Slides and Transcript
Slide 2 of 17
Methadone is a very effective medication and may be one of the most proven medications in addiction in Psychiatry. It has positive impacts on mortality rate, infectious disease as well as psychosocial outcomes like crime and incarceration.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 17
Methadone is a full mu-opioid agonist. It is also an NMDA receptor antagonist. It can be very effective in covering somebody's cravings for over a day. At the same time, the impacts on pain last only six to eight hours.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
Slide 4 of 17
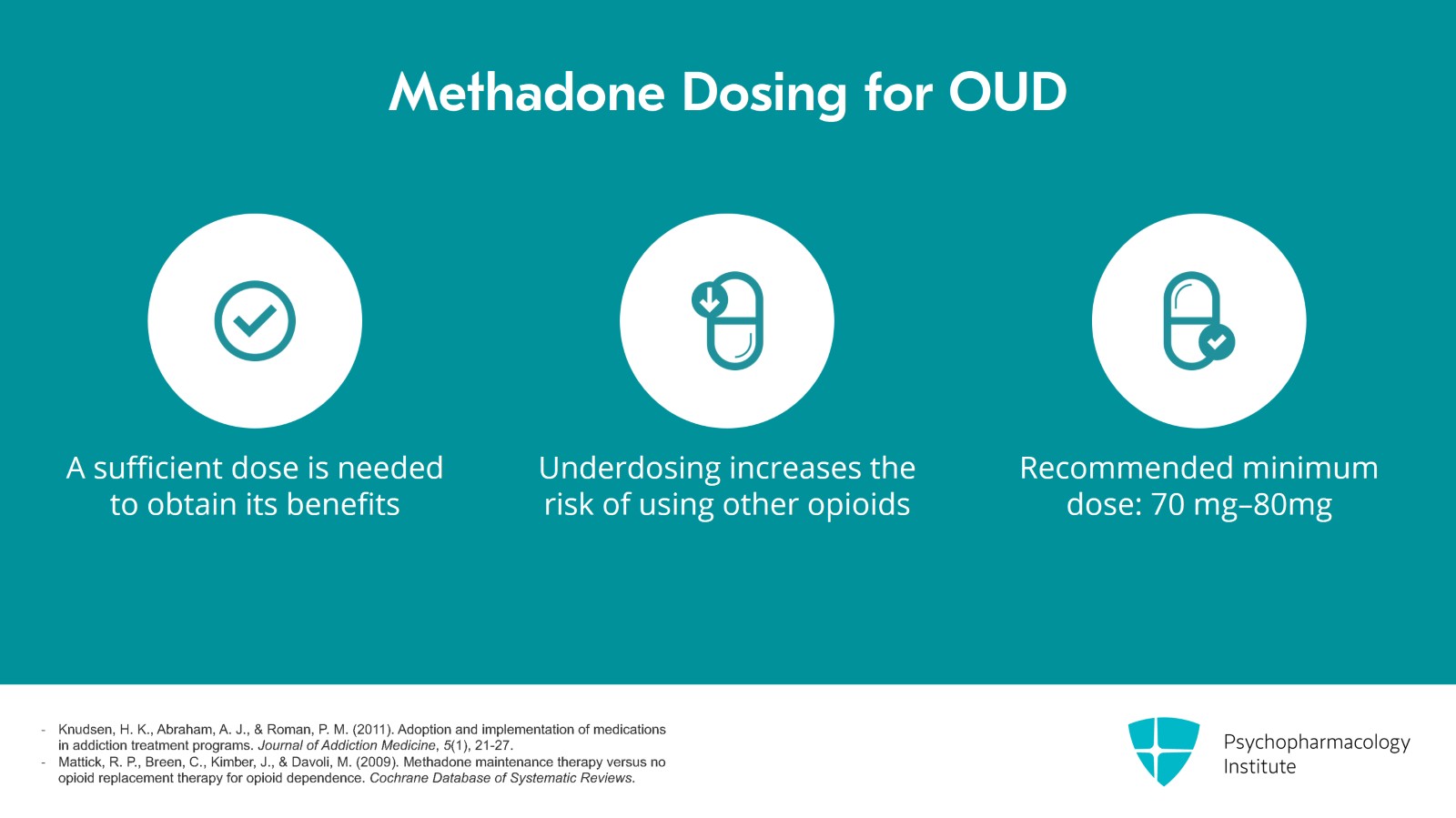
A sufficient dose is needed for somebody to get the benefit of methadone. We know that when underdosed the risk of using other opioids is very high. Therefore, it's very important to make sure that you're seeing a patient who is on methadone that they have a sufficient dose for their opioid use disorder which would be at least 70 to 80 mg.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 17
Currently for opioid use disorder, methadone is only available at an OTP or an opioid treatment program. There have been some recent changes to federal regulations that allow for OTPs to more easily dispense methadone, for example, around telehealth and take-home doses.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
- SAMHSA. (2024). New SAMHSA Rule Expands Access to Medications for the Treatment of Opioid Use Disorder. https://www.polsinelli.com/telehealth/publications/new-samhsa-rule-expands-access-to-medications-for-the-treatment-of-opioid-use-disorder
Slide 6 of 17
There are a lot of practicalities to consider about opioid treatment programs or OTPs. These are federally designated opioid treatment clinics and are the only places that people can get methadone for a substance use disorder. A doctor must place an order from a centrally managed system and only the amount that was ordered is allowed to be dispensed. An individual has to present to the clinic on a certain schedule and obtain their dosing which is usually in the form of a red juice to help prevent injecting.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
- SAMHSA. (2024). New SAMHSA Rule Expands Access to Medications for the Treatment of Opioid Use Disorder. https://www.polsinelli.com/telehealth/publications/new-samhsa-rule-expands-access-to-medications-for-the-treatment-of-opioid-use-disorder
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 17
When patients are allowed to have take-home doses, they must keep with them the doses in a locked box and also keep all of the seals and labels and bottles. This is in an effort to reduce overdose risk to others and also to prevent diversion.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
- SAMHSA. (2024). New SAMHSA Rule Expands Access to Medications for the Treatment of Opioid Use Disorder. https://www.polsinelli.com/telehealth/publications/new-samhsa-rule-expands-access-to-medications-for-the-treatment-of-opioid-use-disorder
Slide 8 of 17
As I noted earlier, federal regulations have recently changed such that OTPs can now dispense up to seven days of take-home doses during the first 14 days of treatment and up to 14 take-home doses for 15 days of treatment and up to 28 take-home days, doses for 31 and on if we believe clinically that a patient can safely handle this amount of take-home doses. Essentially, it is up to a clinician's discretion about how many take-home doses somebody can get and it can be up to a month depending on the case in most phases of treatment.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
- SAMHSA. (2024, January 23). Methadone take-home flexibilities extension guidance. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines/methadone-guidance
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 17
This is extremely beneficial for people who may have had barriers to coming in and getting their methadone who are trying to pursue school or work or other activities. Thus far, data indicates that there's no change to the level of misuse, diversion or harm for methadone take-home doses as we've learned from the public health emergency when exceptions were allowed for longer take-home periods.
References:
- Knudsen, H. K., Abraham, A. J., & Roman, P. M. (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21-27.
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews.
- SAMHSA. (2024, January 23). Methadone take-home flexibilities extension guidance. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines/methadone-guidance
Slide 10 of 17
There are many potential side effects of methadone. Side effects can be respiratory depression especially in people with risk factors. Common to most opioids are constipation, sedation and hyperhidrosis or excessive sweating.
References:
- SAMHSA. (2023, July 31). Medications for substance use disorders. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders
- SAMHSA. (2023, September 18). Methadone. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/methadone
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 17
At high doses, it can be associated with QT prolongation and screening within 30 days should be done for people with significant risk factors for QT prolongation including a history of cardiac arrhythmia or prolonged QT interval, symptoms suggestive of arrhythmia such as episodes of syncope, dizzy spells, palpitations, seizures, medications that may also contribute, hypokalemia, bradycardia, family history of premature death or any other historical information suggestive of a possible cardiac arrhythmia or if the methadone dose is greater than 120 mg a day.
References:
- SAMHSA. (2023, July 31). Medications for substance use disorders. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders
- SAMHSA. (2023, September 18). Methadone. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/methadone
Slide 12 of 17
In those with QTc intervals of greater than 500 ms, methadone should be discontinued or other risk factors should be mitigated.
References:
- SAMHSA. (2023, July 31). Medications for substance use disorders. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders
- SAMHSA. (2023, September 18). Methadone. SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/methadone
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 17
Finally, drug interactions are notable for methadone especially when patients are prescribed or stopped taking a CYP450 34A– inducer or inhibitor. CYP450 inducers like antibiotics, things like rifampin, antiretrovirals and anticonvulsants such as carbamazepine can increase methadone metabolism. Inhibitors can decrease metabolism and increase the risk of overmedication with methadone. Examples of these are some antibiotics like ciprofloxacin, antacids like cimetidine, antifungals like fluconazole, antidepressants like sertraline and more. Methadone can also impact other medications and interactions are always very important with methadone.
References:
- McCance-Katz, E. F., Sullivan, L. E., & Nallani, S. (2010). Drug interactions of clinical importance among the opioids, methadone and buprenorphine, and other frequently prescribed medications: a review. The American Journal on Addictions, 19(1), 4–16.
Slide 14 of 17
Key points around methadone are that methadone is a very effective medication for opioid use disorder impacting many outcomes in addition to opioid use. Methadone is effective in pregnancy. Methadone can only be dispensed as an OTP or an opioid treatment program which has many restrictions.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 17
However, changes to regulations in 2024 have made it slightly easier for patients to access methadone sustainably, for example, provisions which will allow for more take-home doses. Methadone has many side effects. A less common concern, however, and issue for people with risk factors is QTc prolongation.
Slide 16 of 17
Other side effects are sedation, respiratory depression and constipation as it occurs with other opioids. There are also many common medications that can induce and inhibit methadone metabolism.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.