Slides and Transcript
Slide 1 of 23
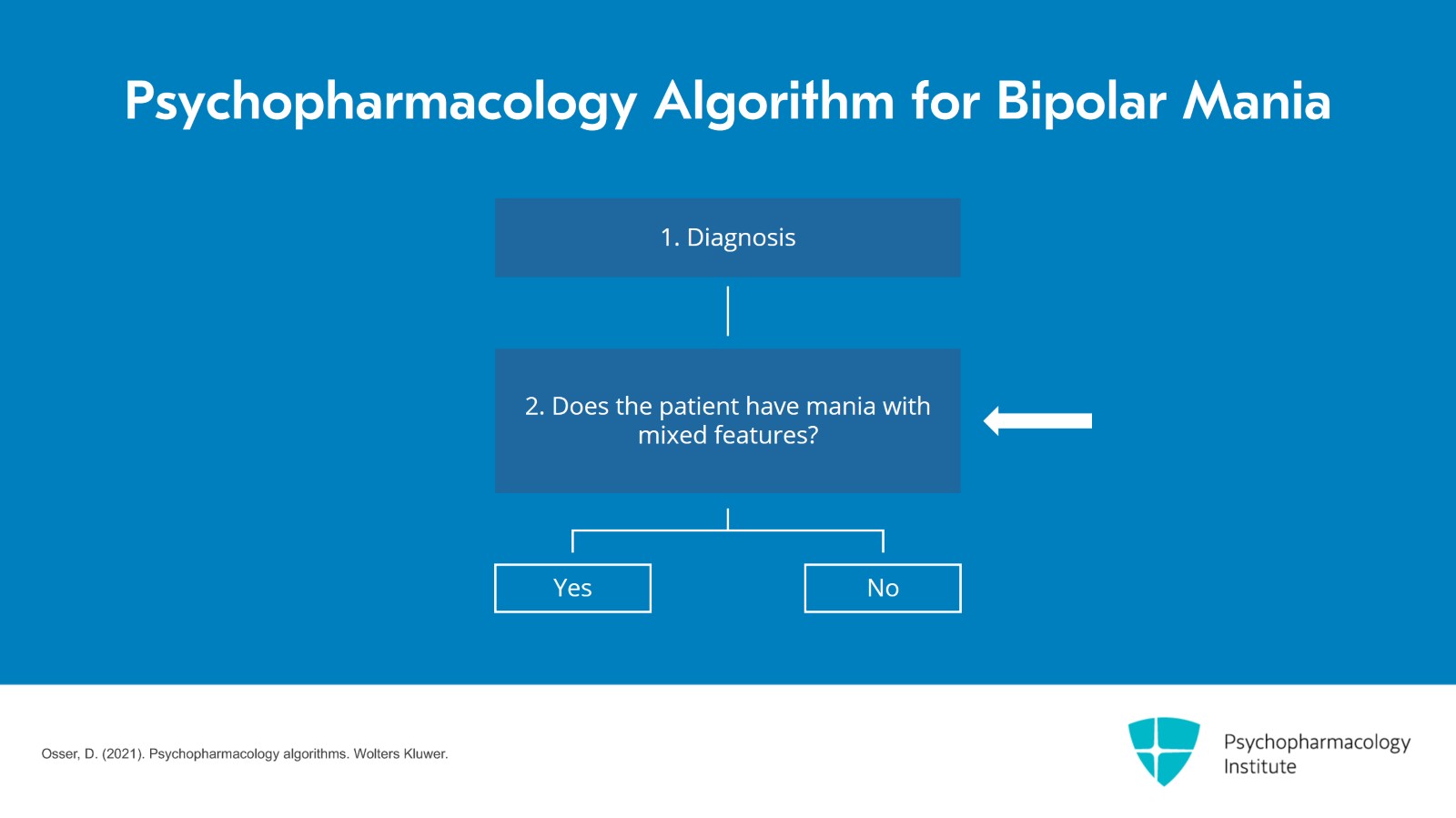
Video 3 of the Algorithm for Managing Bipolar Mania and Severe Hypomania with Psychopharmacology.
Slide 2 of 23
We've gotten to the point in the algorithm where we are going to actually select treatment for this acute manic episode. And at this point, there is a bifurcation in the algorithm. There are two separate algorithms depending on whether the patient meets criteria for mania with mixed depressive features or whether they do not, they have classic mania without significant depressive symptoms.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 23
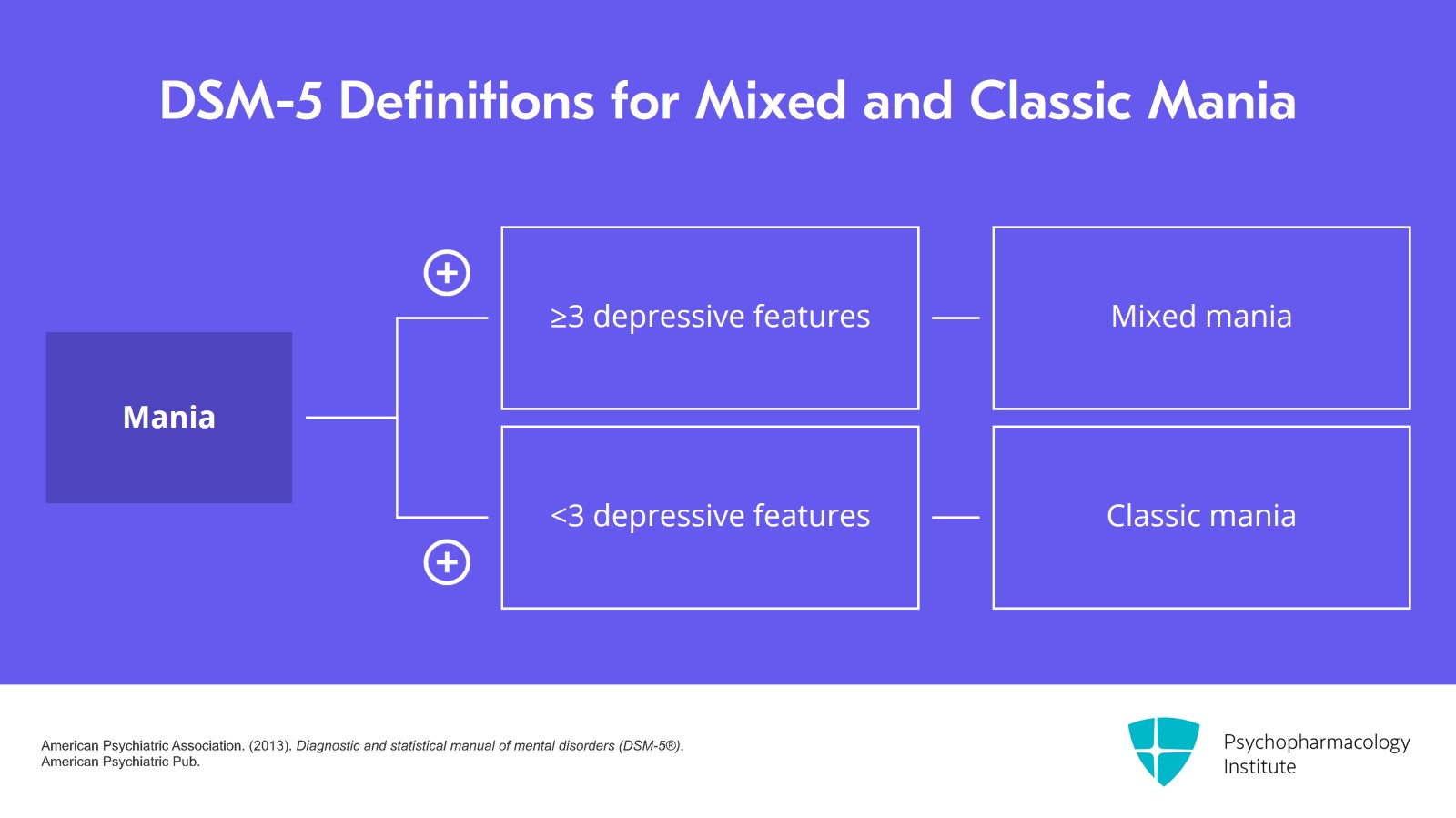
The DSM-5 defines mixed mania as mania with three or more symptoms of depression. Whereas, if it's less than that, it's considered classic mania.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
Slide 4 of 23
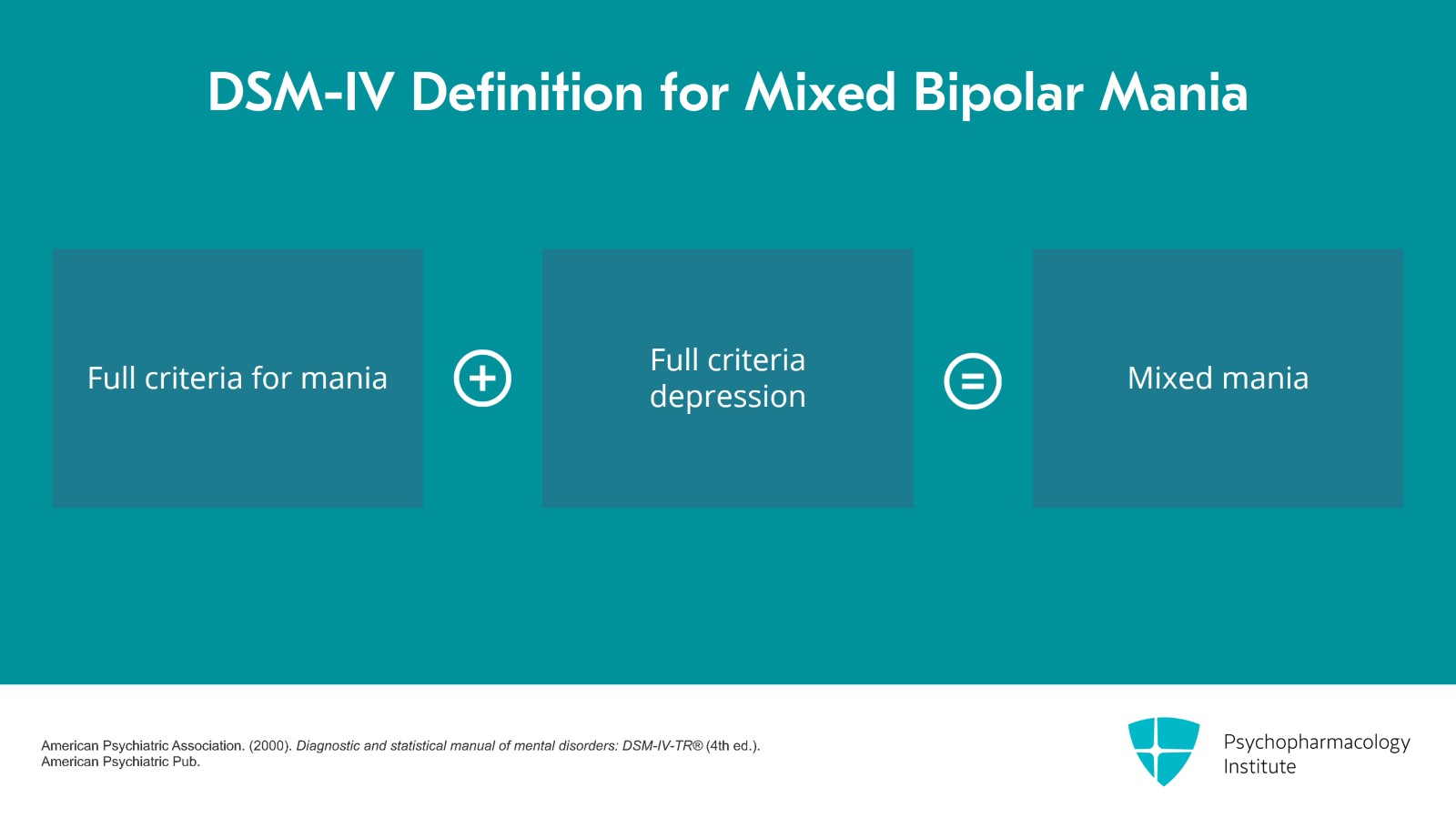
Now, DSM-4 had a whole different definition for mixed bipolar disorder. They required the full criteria for mania and the full criteria for depression to call it mixed. That was changed in DSM-5 and there has been relatively little study of DSM-5 mixed mania. So some of the evidence we've had to look at for the use of medication for mixed mania go back to studies in the old DSM-4 definition. Some of the studies with mixed mania though have used a criteria of two depressive symptoms.
References:
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR® (4th ed.). American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 23
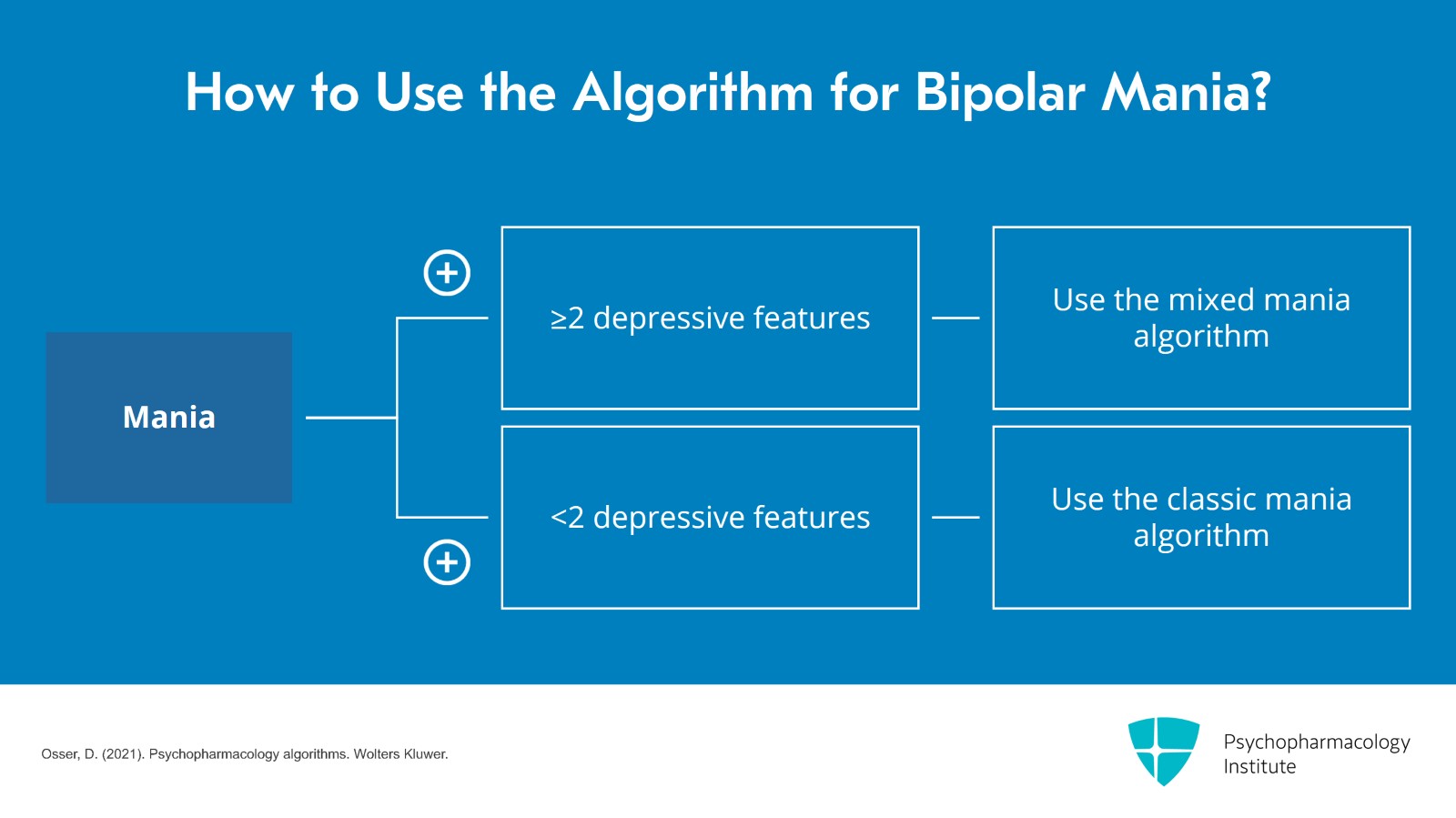
So I think you should probably follow our algorithm for mixed if they have two depressive features rather than needing three. But for those with less than two, you should follow the algorithm for classic mania.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 6 of 23
I will begin by discussing the algorithm for mixed mania. Mixed mania can be up to 40% of cases of mania. So it's important to diagnose it. But the bottom line on mixed mania is it responds less well in general to medications, you often need two medications to treat it and the treatment algorithm is different.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 23
So what is our first-line recommendation for mania with mixed features? It is quetiapine, cariprazine, or another second-generation antipsychotic which I'll explain in a second. Why is that? They have the best evidence in these studies of mixed mania according to two reviews that I've cited.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 8 of 23
Several second-generation antipsychotics have been found effective for bipolar depression and for these depressive symptoms in mixed mania. And of those, quetiapine probably has the most evidence of working for acute bipolar depression and for mixed mania with those depressive symptoms. Quetiapine is not FDA approved for mixed, I should point out, but the studies are positive. There are three positive studies.
References:
- Janicak, P. G., & Rado, J. T. (2011). Quetiapine monotherapy for bipolar depression. Expert Opinion on Pharmacotherapy, 12(10), 1643–1651.
- Calabrese, J. R., Keck, P. E., Jr, Macfadden, W., Minkwitz, M., Ketter, T. A., Weisler, R. H., Cutler, A. J., McCoy, R., Wilson, E., & Mullen, J. (2005). A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. The American Journal of Psychiatry, 162(7), 1351–1360.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 23
Now, cariprazine is the newest bipolar medication on the block that we have available. It's much more expensive than quetiapine. Often, it's not allowed in different formularies but we included it as a preferred choice because it too has efficacy for bipolar depression. Cariprazine actually got an FDA approval for mixed bipolar states along with mania. So it deserves to be a first-line consideration at least if you can afford it. Now, on the downside, cariprazine has not been studied as a maintenance treatment as yet for bipolar mania or bipolar in general.
References:
- Citrome L. (2019). Cariprazine for bipolar depression: What is the number needed to treat, number needed to harm and likelihood to be helped or harmed?. International Journal of Clinical Practice, 73(10), e13397.
Slide 10 of 23
Quetiapine has and appears effective as a maintenance treatment. Hence, we have a slight preference for it over cariprazine because that was one of our criteria. Remember back to video 1, I said it's very important to consider not only what works for the mania but what works to prevent the depression and prevent future episodes of mania. Quetiapine seems to have the best evidence for that. That's why it's our first choice SGA for mixed mania. It isn't extremely effective. It isn't at the top of the list for pure efficacy for the mania in the meta-analyses but it does have these other benefits that accrue to its preference.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 23
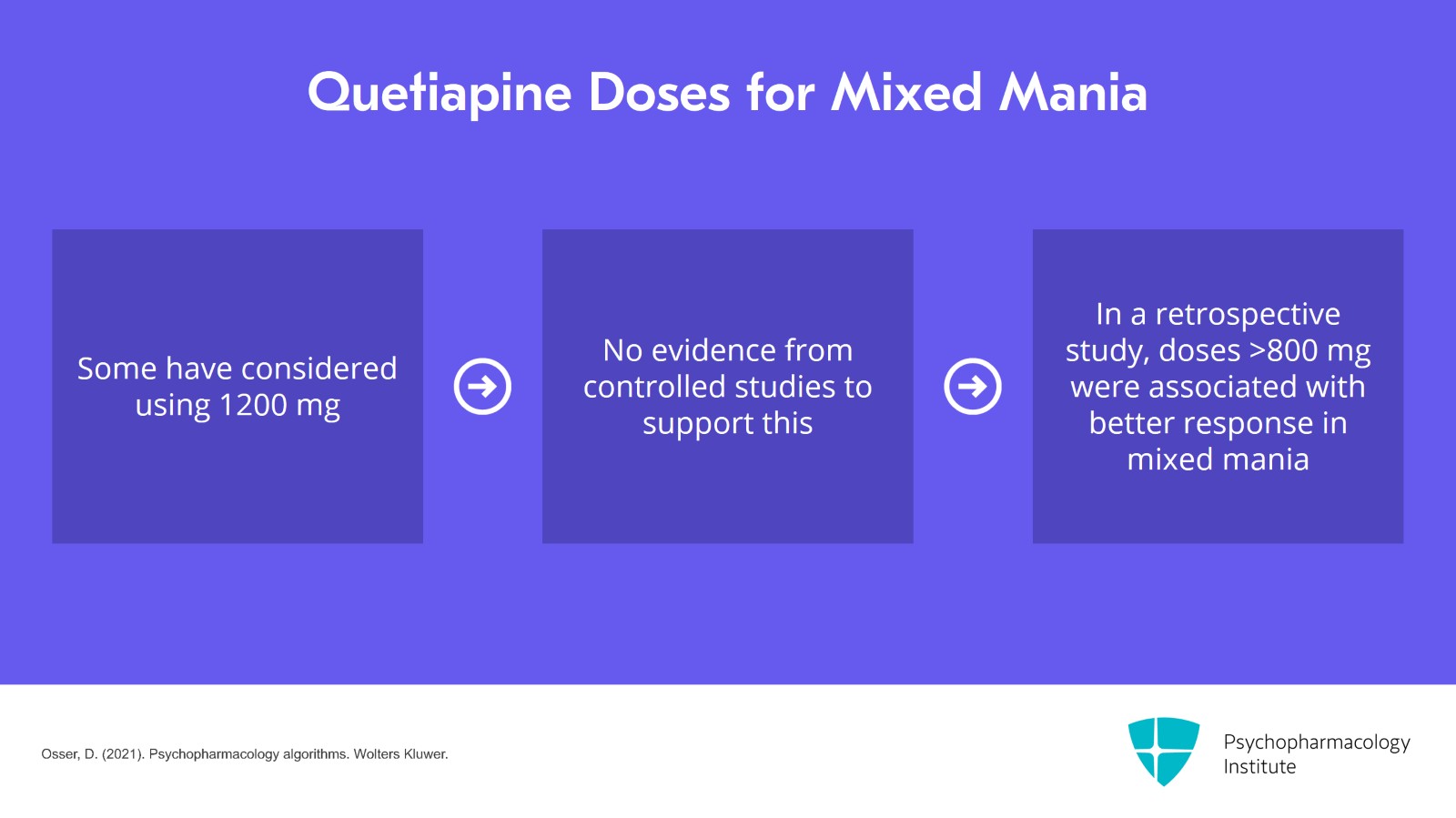
Now, I do want to point out that you seem to need higher doses of quetiapine to get this benefit in mixed mania. 600 to 800 seems to be what is needed.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 12 of 23
Now, some have considered trying 1200 which means going over the PDR max of 800. There is no evidence from controlled studies to support that. But in a paper retrospectively reviewing 50 patients which we cite in our algorithm, for mixed cases only, it seemed that doses over 800 were sometimes used and were associated with better response but not in the nonmixed mania cases. So if you're going to go over the 800, consider it for the mixed cases but nonmixed cases or classic mania, don't go over 800.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 23
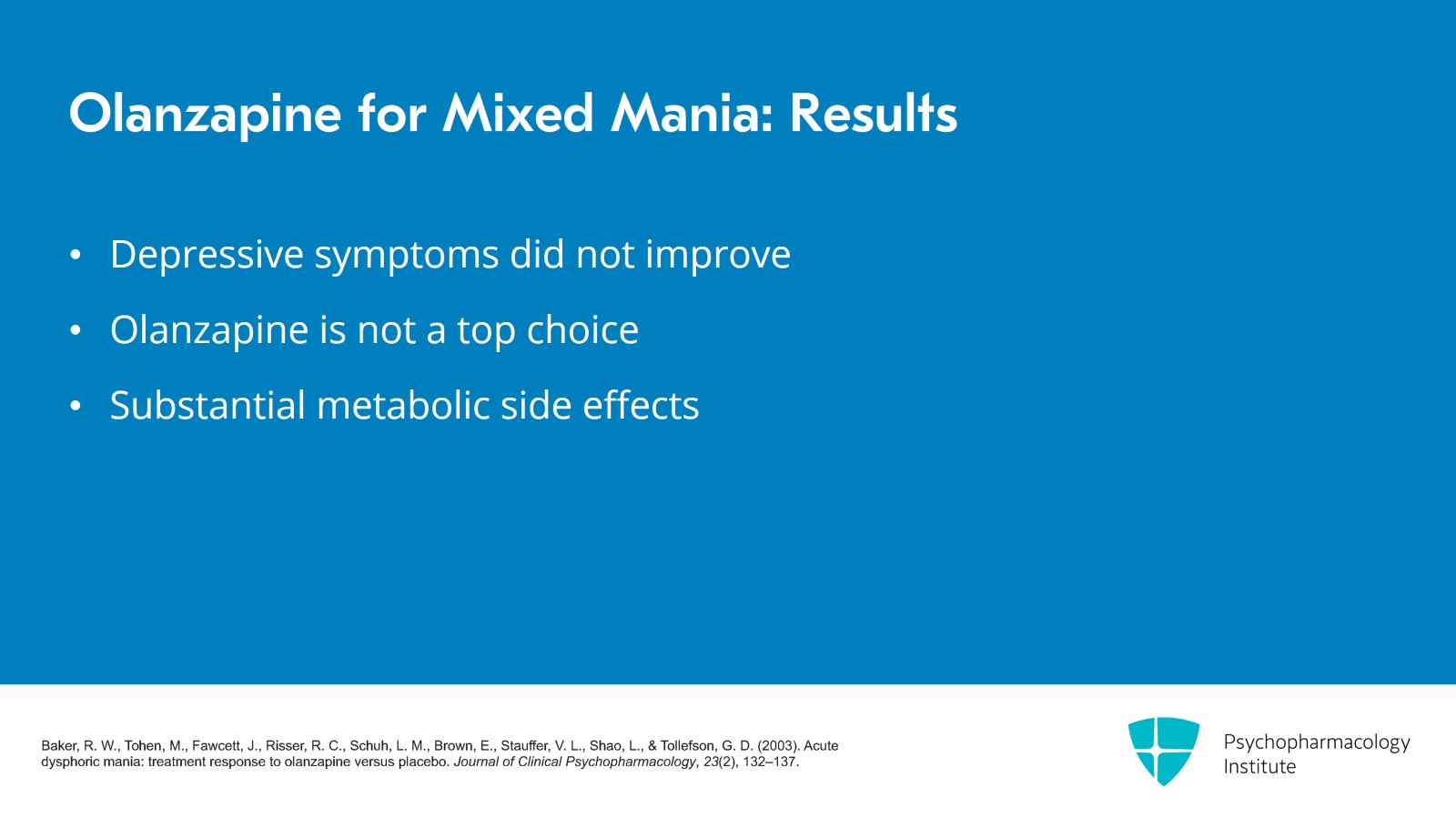
Now, there's a whole lot of other SGAs that are effective for mania. I'll comment briefly on each of them. First of all, olanzapine, it actually had a larger effect size in meta-analyses than quetiapine. Cipriani's meta-analysis found it was 0.43 for olanzapine effect size different from placebo and 0.37 reduction with quetiapine in manic symptoms versus placebo in the overall data. That's not a statistically significant difference. It's a slight numeric difference. Basically, it means that there was 43% improvement on average with olanzapine, 37% with quetiapine. But these results were in general patients.
References:
- Cipriani, A., Barbui, C., Salanti, G., Rendell, J., Brown, R., Stockton, S., Purgato, M., Spineli, L. M., Goodwin, G. M., & Geddes, J. R. (2011). Comparative efficacy and acceptability of antimanic drugs in acute mania: A multiple-treatments meta-analysis. Lancet, 378(9799), 1306–1315.
Slide 14 of 23
The results in mixed patients with olanzapine for which we have some separate data by were not good. Depressive symptoms were not improved by olanzapine. So that's why we don't have it as a top choice. We also in any case don't have olanzapine as a top choice even for mania that's classic due to its metabolic side effects which are substantial.
References:
- Baker, R. W., Tohen, M., Fawcett, J., Risser, R. C., Schuh, L. M., Brown, E., Stauffer, V. L., Shao, L., & Tollefson, G. D. (2003). Acute dysphoric mania: treatment response to olanzapine versus placebo. Journal of Clinical Psychopharmacology, 23(2), 132–137.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 23
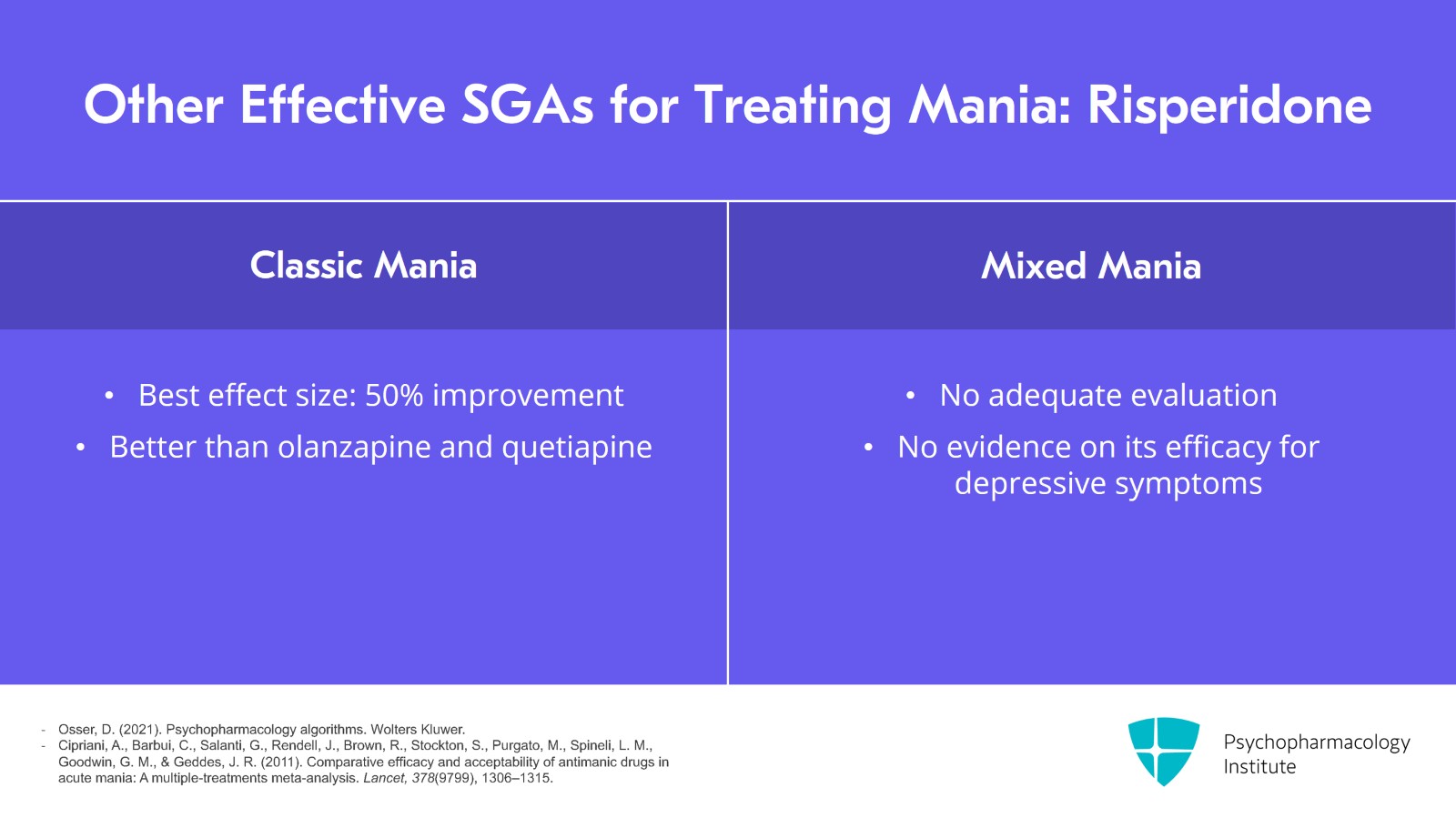
Risperidone is another option. It had the best effect size against acute mania in the meta-analyses. It was 0.50 improvement. That's a 50% improvement. That made it better than the olanzapine and the quetiapine. However, it's had no adequate evaluation in mixed and no studies in bipolar depression. We have no idea whether this drug works for depressive symptoms either acutely or in the context of mania. So that's why we have it down here as another, as a lower option.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
- Cipriani, A., Barbui, C., Salanti, G., Rendell, J., Brown, R., Stockton, S., Purgato, M., Spineli, L. M., Goodwin, G. M., & Geddes, J. R. (2011). Comparative efficacy and acceptability of antimanic drugs in acute mania: A multiple-treatments meta-analysis. Lancet, 378(9799), 1306–1315.
Slide 16 of 23
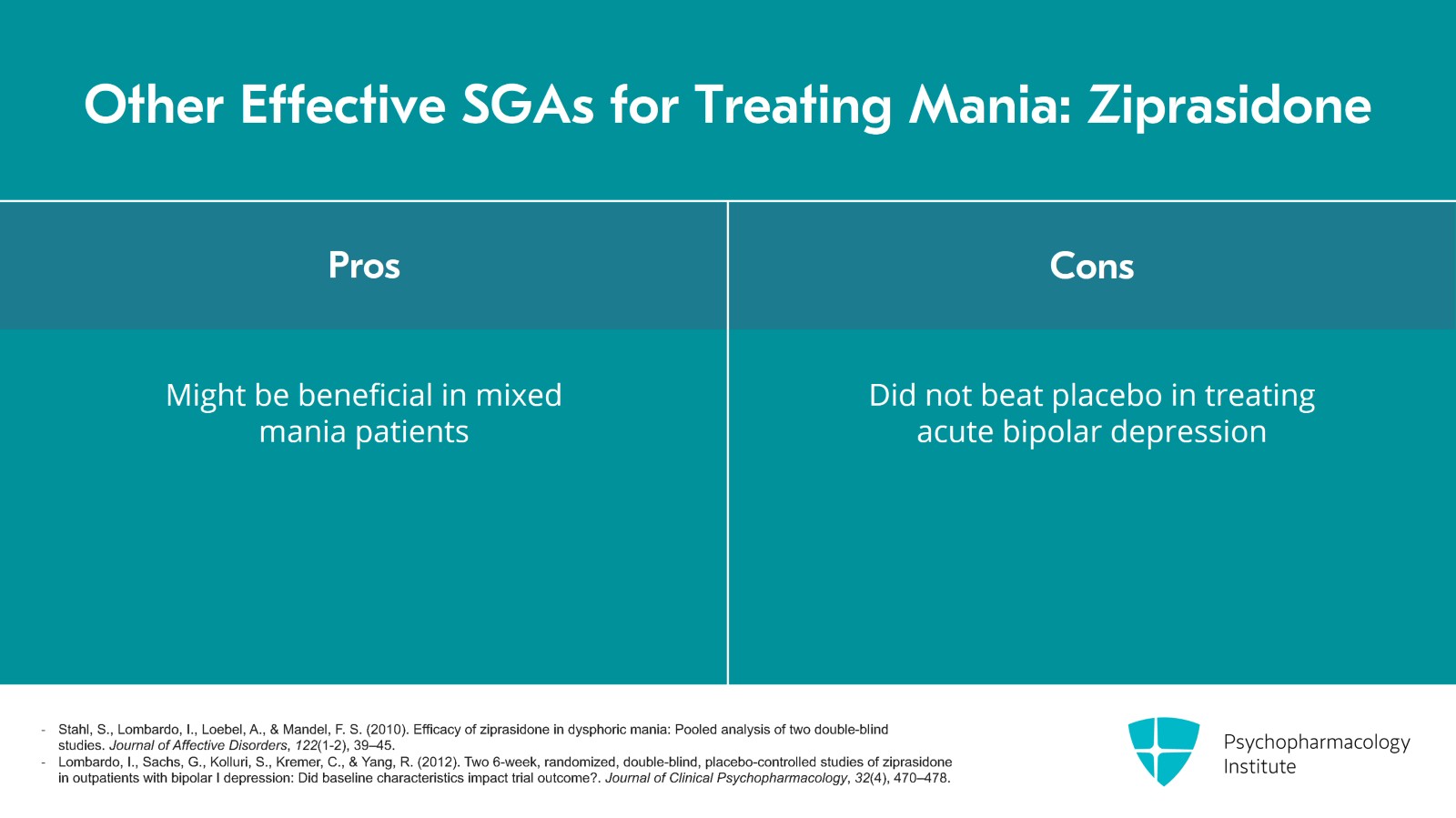
Ziprasidone, significant benefit was found in a post hoc analysis of results in mixed mania patients. That's kind of encouraging about ziprasidone. However, it has been tried in acute bipolar depression in two randomized trials and did not beat placebo in either. So that's why we don't prefer it for mixed cases.
References:
- Stahl, S., Lombardo, I., Loebel, A., & Mandel, F. S. (2010). Efficacy of ziprasidone in dysphoric mania: Pooled analysis of two double-blind studies. Journal of Affective Disorders, 122(1-2), 39–45.
- Lombardo, I., Sachs, G., Kolluri, S., Kremer, C., & Yang, R. (2012). Two 6-week, randomized, double-blind, placebo-controlled studies of ziprasidone in outpatients with bipolar I depression: Did baseline characteristics impact trial outcome?. Journal of Clinical Psychopharmacology, 32(4), 470–478.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 23
Similar situation with aripiprazole, there are reports that in some mixed patients it had benefits but it too has been tried in two randomized controlled trials for acute bipolar depression and did not beat placebo. So we think of it as not effective for depression. So we don't want to use it because depression is often the next step after the mania resolves.
References:
- Suppes, T., Eudicone, J., McQuade, R., Pikalov, A., 3rd, & Carlson, B. (2008). Efficacy and safety of aripiprazole in subpopulations with acute manic or mixed episodes of bipolar I disorder. Journal of Affective Disorders, 107(1-3), 145–154.
- Thase, M. E., Jonas, A., Khan, A., Bowden, C. L., Wu, X., McQuade, R. D., Carson, W. H., Marcus, R. N., & Owen, R. (2008). Aripiprazole monotherapy in nonpsychotic bipolar I depression: Results of 2 randomized, placebo-controlled studies. Journal of Clinical Psychopharmacology, 28(1), 13–20.
Slide 18 of 23
And lurasidone, finally, it's an antipsychotic that is approved for bipolar depression. Never studied in mania though so we don't use it for mania.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 23
Now, what about lithium? You're wondering, why don't we have it? It doesn't seem to work well in mixed mania as best we can tell. Now, in the bipolar depression algorithm we noted that lithium has not been found effective as a monotherapy for bipolar depression. The SGAs have though, several of them. So we think that patients with depressive symptoms along with their mania would probably have poor response to lithium. So we don't have it as a first choice.
References:
- Fagiolini, A., Cuomo, A., & McIntyre, R. S. (2022). Lithium. Pocket Guide to Practical Psychopharmacology, 1-22.
- Crapanzano, C., Casolaro, I., Amendola, C., & Damiani, S. (2022). Lithium and Valproate in bipolar disorder: From international evidence-based guidelines to clinical predictors. Clinical Psychopharmacology and Neuroscience, 20(3), 403-414.
Slide 20 of 23
The key points that we made in focusing on initial treatment was that we think the first-line treatment is with a second-generation antipsychotic and of these, quetiapine is preferred but cariprazine is interesting because of its efficacy in depression as well as mania but it has no maintenance data as yet.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 23
The available evidence suggests lithium would be disappointing as a first-line treatment for mixed mania because it has not done well in general for acute bipolar depression symptoms. And then we also in this video reviewed the merits of other SGAs if you don't want to use quetiapine or cariprazine first line. They have varying but in general weaker evidence of likely effectiveness for depressive symptoms in acute mixed mania patients.
Slide 22 of 23
And this ability to be helpful for depression is an important consideration in prioritizing treatments as we discussed in the introductory module of this talk.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.