Slides and Transcript
Slide 2 of 13
So anorexia nervosa. This is one of the most lethal, if not the most lethal psychiatric condition in our nomenclature. Some people now say that opiate addiction is rivaling it but suffice to say that there is an enormously high morbidity and mortality associated with anorexia nervosa. There is a new description of it in DSM-5. The word refusal has been taken out and this is largely due to the implication that that’s blaming people for not eating or gaining weight…
References:
- American Psychiatric Association. (2013). Feeding and eating disorders. In Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 13
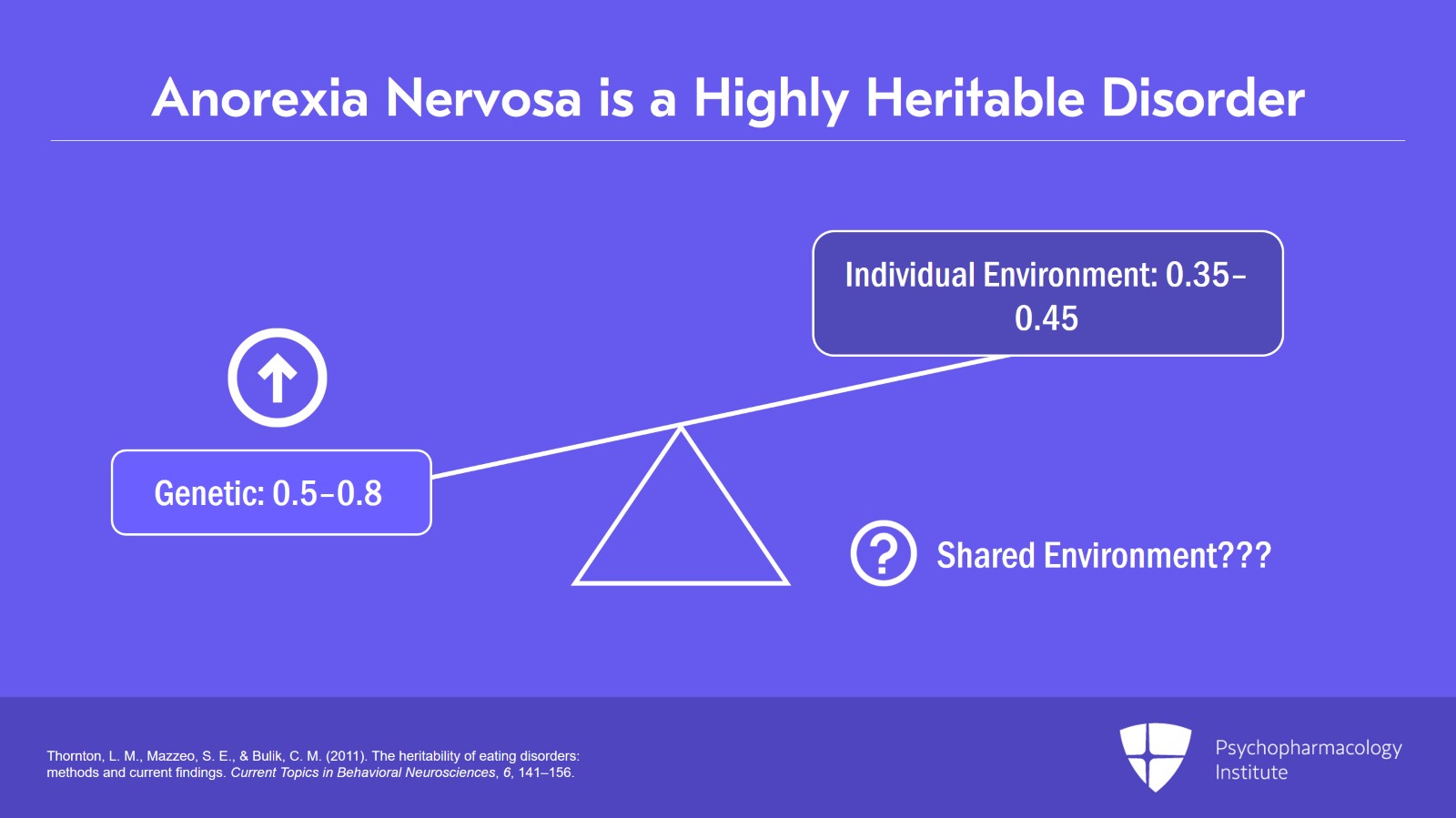
… Anorexia nervosa is a highly heritable disorder with heritability rates on the order of 0.5 to 0.8. So most of the variance is accounted for by additive genetic effects which is contrary to popular belief in society, in our culture. Sociocultural effects are not the primary cause in multiple twin studies.
The other major source of the variance is largely individual or unique environmental factors which account for 0.35 to 0.45 of the variance. That’s where trauma and adverse experiences during development come into play and which interact with genetic factors. Whereas, the shared environmental piece hardly accounts for any of the variance whatsoever. That’s a big surprise to many people who attribute anorexia nervosa to primarily sociocultural factors. If that were the case, we would have a much higher prevalence of anorexia nervosa.
References:
- Thornton, L. M., Mazzeo, S. E., & Bulik, C. M. (2011). The heritability of eating disorders: methods and current findings. Current Topics in Behavioral Neurosciences, 6, 141–156.
Slide 4 of 13
First and foremost, anorexia nervosa involves a restriction of energy intake relative to requirements leading to significantly low body weight in the context of age, developmental trajectory and physical health.
Significantly low weight is purposely more arbitrary but it’s defined as weight that is less than minimally normal and for children and adolescents, less than minimally expected.
What is really important in diagnosing anorexia nervosa is to see the individual’s childhood growth charts. It may take a little work tracking that information down particularly if people have moved various places and seen a number of doctors. But contacting pediatricians and/or family doctors to piece together the trajectory of where they were at birth and how they progressed in terms of their growth and development is really key to understanding what is “normal” for any given individual.
References:
- American Psychiatric Association. (2013). Feeding and eating disorders. In Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 13
There are specifiers whether one is in partial remission or full remission. I will say that it does take some time for people to get into true remission and initially involves normalization of weight or what is called nutritional rehabilitation. And the treatment typically involves adjunctive treatment by a dietitian who is versed in eating disorders.
References:
- American Psychiatric Association. (2013). Feeding and eating disorders. In Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Slide 6 of 13
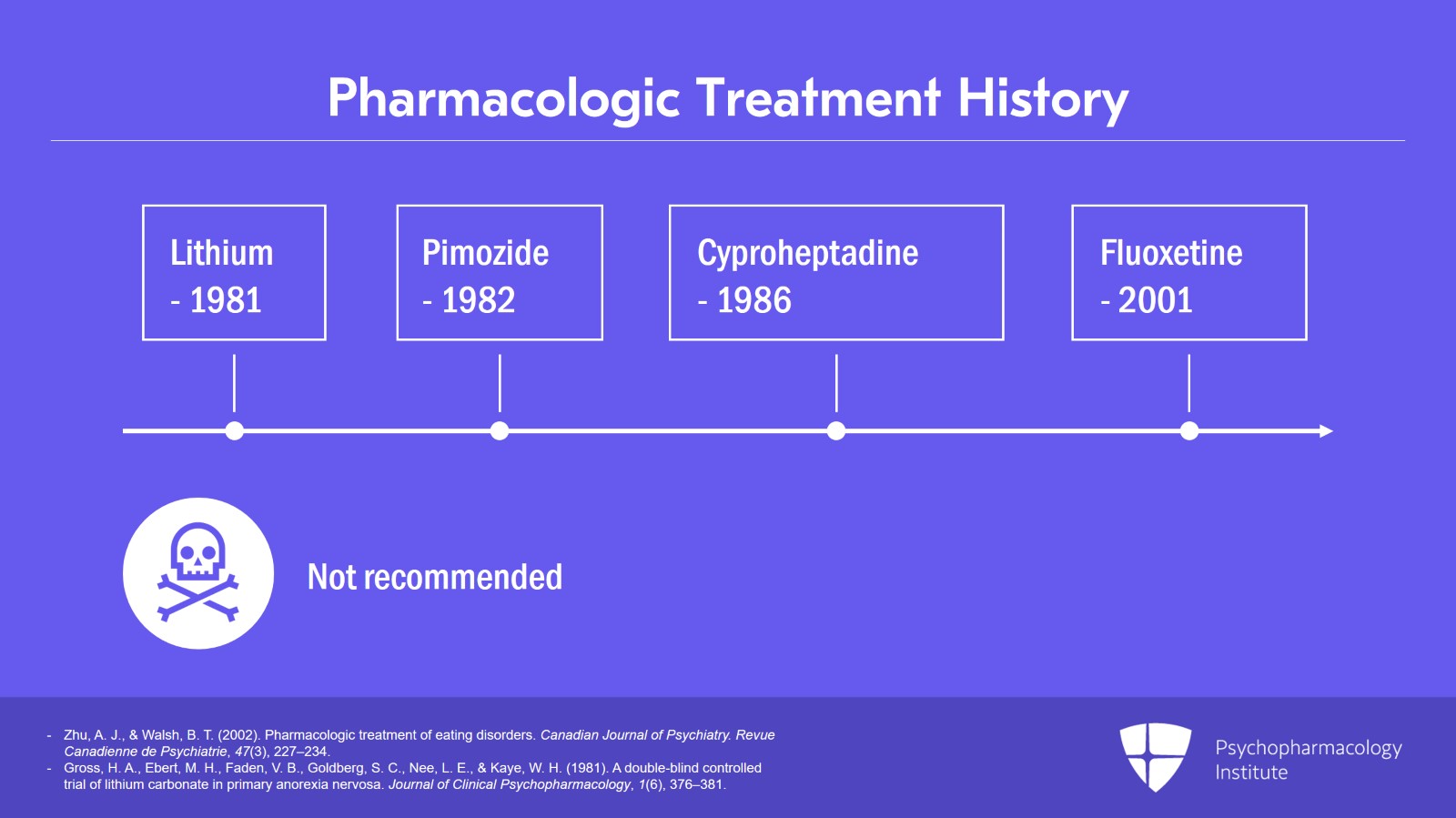
In the next slide, this is an overview of the pharmacological treatment history of anorexia nervosa going back several decades. There was one early study that showed lithium was effective. It was effective statistically but no one uses it now clinically and I’m not recommending it as this can be highly lethal, particularly in people who are starving or not drinking enough fluids as well as in the binge-purge type of anorexia nervosa. That’s a setup for lithium toxicity.
References:
- Zhu, A. J., & Walsh, B. T. (2002). Pharmacologic treatment of eating disorders. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 47(3), 227–234.
- Gross, H. A., Ebert, M. H., Faden, V. B., Goldberg, S. C., Nee, L. E., & Kaye, W. H. (1981). A double-blind controlled trial of lithium carbonate in primary anorexia nervosa. Journal of Clinical Psychopharmacology, 1(6), 376–381.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 13
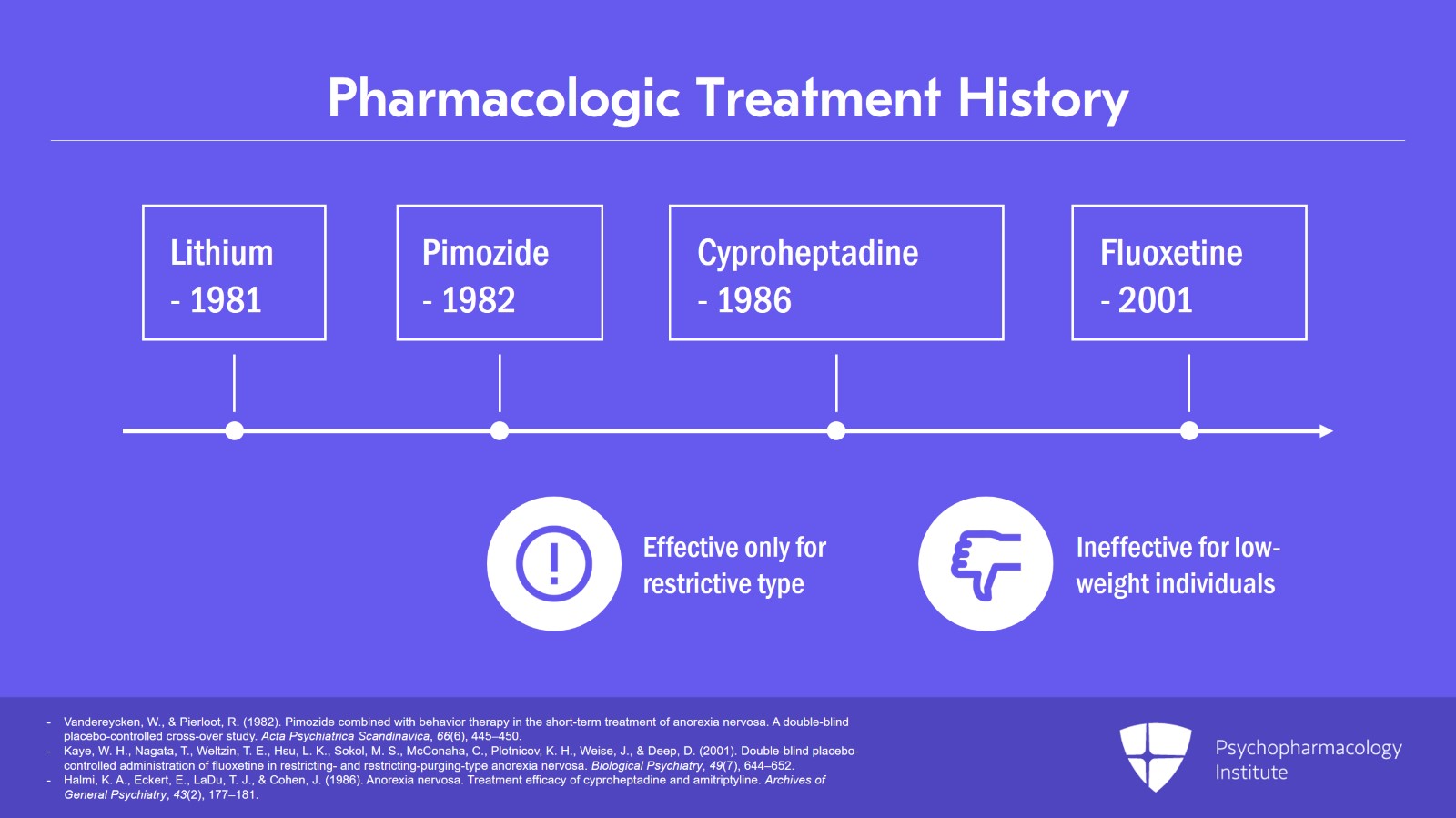
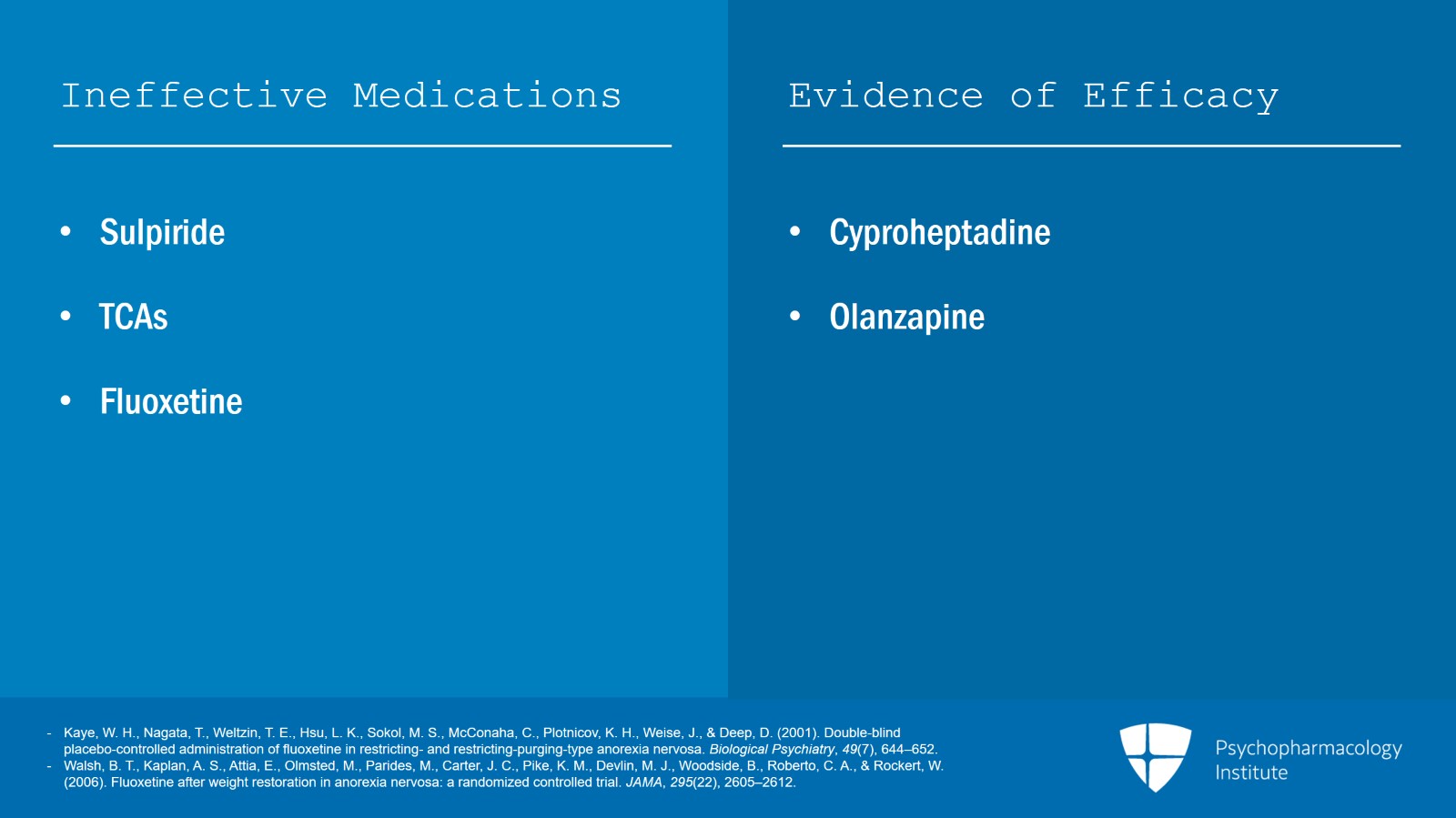
Pimozide, fluoxetine. And many people are surprised to learn that fluoxetine in low-weight individuals is absolutely ineffective.
It was shown in this one study which I’m going to show you to be helpful in terms of preventing relapse in weight-restored individuals with anorexia nervosa. Cyproheptadine is one older drug studied back in the 1980s that worked only in the restricting type of anorexia nervosa. But olanzapine is really the major medication with an incomparable evidence base.
References:
- Vandereycken, W., & Pierloot, R. (1982). Pimozide combined with behavior therapy in the short-term treatment of anorexia nervosa. A double-blind placebo-controlled cross-over study. Acta Psychiatrica Scandinavica, 66(6), 445–450.
- Kaye, W. H., Nagata, T., Weltzin, T. E., Hsu, L. K., Sokol, M. S., McConaha, C., Plotnicov, K. H., Weise, J., & Deep, D. (2001). Double-blind placebo-controlled administration of fluoxetine in restricting- and restricting-purging-type anorexia nervosa. Biological Psychiatry, 49(7), 644–652.
- Halmi, K. A., Eckert, E., LaDu, T. J., & Cohen, J. (1986). Anorexia nervosa. Treatment efficacy of cyproheptadine and amitriptyline. Archives of General Psychiatry, 43(2), 177–181.
Slide 8 of 13
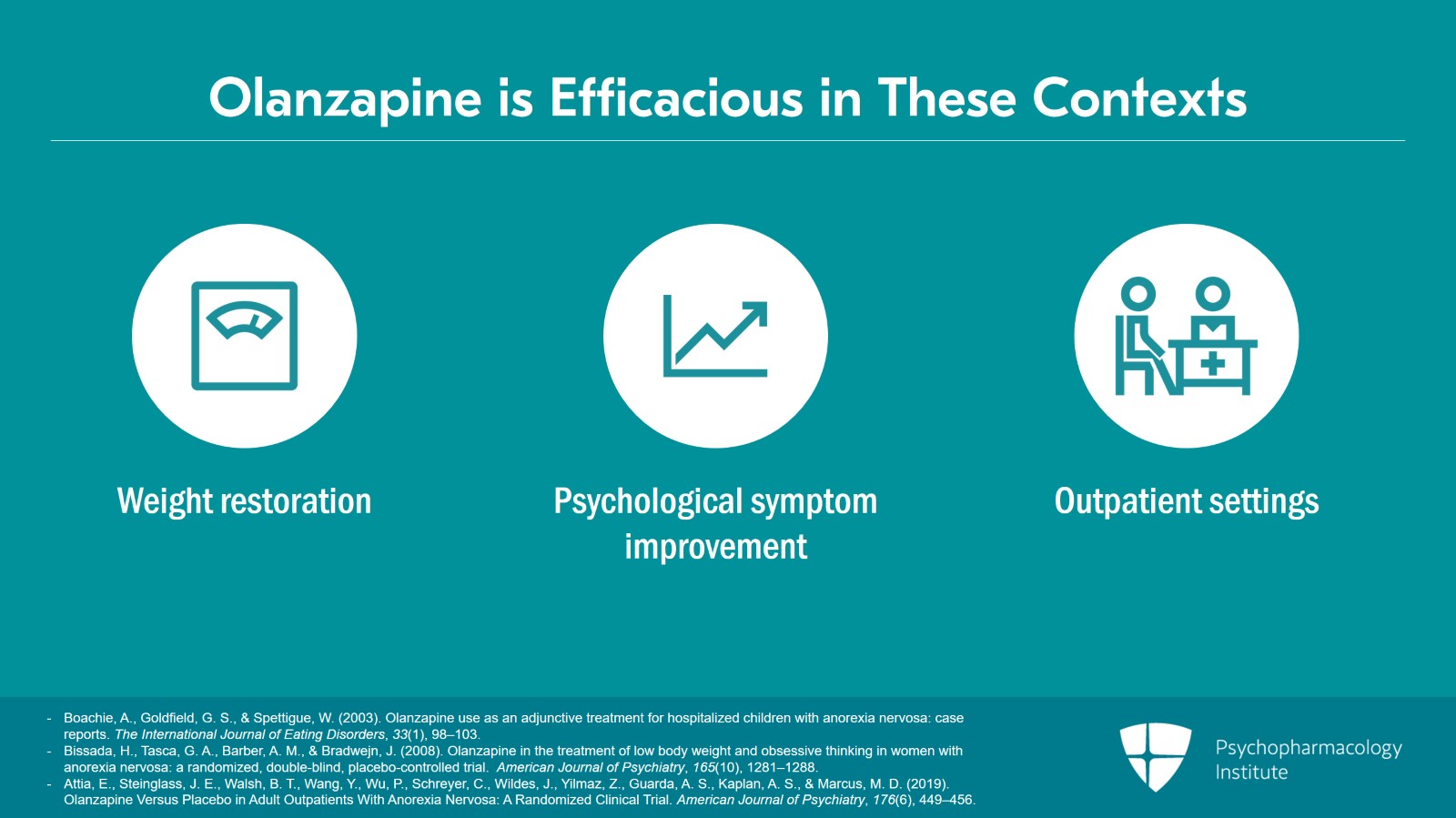
There are six randomized controlled trials that demonstrate the efficacy of olanzapine either for weight restoration or psychological symptom improvement. Some trials show olanzapine and aripiprazole to be ineffective but these have been in inpatient or residential settings where you’ve got a full court press so to speak. You’ve got meal therapy six times a day. You’ve got constant nursing staff. You have psychotherapy groups going on all day and individual therapy and family therapy and so forth. And so in that context where you have a full court press, you don’t see an advantage of olanzapine. You see it in outpatient studies where you don’t have that kind of intensity of therapy.
References:
- Boachie, A., Goldfield, G. S., & Spettigue, W. (2003). Olanzapine use as an adjunctive treatment for hospitalized children with anorexia nervosa: case reports. The International Journal of Eating Disorders, 33(1), 98–103.
- Bissada, H., Tasca, G. A., Barber, A. M., & Bradwejn, J. (2008). Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. American Journal of Psychiatry, 165(10), 1281–1288.
- Attia, E., Steinglass, J. E., Walsh, B. T., Wang, Y., Wu, P., Schreyer, C., Wildes, J., Yilmaz, Z., Guarda, A. S., Kaplan, A. S., & Marcus, M. D. (2019). Olanzapine Versus Placebo in Adult Outpatients With Anorexia Nervosa: A Randomized Clinical Trial. American Journal of Psychiatry, 176(6), 449–456.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 13
Several studies have shown medications to be ineffective such as sulpiride, tricyclic antidepressants. And then a big surprise to a lot of you, fluoxetine does not work in non-weight-restored patients. And then in another study, restored patients who are also getting cognitive behavioral therapy focused on relapse prevention, it was no better than CBT alone. In the same study that I mentioned earlier, cyproheptadine was only helpful at least statistically but not so much clinically in anorexia nervosa restricting type of patients. And before the advent of olanzapine, a lot of pediatricians and child psychiatrists would use cyproheptadine to treat anorexia nervosa.
References:
- Kaye, W. H., Nagata, T., Weltzin, T. E., Hsu, L. K., Sokol, M. S., McConaha, C., Plotnicov, K. H., Weise, J., & Deep, D. (2001). Double-blind placebo-controlled administration of fluoxetine in restricting- and restricting-purging-type anorexia nervosa. Biological Psychiatry, 49(7), 644–652.
- Walsh, B. T., Kaplan, A. S., Attia, E., Olmsted, M., Parides, M., Carter, J. C., Pike, K. M., Devlin, M. J., Woodside, B., Roberto, C. A., & Rockert, W. (2006). Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. JAMA, 295(22), 2605–2612.
Slide 10 of 13
Zinc is something that can be depleted in the face of semi-starvation which can add to the decrease in appetite….
References:
- Humphries, L., Vivian, B., Stuart, M., & McClain, C. J. (1989). Zinc deficiency and eating disorders. The Journal of Clinical Psychiatry, 50(12), 456–459.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 13
…But anorexia nervosa is really a misnomer. It does not technically involve a loss of appetite. It’s the anxiety, the obsessionality and compulsivity that override the drive to eat. Patients will tell you that they are hungry but too afraid to eat.
References:
- Steiger H. (2004). Eating disorders and the serotonin connection: state, trait and developmental effects. Journal of Psychiatry & Neuroscience : JPN, 29(1), 20–29.
Slide 12 of 13
The key points of this video include: Many medicines have been studied in anorexia nervosa but olanzapine is the only agent that has shown any consistent clinical effect in multiple controlled trials. Pharmacotherapy for anorexia nervosa should be adjunctive to multimodal therapies.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.