Slides and Transcript
Slide 2 of 15
Well, there are some issues with clozapine-related sialorrhea which are really important.
For one thing, it’s common. The incidence rate is 30% to 80%, not always dose dependent.
Not only does this cause a social problem especially if people drool during the daytime but the bigger concern is nighttime aspiration which may increase the risk for pneumonia.
References:
- Gurrera, R. J., Parlee, A. C., & Perry, N. L. (2016). Aspiration pneumonia. Journal of Clinical Psychopharmacology, 36(2), 174-176.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
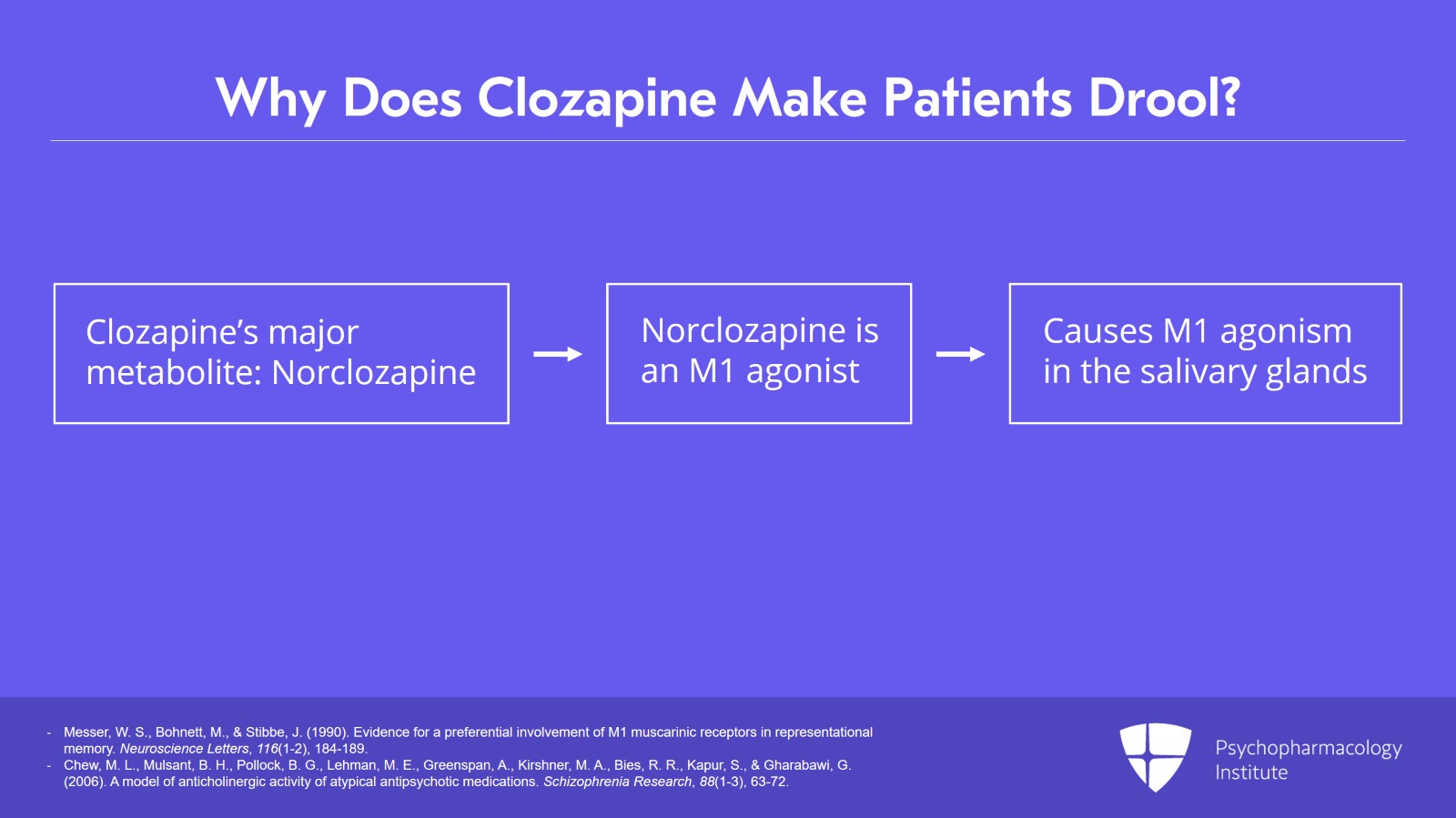
Why does clozapine make people drool?
Well, clozapine has a major metabolite, norclozapine, which we also think contributes partly to the efficacy. But while clozapine is predominantly a muscarinic antagonist at M1 receptors, norclozapine is an M1 agonist. And that’s why we get that unusual combination of a drug which makes you constipated because of the clozapine and it makes you drool because of the M1 agonism acting at the salivary glands.
References:
- Messer, W. S., Bohnett, M., & Stibbe, J. (1990). Evidence for a preferential involvement of M1 muscarinic receptors in representational memory. Neuroscience Letters, 116(1-2), 184-189.
- Chew, M. L., Mulsant, B. H., Pollock, B. G., Lehman, M. E., Greenspan, A., Kirshner, M. A., Bies, R. R., Kapur, S., & Gharabawi, G. (2006). A model of anticholinergic activity of atypical antipsychotic medications. Schizophrenia Research, 88(1-3), 63-72.
Slide 4 of 15
The number one rule of thumb is that we want to first try locally applied agents to treat sialorrhea.
Systemic anticholinergics are the drugs of last resort because they double the risk for ileus.
References:
- Bird, A. M., Smith, T. L., & Walton, A. E. (2011). Current treatment strategies for clozapine-induced sialorrhea. Annals of Pharmacotherapy, 45(5), 667-675.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
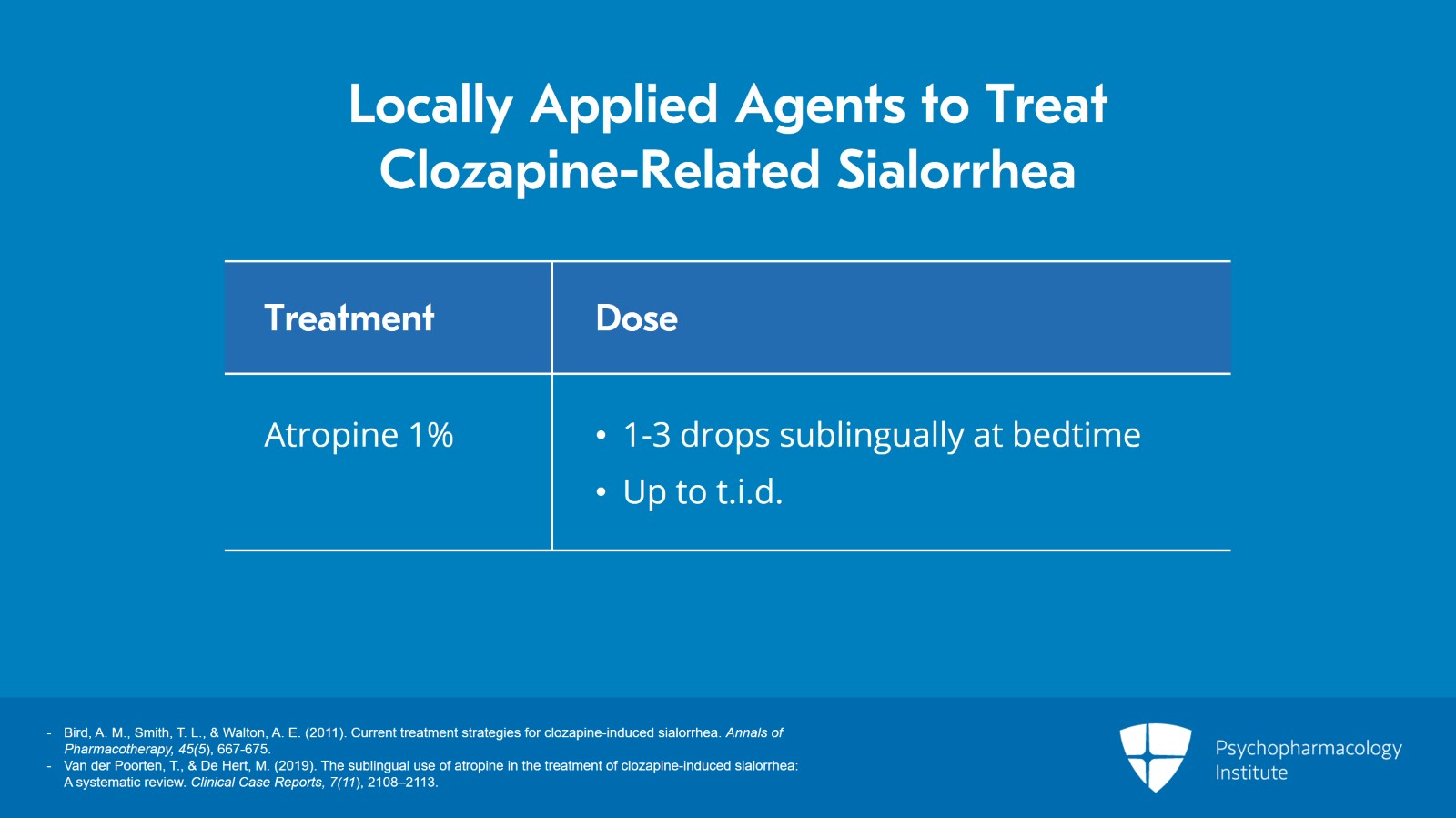
Locally applied agents to treat sialorrhea.
The first treatment of choice is atropine 1% drops. The dosing is one to three drops sublingually initially at bedtime and if needed up to t.i.d.
The idea is we really do want to dry people up at night so they don’t aspirate. When I trained, we were taught to tell patients, oh, put a towel under your head to protect the pillow. Well, good for the pillow but that’s not so helpful for the patient.
References:
- Bird, A. M., Smith, T. L., & Walton, A. E. (2011). Current treatment strategies for clozapine-induced sialorrhea. Annals of Pharmacotherapy, 45(5), 667-675.
- Van der Poorten, T., & De Hert, M. (2019). The sublingual use of atropine in the treatment of clozapine-induced sialorrhea: A systematic review. Clinical Case Reports, 7(11), 2108–2113.
Slide 6 of 15
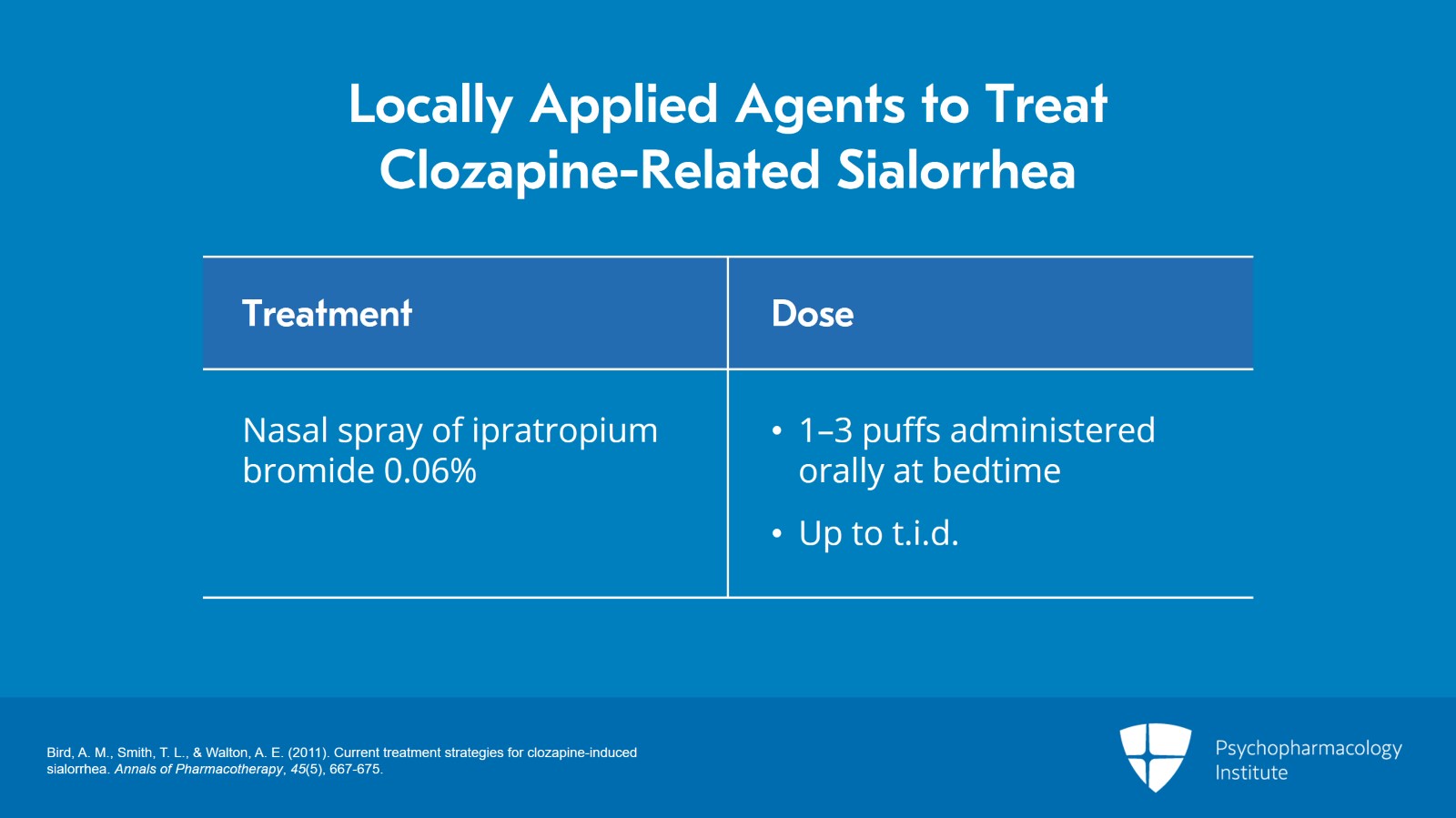
If that doesn’t work up to the maximum dose of three drops sublingually t.i.d., you can try the anticholinergic nasal spray ipratropium bromide but use the higher strength of 0.06%. While this was developed as a nasal spray, they’re going to spray it in their mouth.
Again, the dosing is one to three puffs in the mouth initially at bedtime and if needed up to t.i.d. with the same instructions.
References:
- Bird, A. M., Smith, T. L., & Walton, A. E. (2011). Current treatment strategies for clozapine-induced sialorrhea. Annals of Pharmacotherapy, 45(5), 667-675.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
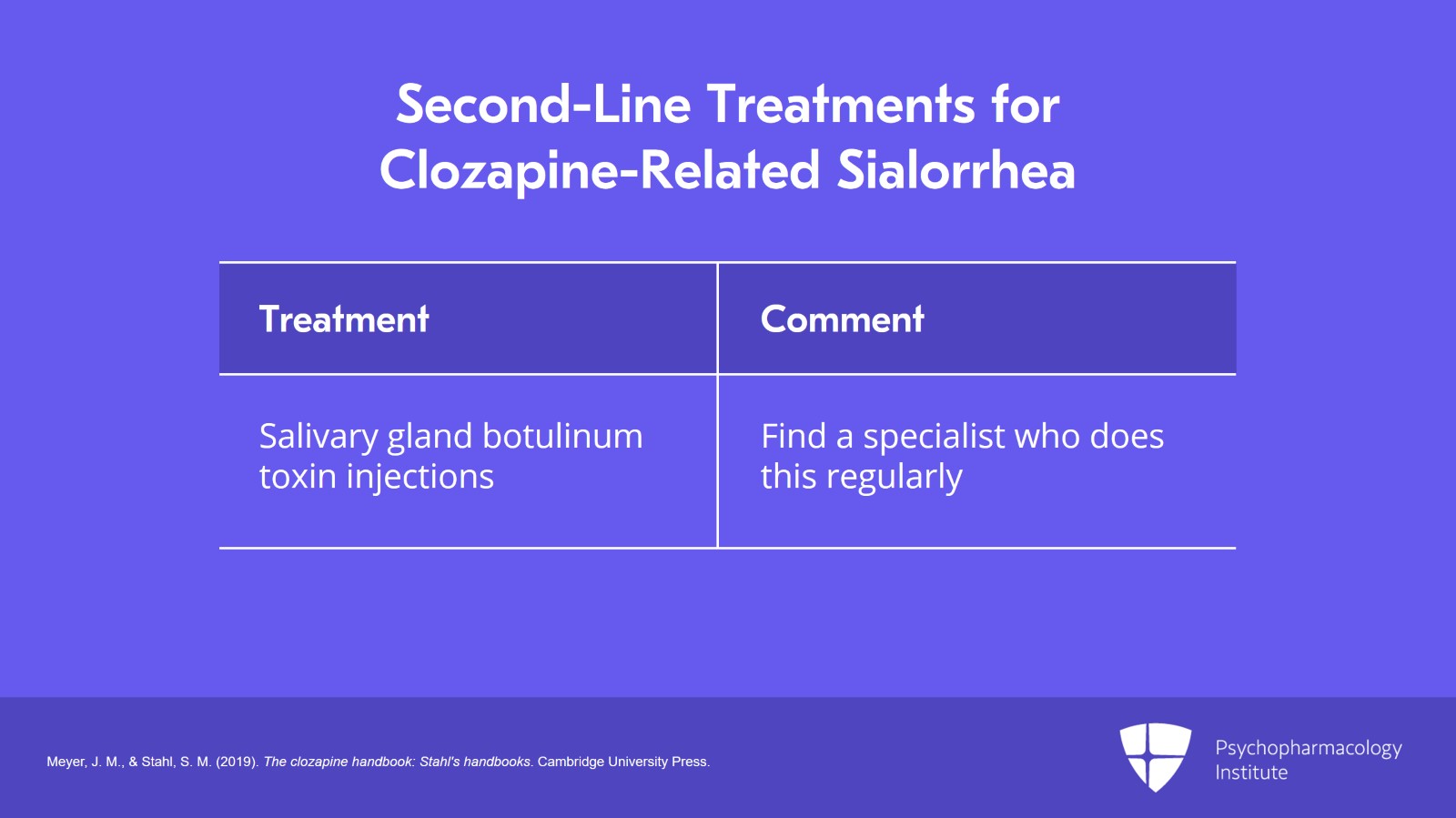
If the locally applied agents don’t work, here are the second-line treatments.
Number one on the list are salivary gland botulinum toxin injections.
Now, I appreciate this may not be available to everybody listening to this but if you look around there are people out there who do this.
Try to find a movement disorder specialist, a neurologist, an ENT surgeon, maybe a physical medicine physician who does this on a regular basis for sialorrhea.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Slide 8 of 15
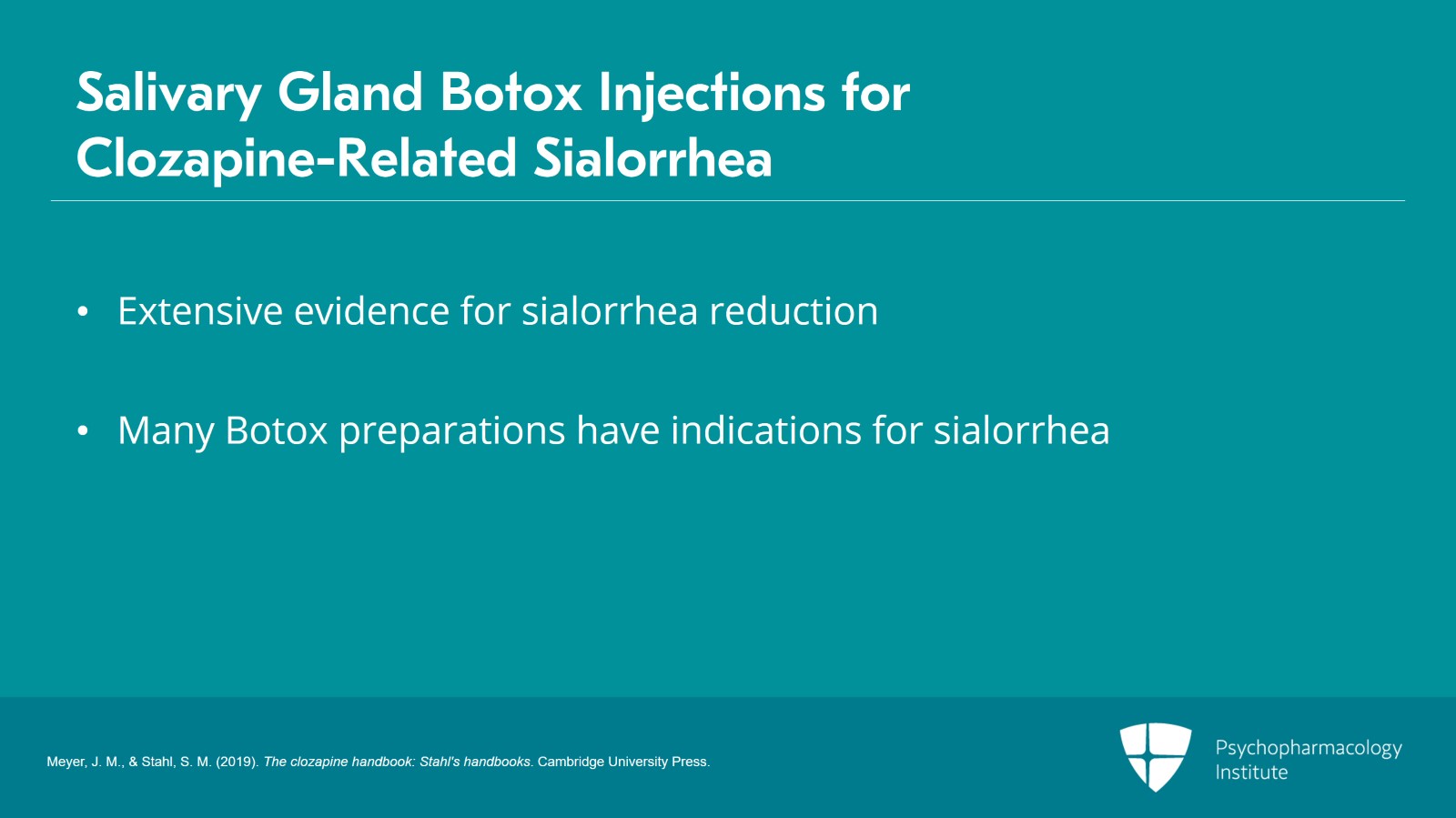
Importantly, there’s extensive evidence for sialorrhea reduction. There are six double-blind studies.
Many of the Botox preparations actually have indications now for sialorrhea. With relevance to us, there are numerous case reports and case series of people using botulinum toxin injections into the salivary glands with both Botox A and B for clozapine-related sialorrhea.
Where I have worked for many years at the California State Hospital system, we’ve now established a Botox clinic for people who have clozapine-related sialorrhea.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
The beauty of the Botox injection is the same as for the locally applied agents.
We do not get systemic adverse effects.
It is very well tolerated.
Once it starts working, the effects may last weeks up to months.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Slide 10 of 15
It does take a bit of time for them to work.
Unlike somebody with a neurological disorder like Parkinson’s disease, we’re actually trying to interfere with the action of a drug, clozapine, or its metabolite, norclozapine, which is being administered on a daily basis.
So it may take a number of weeks for the toxin to penetrate into the salivary glands and disable the mechanism which results in drooling.
Once you give it some time to build up, often there is significant reduction but it may not completely resolve the problem.
But the goal is maybe it makes it better enough that they can now use the locally applied agents to manage the problem.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
If Botox is not available or does not work, the drug of last resort is glycopyrrolate. This is a peripherally acting anticholinergic that does not penetrate the blood-brain barrier and thus you avoid all of the CNS effects from using other anticholinergics like benztropine, diphenhydramine or outside the US, hyoscine.
There are several randomized trials supporting its efficacy for clozapine-related sialorrhea. However, it adds to clozapine’s anticholinergic burden and doubles the risk for ileus. Once you start glycopyrrolate, you have to manage the constipation problem aggressively and we’ll be discussing that shortly.
References:
- Liang, C., Ho, P., Shen, L., Lee, W., Yang, F., & Chiang, K. (2010). Comparison of the efficacy and impact on cognition of glycopyrrolate and biperiden for clozapine-induced sialorrhea in schizophrenic patients: A randomized, double-blind, crossover study. Schizophrenia Research, 119(1-3), 138-144.
Slide 12 of 15
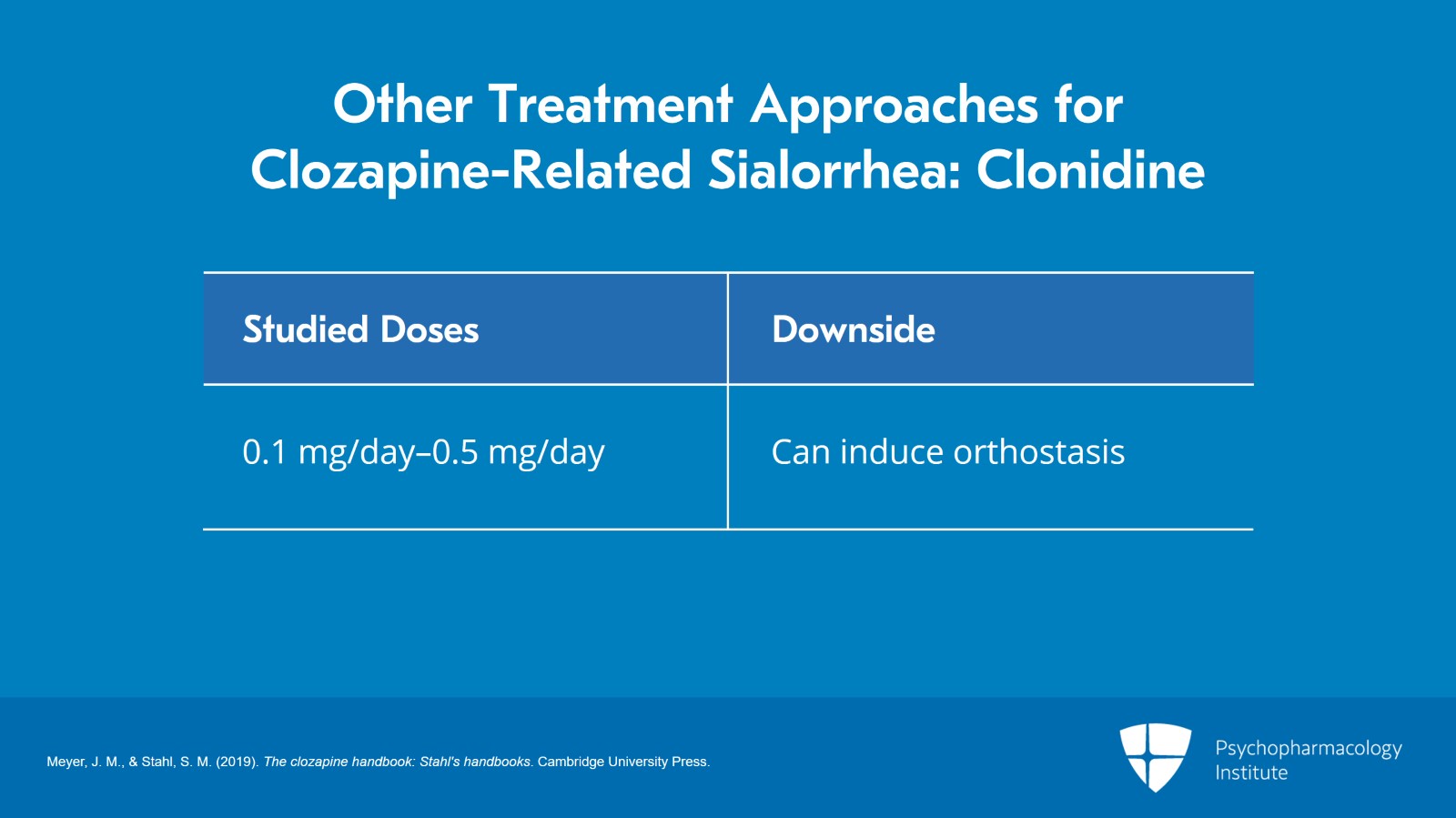
Other treatment approaches based on case reports or case series include the alpha-2 agonist, clonidine.
Alpha-2 neurotransmission is actually involved in the salivary reflex and if you stimulate it with clonidine you actually lower salivary output.
The doses of clonidine studied have been between 0.1 and 0.5 mg per day. The big downside of clonidine is that it itself can induce orthostasis and this may be a problem in somebody who’s already perhaps experiencing orthostasis from clozapine. Clonidine is not very commonly used but it does exist and there is some supportive data for this purpose.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
The key point is that you really want to treat sialorrhea both for its social consequences as well as the medical consequence of nighttime aspiration.
Orally applied medications such as atropine 1% drops or ipratropium 0.06% spray are preferred because they do not increase constipation risk in a way that the peripherally acting anticholinergics do.
Slide 14 of 15
Consider trying botulinum toxin injections before using glycopyrrolate. These products are indicated for sialorrhea and they may allow you to avoid having to use the systemic anticholinergic, glycopyrrolate.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.