Slides and Transcript
Slide 1 of 12
Next, we’re going to talk about mood stabilizers for patients with borderline personality disorder.
Slide 2 of 12
We’ll talk a little bit about lamotrigine which is particularly interesting. Some of the earlier randomized controlled trials of lamotrigine suggested they may have a role for affective instability as a primary outcome.
References:
- Reich, D. B., Zanarini, M. C., & Bieri, K. A. (2009). A preliminary study of lamotrigine in the treatment of affective instability in borderline personality disorder. International Clinical Psychopharmacology, 1.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 12
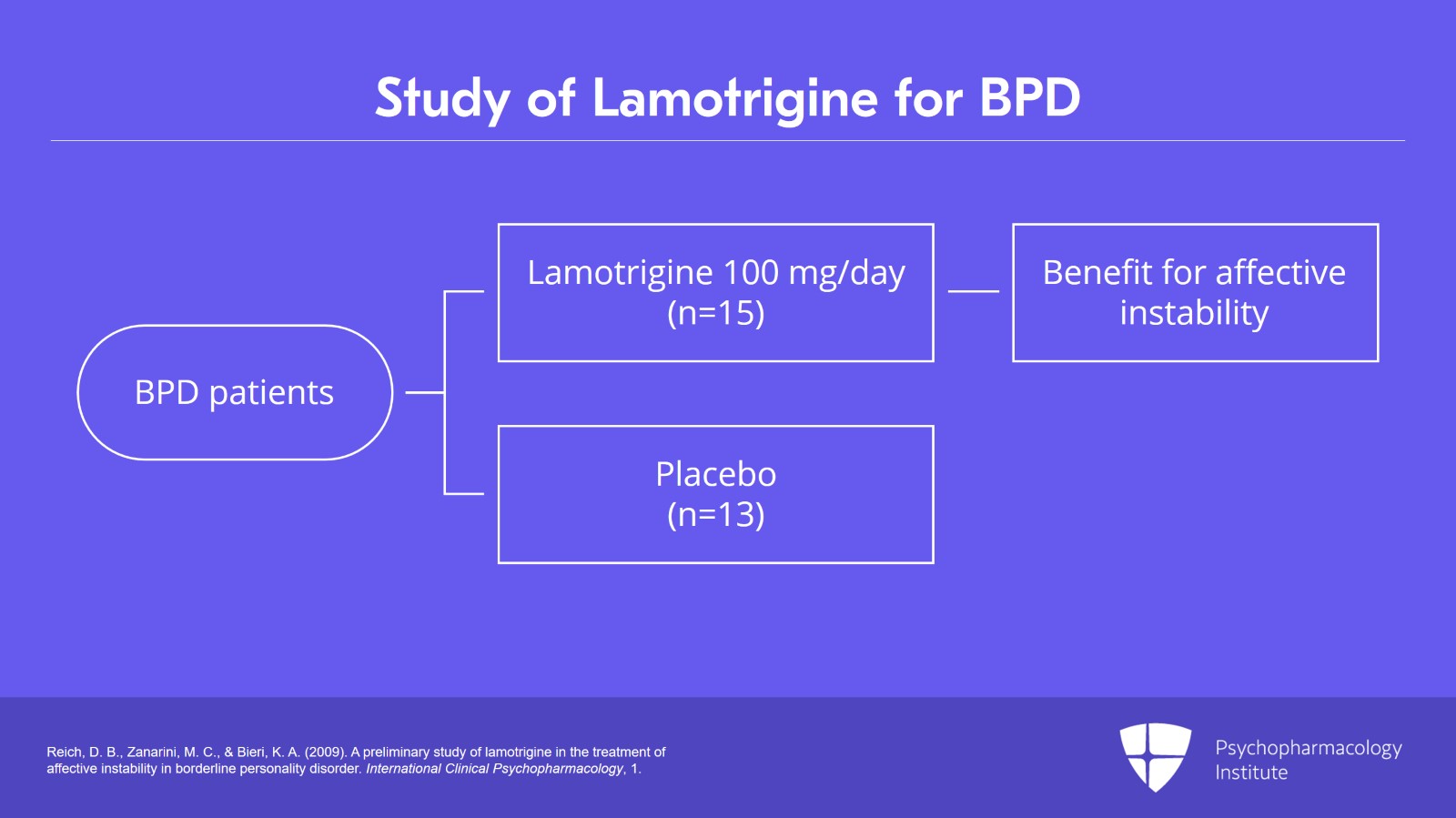
This was a small study for borderline personality disorder of 15 patients in the lamotrigine arm, 13 patients in the placebo arm and the dose was around 100 mg a day. So certainly, the trial has limitations but it did show benefit for lamotrigine for affective instability.
References:
- Reich, D. B., Zanarini, M. C., & Bieri, K. A. (2009). A preliminary study of lamotrigine in the treatment of affective instability in borderline personality disorder. International Clinical Psychopharmacology, 1.
Slide 4 of 12
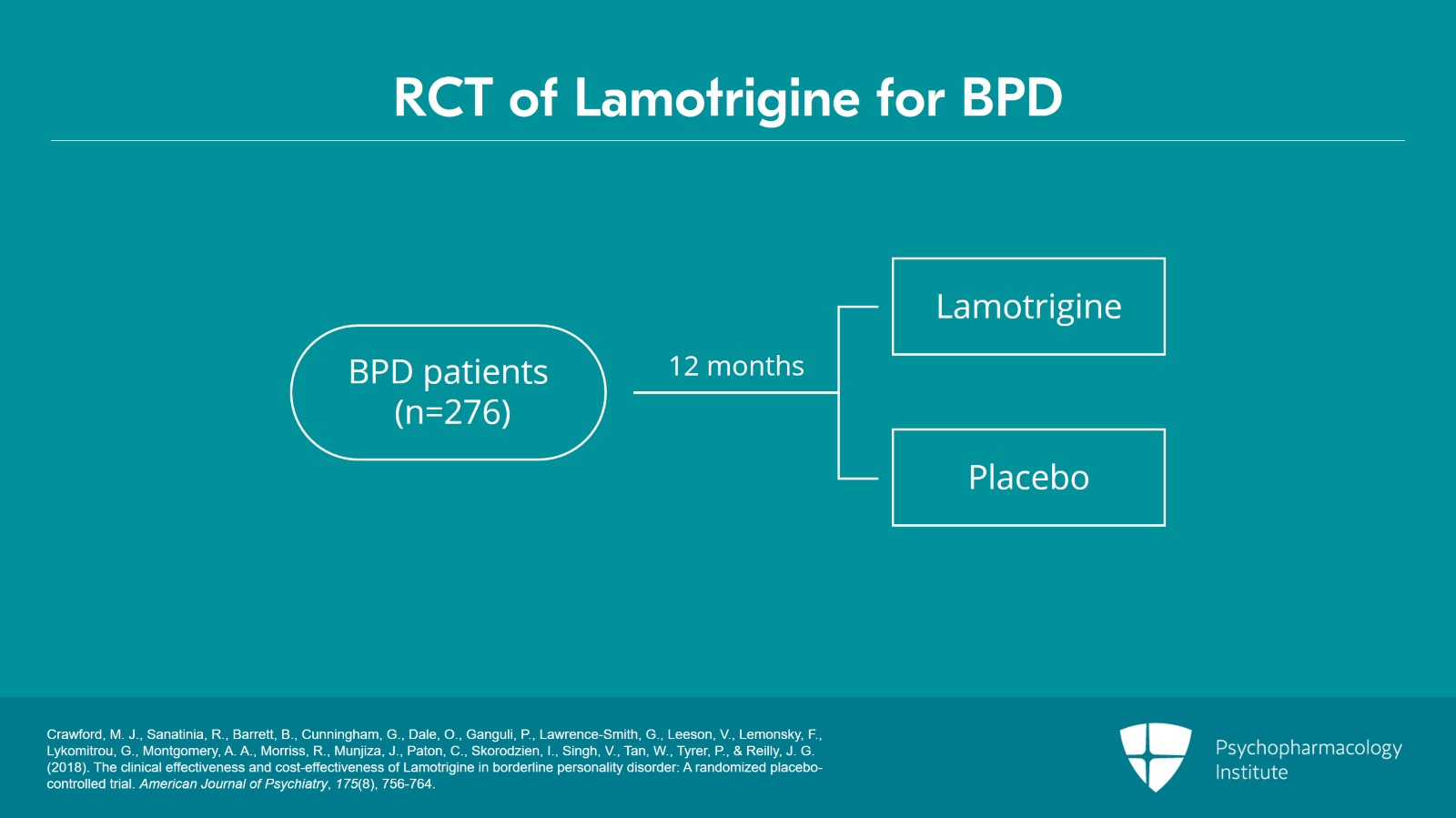
And it was on that basis that Crawford and colleagues in the UK undertook probably the best pharmacologic study in patients with borderline personality disorder.
And this was a randomized controlled trial of lamotrigine versus placebo that followed these patients for 12 months. The sample was made up of 276 patients although they did lose a number of patients during the 12-month follow-up. They compared lamotrigine versus placebo but all the patients were receiving care sort of in a mental health specialty clinic.
References:
- Crawford, M. J., Sanatinia, R., Barrett, B., Cunningham, G., Dale, O., Ganguli, P., Lawrence-Smith, G., Leeson, V., Lemonsky, F., Lykomitrou, G., Montgomery, A. A., Morriss, R., Munjiza, J., Paton, C., Skorodzien, I., Singh, V., Tan, W., Tyrer, P., & Reilly, J. G. (2018). The clinical effectiveness and cost-effectiveness of Lamotrigine in borderline personality disorder: A randomized placebo-controlled trial. American Journal of Psychiatry, 175(8), 756-764.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
The primary outcome was borderline symptoms, but they had a breadth of secondary outcomes including depression, self-harm, substance use, social functioning, and quality of life including a cost effectiveness analysis.
References:
- Crawford, M. J., Sanatinia, R., Barrett, B., Cunningham, G., Dale, O., Ganguli, P., Lawrence-Smith, G., Leeson, V., Lemonsky, F., Lykomitrou, G., Montgomery, A. A., Morriss, R., Munjiza, J., Paton, C., Skorodzien, I., Singh, V., Tan, W., Tyrer, P., & Reilly, J. G. (2018). The clinical effectiveness and cost-effectiveness of Lamotrigine in borderline personality disorder: A randomized placebo-controlled trial. American Journal of Psychiatry, 175(8), 756-764.
Slide 6 of 12
Now, this study is important because it demonstrated that there were no differences between lamotrigine and placebo on the borderline outcomes or any of the secondary outcomes. There was no advantage to lamotrigine in terms of quality of life or costing. And so, the authors concluded that we could not recommend lamotrigine for borderline patients based on this carefully conceived study.
References:
- Crawford, M. J., Sanatinia, R., Barrett, B., Cunningham, G., Dale, O., Ganguli, P., Lawrence-Smith, G., Leeson, V., Lemonsky, F., Lykomitrou, G., Montgomery, A. A., Morriss, R., Munjiza, J., Paton, C., Skorodzien, I., Singh, V., Tan, W., Tyrer, P., & Reilly, J. G. (2018). The clinical effectiveness and cost-effectiveness of Lamotrigine in borderline personality disorder: A randomized placebo-controlled trial. American Journal of Psychiatry, 175(8), 756-764.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
Well, just a couple of comments on the Crawford study that I think are important takeaways.
The challenge of the study is that they used a rather limited measure of affective instability and so I think you can question whether it’s a valid outcome measure. Were they really capturing affective instability with the measure they used?
References:
- Crawford, M. J., Sanatinia, R., Barrett, B., Cunningham, G., Dale, O., Ganguli, P., Lawrence-Smith, G., Leeson, V., Lemonsky, F., Lykomitrou, G., Montgomery, A. A., Morriss, R., Munjiza, J., Paton, C., Skorodzien, I., Singh, V., Tan, W., Tyrer, P., & Reilly, J. G. (2018). The clinical effectiveness and cost-effectiveness of Lamotrigine in borderline personality disorder: A randomized placebo-controlled trial. American Journal of Psychiatry, 175(8), 756-764.
Slide 8 of 12
More importantly, all of these patients were considered to have complex personality disorders and I would take that to mean rather severe borderline personality disorder. So, it’s not clear that it would generalize to less severe borderline patients which seem to be the patients in the earlier research studies.
References:
- Crawford, M. J., Sanatinia, R., Barrett, B., Cunningham, G., Dale, O., Ganguli, P., Lawrence-Smith, G., Leeson, V., Lemonsky, F., Lykomitrou, G., Montgomery, A. A., Morriss, R., Munjiza, J., Paton, C., Skorodzien, I., Singh, V., Tan, W., Tyrer, P., & Reilly, J. G. (2018). The clinical effectiveness and cost-effectiveness of Lamotrigine in borderline personality disorder: A randomized placebo-controlled trial. American Journal of Psychiatry, 175(8), 756-764.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
I have used lamotrigine at times in mild to moderate borderline patients, for example, the patients I might see in primary care consultation or collaborative care. It can be helpful for the affective instability. And often, they’ve done quite well with doses in the range of 200 mg a day.
References:
- Reich, D. B., Zanarini, M. C., & Bieri, K. A. (2009). A preliminary study of lamotrigine in the treatment of affective instability in borderline personality disorder. International Clinical Psychopharmacology, 1.
Slide 10 of 12
Lithium, there is only one small study in borderline patients. So, lithium has a very limited role in borderline personality disorder. And of course, it is highly toxic in overdoses so I think it’s not a recommended mood stabilizer in borderline patients.
References:
- Links, P. S., Steiner, M., Boiago, I., & Irwin, D. (1990). Lithium therapy for borderline patients: Preliminary findings. Journal of Personality Disorders, 4(2), 173-181.
- Olabi, B., & Hall, J. (2010). Borderline personality disorder: Current drug treatments and future prospects. Therapeutic Advances in Chronic Disease, 1(2), 59-66.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
So, the key points around mood stabilizers is that the Crawford trial certainly makes me more cautious about using mood stabilizers in borderline patients because of the lack of findings from the best trial.
Lamotrigine can be helpful for the affective instability in mild to moderate borderline patients
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.