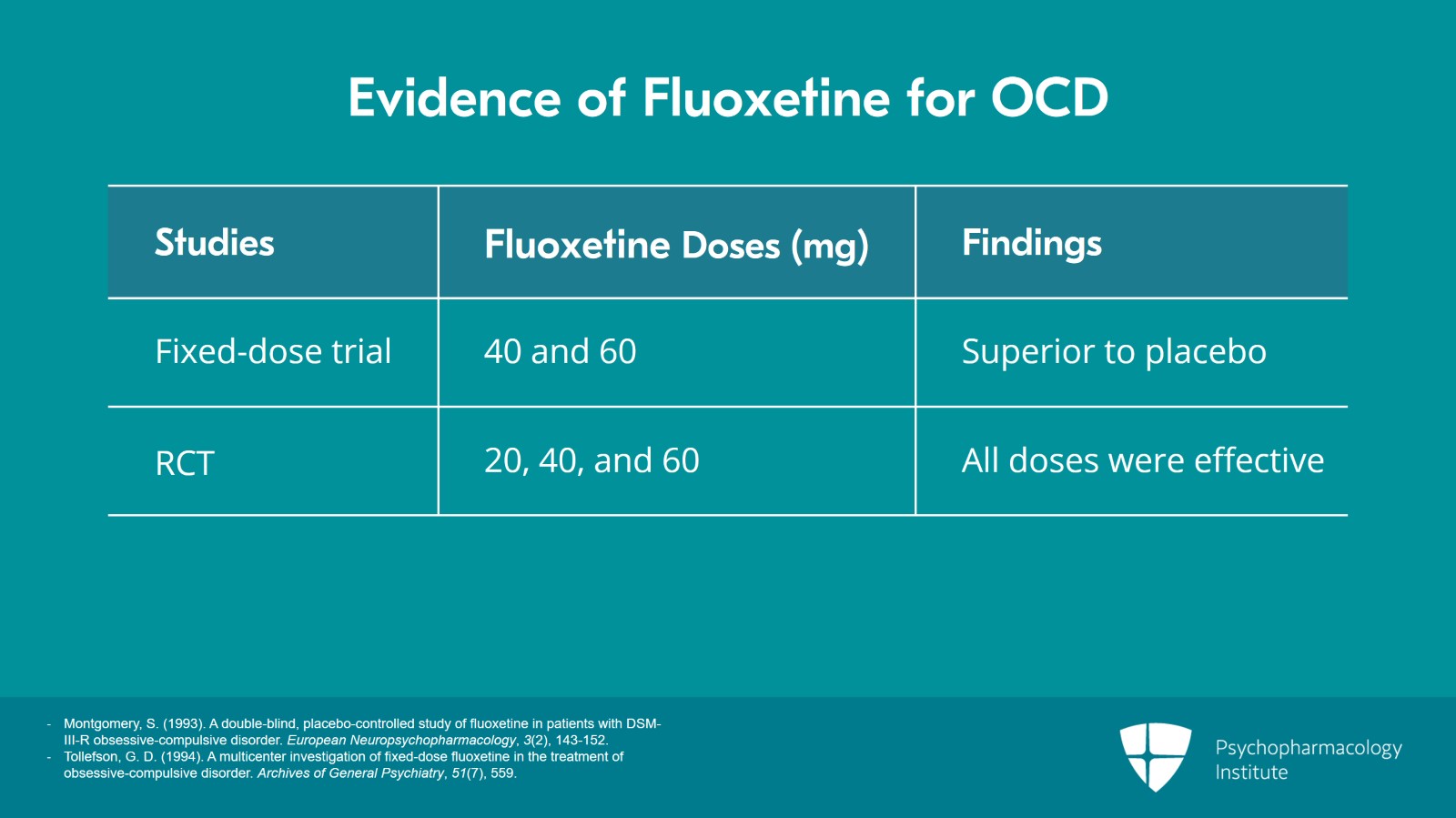
Let’s start with fluoxetine. Fluoxetine is a very reasonable choice.
A fixed dose trial of it found 40 mg and 60 mg superior to placebo.
And a randomized trial comparing three doses – 20, 40, and 60 – were all effective. And I’ll be showing you a little more data on that shortly. So it works.
References:
- Montgomery, S. (1993). A double-blind, placebo-controlled study of fluoxetine in patients with DSM-III-R obsessive-compulsive disorder. European Neuropsychopharmacology, 3(2), 143-152.
- Tollefson, G. D. (1994). A multicenter investigation of fixed-dose fluoxetine in the treatment of obsessive-compulsive disorder. Archives of General Psychiatry, 51(7), 559.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 17
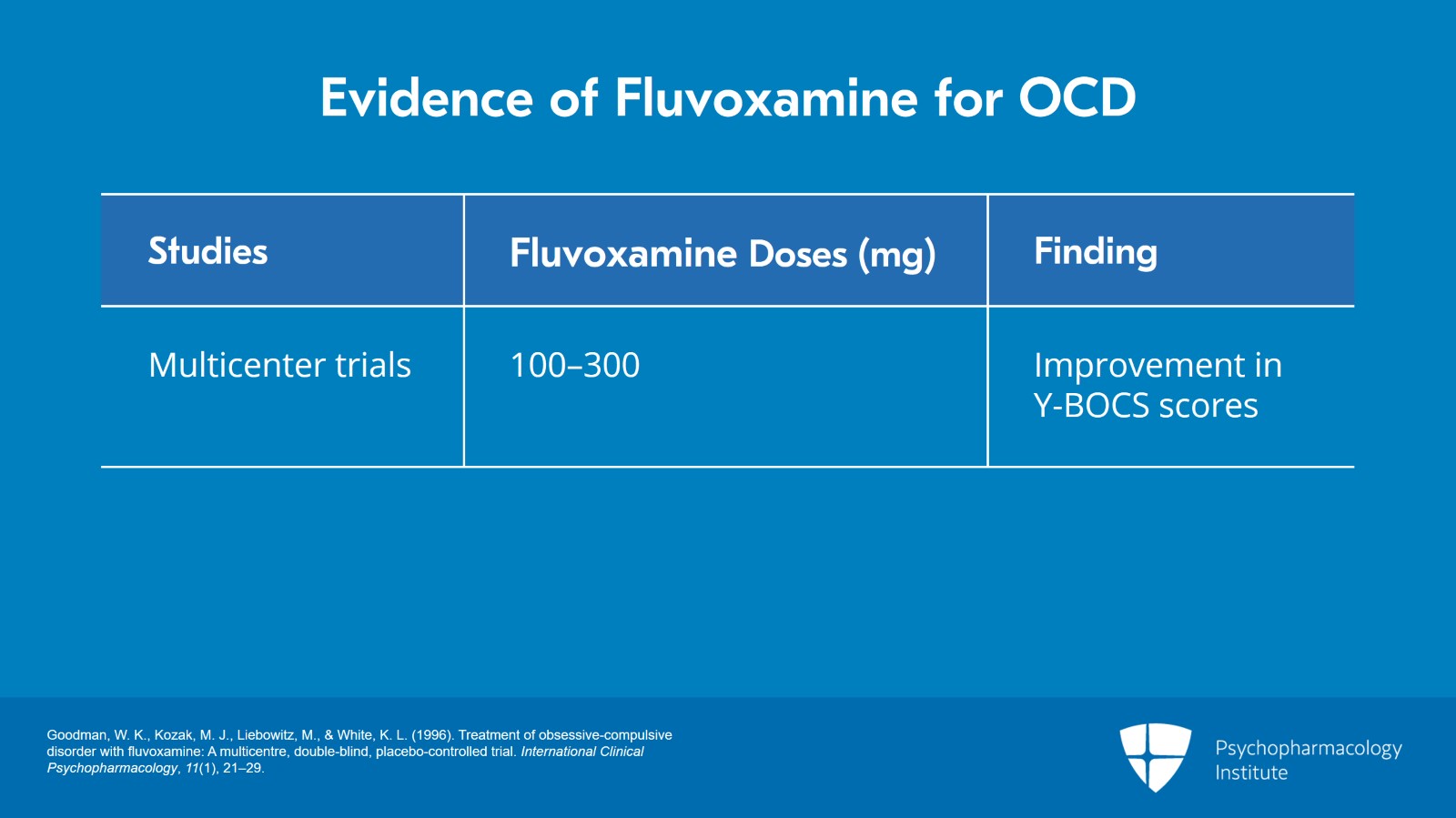
Second option would be fluvoxamine which was actually the first SSRI approved in the United States for OCD though it’s not been shown better than anything else for it but it was the first.
And it had two multicenter trials at that time of 156 and 253 patients. They used a flexible dosing in these studies between 100 and 300. There was good improvement on the Yale-Brown OCD scale, the so-called Y-BOCS.
References:
- Goodman, W. K., Kozak, M. J., Liebowitz, M., & White, K. L. (1996). Treatment of obsessive-compulsive disorder with fluvoxamine: A multicentre, double-blind, placebo-controlled trial. International Clinical Psychopharmacology, 11(1), 21–29.
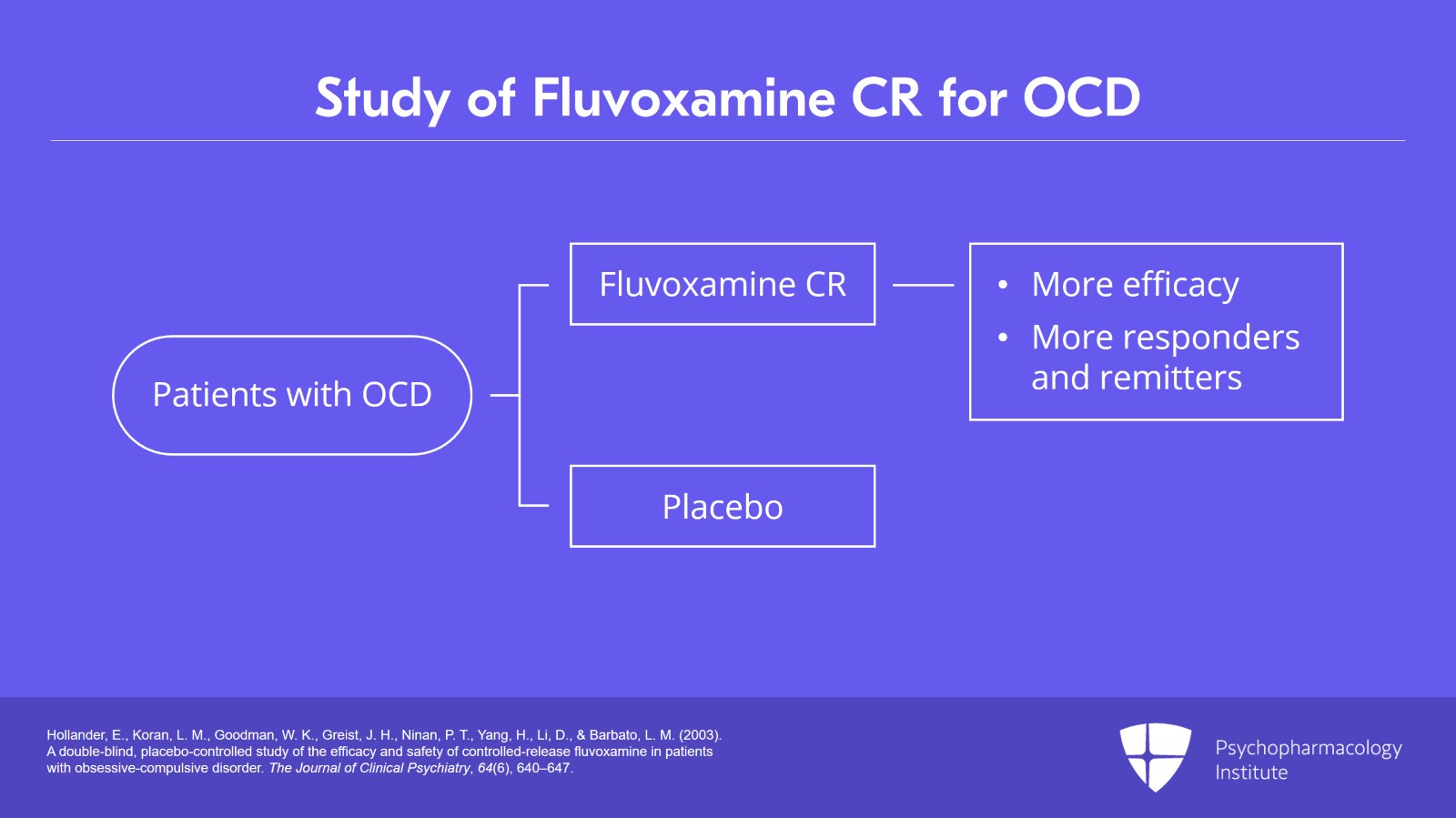
Slide 10 of 17
And there also is a fluvoxamine CR, controlled release, formulation that has been studied and found efficacious compared to placebo.
And also, that same study with the CR version of fluvoxamine found that they were highly more responders and remitters. There were actually more remitters. OCD does not often remit. It improves but it rarely remits. But there were more remitters compared to placebo with fluvoxamine so that’s a good option.
References:
- Hollander, E., Koran, L. M., Goodman, W. K., Greist, J. H., Ninan, P. T., Yang, H., Li, D., & Barbato, L. M. (2003). A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 64(6), 640–647.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
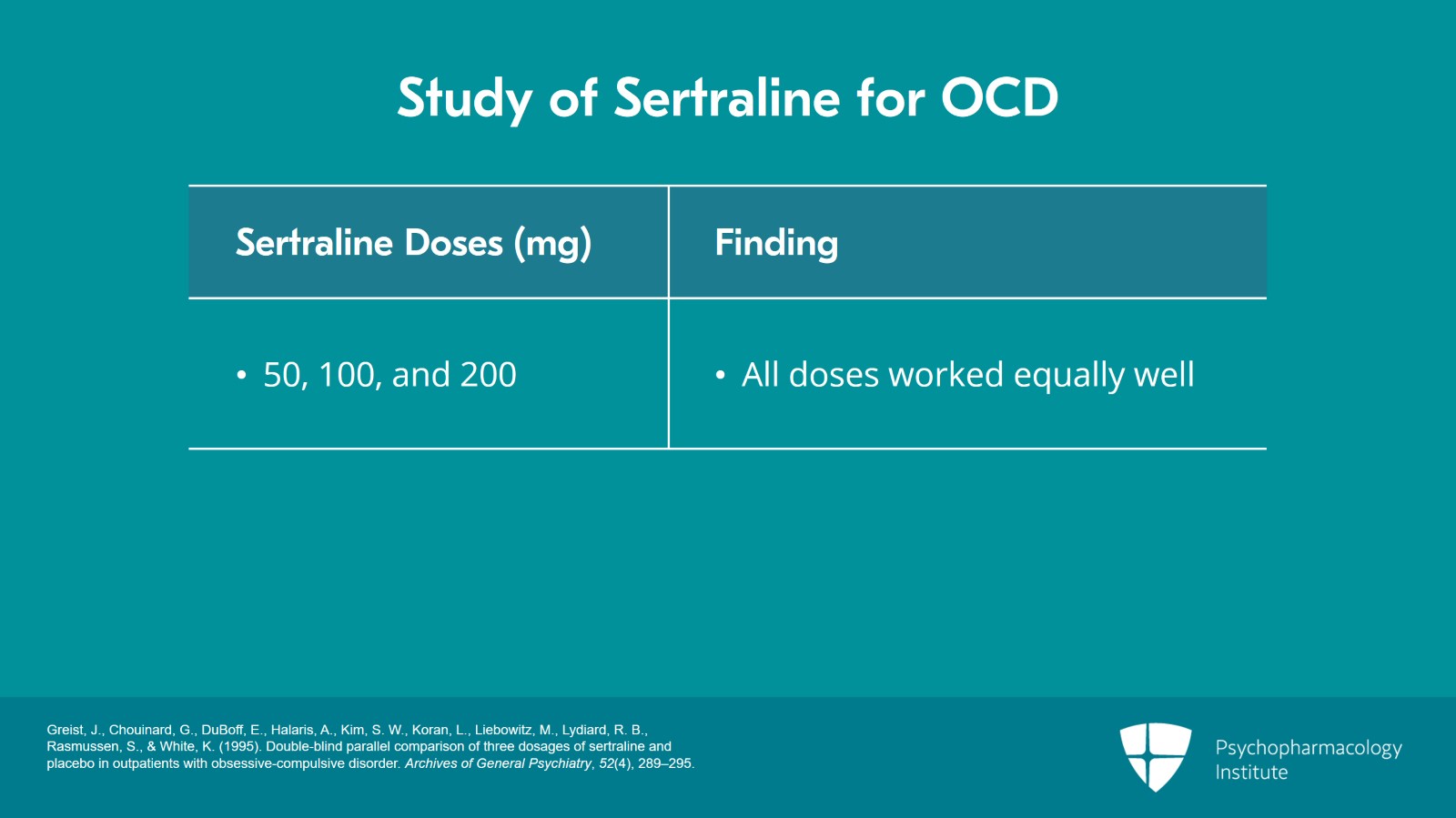
Slide 11 of 17
And the third option is sertraline and it was studied way back in 1995 by Greist and colleagues. They did three doses of 50, 100, and 200. They all worked and all worked equally well actually. There was no difference in the effectiveness of 50, 100, and 200 in that study.
References:
- Greist, J., Chouinard, G., DuBoff, E., Halaris, A., Kim, S. W., Koran, L., Liebowitz, M., Lydiard, R. B., Rasmussen, S., & White, K. (1995). Double-blind parallel comparison of three dosages of sertraline and placebo in outpatients with obsessive-compulsive disorder. Archives of General Psychiatry, 52(4), 289–295.
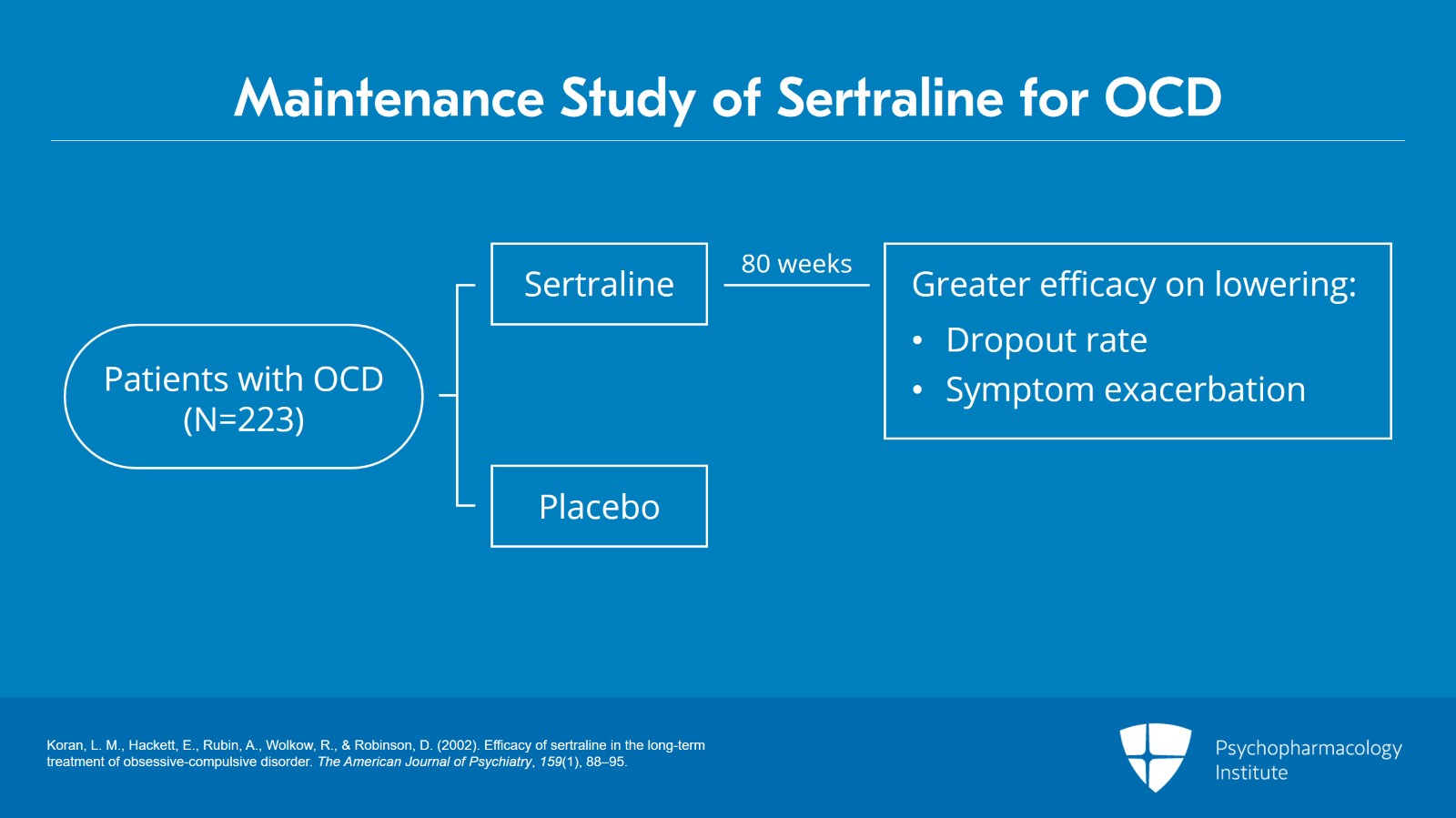
Slide 12 of 17
One more thing to mention is that sertraline has a maintenance study of 80 weeks; 223 patients were studied for that length of time. And it had greater effectiveness than placebo on the dropout rate due to insufficient response.
Also, there was a greater number of exacerbations of symptoms by their criteria in the ones who went off their sertraline, 35%, about 1/3 got worse and 12% got worse if they just stayed on their sertraline.
References:
- Koran, L. M., Hackett, E., Rubin, A., Wolkow, R., & Robinson, D. (2002). Efficacy of sertraline in the long-term treatment of obsessive-compulsive disorder. The American Journal of Psychiatry, 159(1), 88–95.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
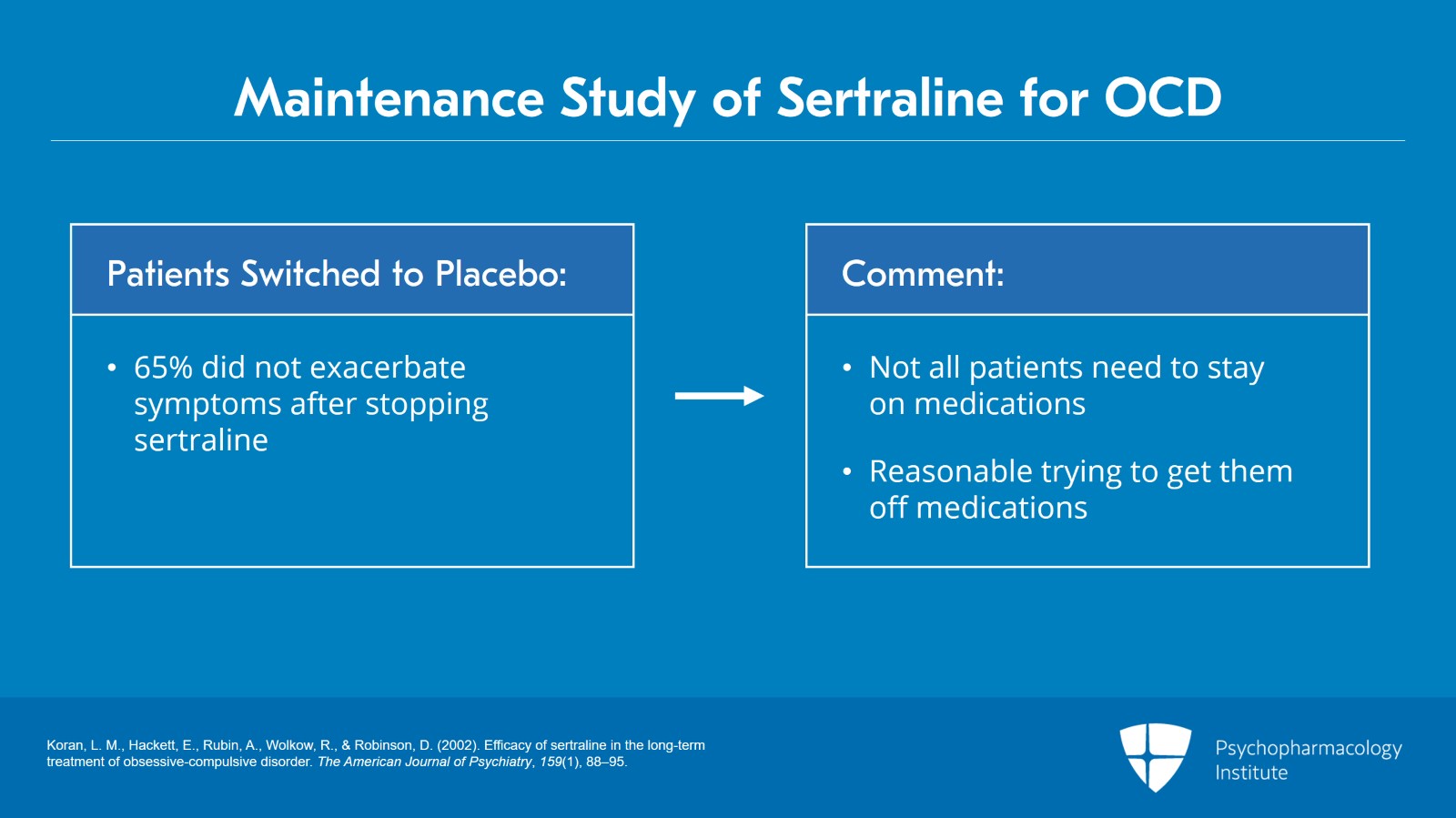
Slide 13 of 17
I like to note though in this kind of maintenance studies when you have 35% getting worse when you switch to placebo it’s worth keeping in mind that means 65% did not exacerbate after stopping their sertraline and going on to placebo. That’s just about 2/3 who didn’t need to keep taking their sertraline.
I think there’s an important message there that not everybody needs to stay on these medications forever and it’s reasonable to try going off them if patients are willing. The side effects can be considerable as we’ll be discussing and they might not need it. Anyway, the quality of life does improve in the group maintained on sertraline compared to those assigned a placebo in this long-term followup study.
References:
- Koran, L. M., Hackett, E., Rubin, A., Wolkow, R., & Robinson, D. (2002). Efficacy of sertraline in the long-term treatment of obsessive-compulsive disorder. The American Journal of Psychiatry, 159(1), 88–95.
Slide 14 of 17
Now, what about citalopram or escitalopram?
We don’t recommend them. They are not FDA approved. They have been found effective in some studies.
However, there are issues with QTc prolongation. As you know, citalopram already had their dosage lowered to a maximum of 40 because of that and we do fairly often have to go to higher doses than 40 and escitalopram causes only moderate QTc prolongation at the approved doses up to 20 but above that though studies have shown that QTc increases become quite significant.
And if you would want to go to high doses which you might need to you’ll have a barrier to doing that due to the QTc issue. So that’s why we would avoid both of those, citalopram and escitalopram.
References:
- Ray, W. A., Chung, C. P., Murray, K. T., Hall, K., & Stein, C. M. (2016). High-dose Citalopram and Escitalopram and the risk of out-of-Hospital death. The Journal of Clinical Psychiatry, 78(02), 190-195.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 17
So to summarize this video, video 3, SSRIs are first line for the pharmacotherapy of OCD in our opinion in concert with most other experts.
Four are FDA approved but we prefer three – sertraline, fluoxetine, and fluvoxamine.
Slide 16 of 17
And not paroxetine because of the much greater side effect burden of paroxetine compared to the other SSRIs.
We do not recommend citalopram and escitalopram because of risks of QTc prolongation if you should want to go to high doses which you might need to.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.