Slides and Transcript
Slide 2 of 20
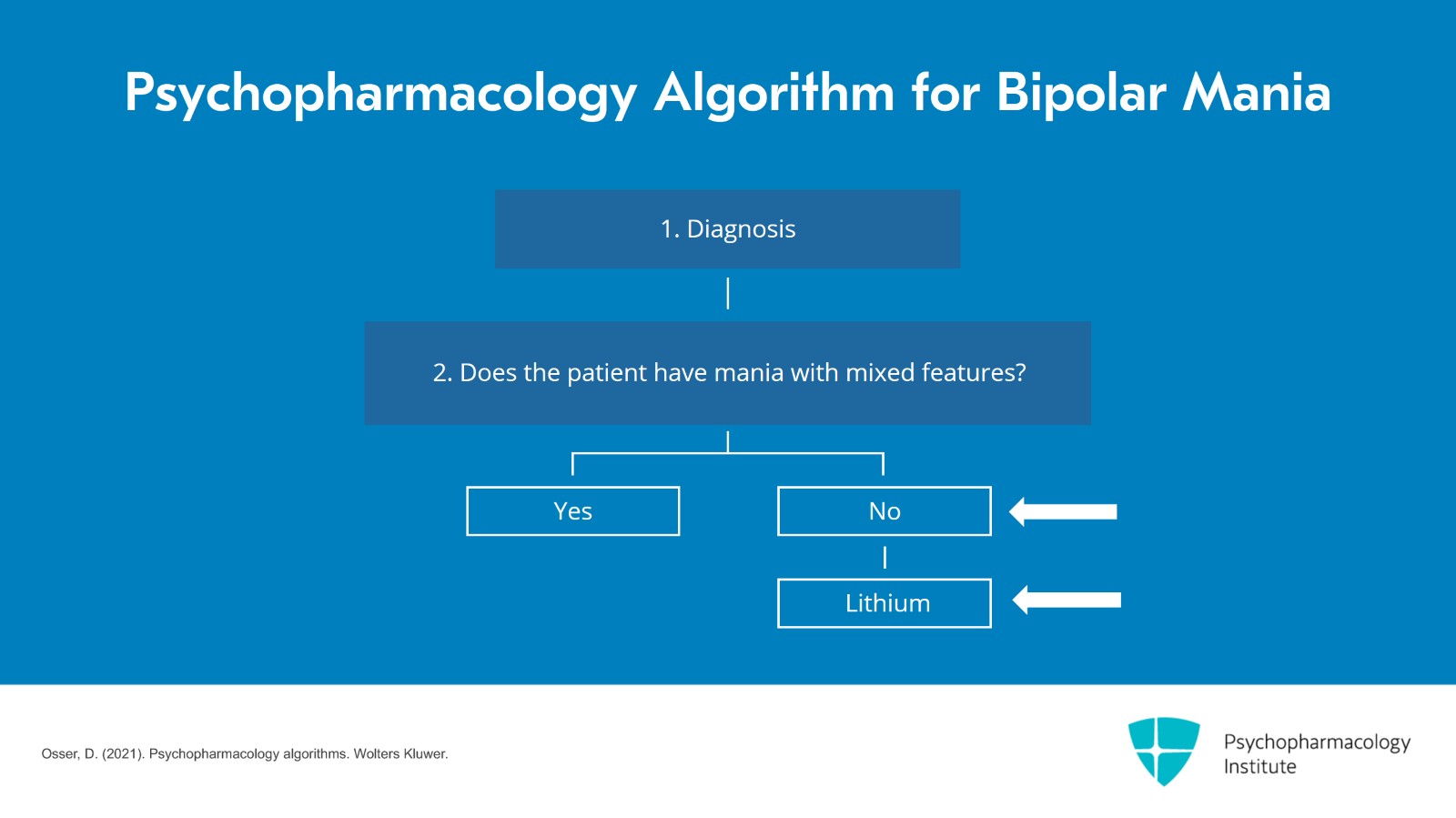
And in this video, we are going to discuss the part of the flow chart that is concerned with people with classic mania, not mixed. And our recommendation for the first drug to use for them for their acute mania is lithium, not a second-generation antipsychotic or valproate which are so commonly used in clinical practice.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 20
Why do we pick lithium first? First of all, it's the only mood stabilizer with FDA approved monotherapy maintenance efficacy for mania and depression. And as you may recall from video 1, we put great importance on choosing medication for mania that's also going to work for preventing future manias and especially future depressions. And lithium is the only mood stabilizer with FDA approval for all those uses.
References:
- Rybakowski J. K. (2011). Lithium in neuropsychiatry: A 2010 update. The World Journal of Biological Psychiatry, 12(5), 340–348.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 4 of 20
It's also the only bipolar med effective for suicide risk which is a huge issue in bipolar disorder. It's better than valproate, olanzapine and quetiapine for other self-harm and unintentional injury according to some studies cited here. And lithium is also the only medication we have for bipolar disorder with clear neuroprotective effects. It actually slows or may even arrest and reverse some of the cortical gray shrinkage that occurs over years from bipolar disorder.
References:
- Baldessarini, R. J., Tondo, L., Davis, P., Pompili, M., Goodwin, F. K., & Hennen, J. (2006). Decreased risk of suicides and attempts during long-term lithium treatment: a meta-analytic review. Bipolar Disorders, 8(5 Pt 2), 625–639.
- Rybakowski J. K. (2011). Lithium in neuropsychiatry: A 2010 update. The World Journal of Biological Psychiatry, 12(5), 340–348.
- Velosa, J., Delgado, A., Finger, E., Berk, M., Kapczinski, F., & de Azevedo Cardoso, T. (2020). Risk of dementia in bipolar disorder and the interplay of lithium: A systematic review and meta-analyses. Acta Psychiatrica Scandinavica, 141(6), 510–521.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 20
Now, there are more advantages. I haven't listed all of them. Patients on lithium monotherapy in three large community surveys were less likely to need any med changes compared to all other regimens. We have three major surveys of people in the community, how they're doing, what are they on with their bipolar. And lithium stands out as the monotherapy in the largest numbers. Everybody else seems to need combinations of treatment to be okay in the community. Another advantage of lithium, no evidence that it's inferior to the SGAs for psychotic mania. And in one study, it was actually better than valproate for psychotic mania.
References:
- Baldessarini, R. J., Leahy, L., Arcona, S., Gause, D., Zhang, W., & Hennen, J. (2007). Patterns of psychotropic drug prescription for U.S. patients with diagnoses of bipolar disorders. Psychiatric Services (Washington, D.C.), 58(1), 85–91.
- Swann, A. (2002). Pattern of response to Divalproex, lithium, or placebo in four naturalistic subtypes of mania. Neuropsychopharmacology, 26(4), 530-536.
Slide 6 of 20
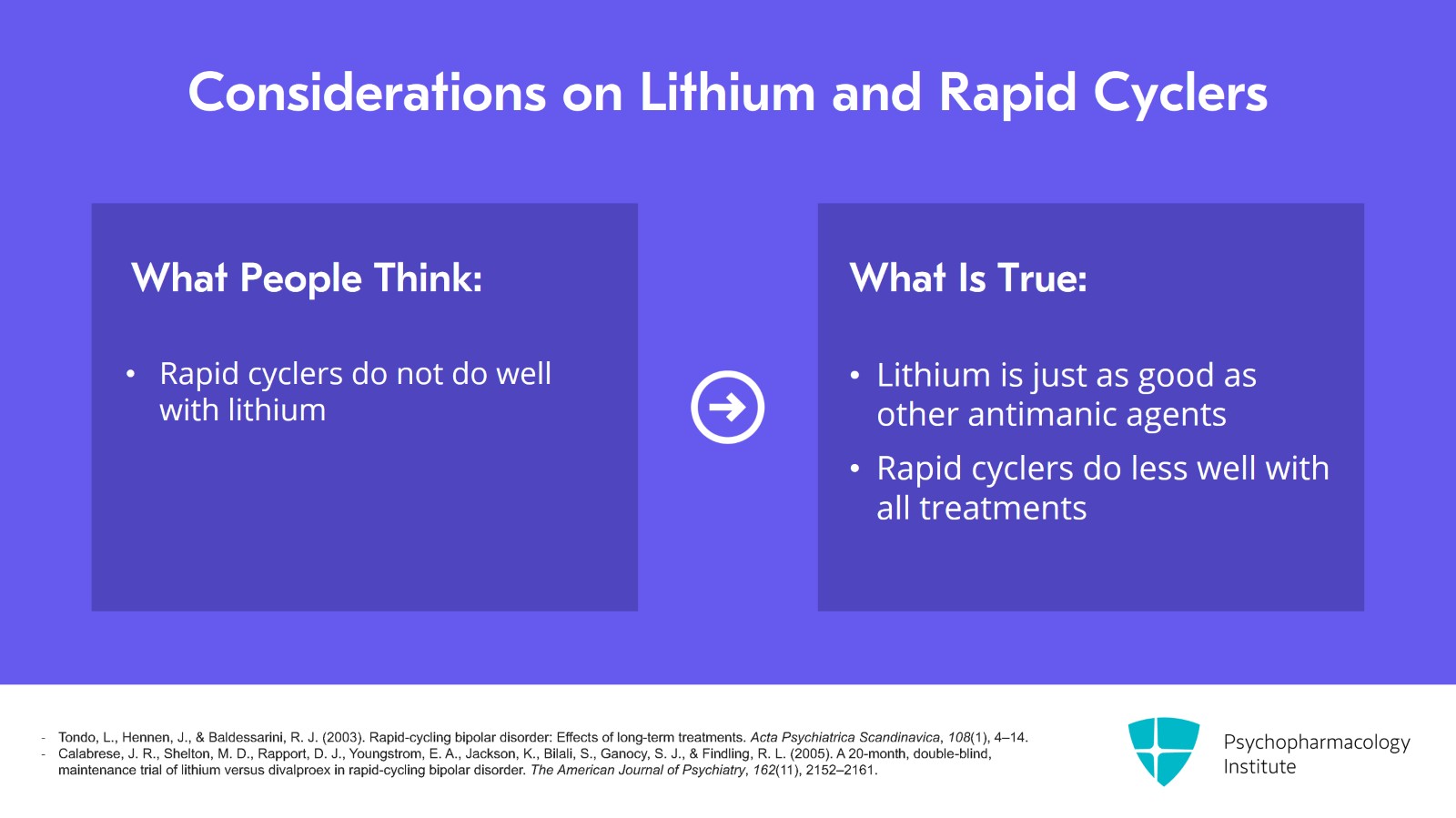
And by the way, some people have the opinion that rapid cyclers don't do so well in lithium. Well, it's just false. Lithium is just as good as the other antimanic agents for rapid cyclers. Several reviews of the literature concluded that. Now, all people do less well when they're rapid cyclers. Lithium is just not any worse than the others. They all don't work as all. Rapid cycling is a tough problem and our treatments don't work as well for it. But I do recommend strongly getting them off antidepressants. That makes rapid cycling, it causes it and makes it worse. All right. So first choice is lithium.
References:
- Tondo, L., Hennen, J., & Baldessarini, R. J. (2003). Rapid-cycling bipolar disorder: Effects of long-term treatments. Acta Psychiatrica Scandinavica, 108(1), 4–14.
- Calabrese, J. R., Shelton, M. D., Rapport, D. J., Youngstrom, E. A., Jackson, K., Bilali, S., Ganocy, S. J., & Findling, R. L. (2005). A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. The American Journal of Psychiatry, 162(11), 2152–2161.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 20
Now, what about the second-generation antipsychotics? Risperidone and olanzapine have good efficacy. The standardized mean difference from placebo in that meta-analysis for nonmixed mania was 0.5 as I mentioned earlier, olanzapine 0.42 but neither has evidence of efficacy for depressive symptoms in bipolar depression or mixed mania. So given the priority we place on that ability, they are ranked lower.
References:
- Cipriani, A., Barbui, C., Salanti, G., Rendell, J., Brown, R., Stockton, S., Purgato, M., Spineli, L. M., Goodwin, G. M., & Geddes, J. R. (2011). Comparative efficacy and acceptability of antimanic drugs in acute mania: A multiple-treatments meta-analysis. The Lancet, 378(9799), 1306-1315.
Slide 8 of 20
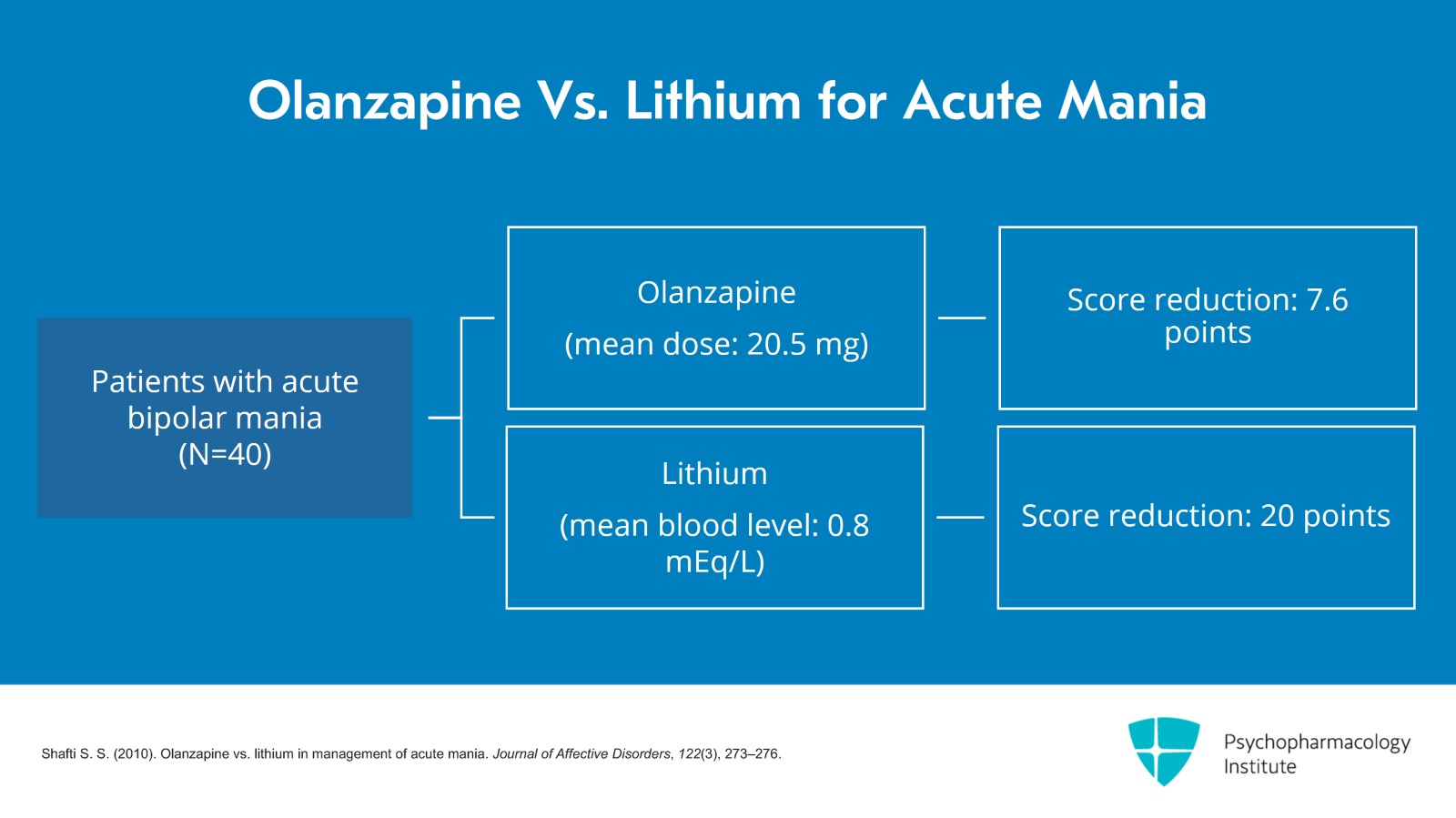
Now, what about olanzapine? Olanzapine is still popular for acute mania. How does it compare with lithium in acute mania? You may want to know. What's the evidence? Well, I will propose that you have a look at this study by Shafti et al. of olanzapine versus lithium in acute bipolar mania published in the Journal of Affective Disorders, 2010. It was a small study, 40 patients, all women and it was a three-week study like most manic studies are, using the Manic State Rating Scale. The severity of mania reduction was the outcome measure. And with lithium at a mean blood level of 0.8 mEq/L reduced the score by 20 points. Whereas, olanzapine at a mean dose of 20.5 mg, so in other words both the lithium and although the olanzapine were robustly dosed, the mean reduction on olanzapine was 7.6 points versus the 20 points on lithium. That was statistically significant at a 0.0002 level. Anyone believe that study listening to this lecture? Anyone believe that lithium could have been so much better than olanzapine when they were compared head-to-head in these women with mania?
References:
- Shafti S. S. (2010). Olanzapine vs. lithium in management of acute mania. Journal of Affective Disorders, 122(3), 273–276.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 20
Well, for completeness, let's mention that there were two other studies of lithium versus olanzapine. In one of them, the olanzapine beat lithium. And in the third one, olanzapine had exactly the same results as lithium. So if we take all three studies, it looks like they're about the same. So that's why we argue that they are the same.
References:
- Chengappa, K. N., Baker, R. W., Shao, L., Yatham, L. N., Tohen, M., Gershon, S., & Kupfer, D. J. (2003). Rates of response, euthymia and remission in two placebo-controlled olanzapine trials for bipolar mania. Bipolar Disorders, 5(1), 1–5.
Slide 10 of 20
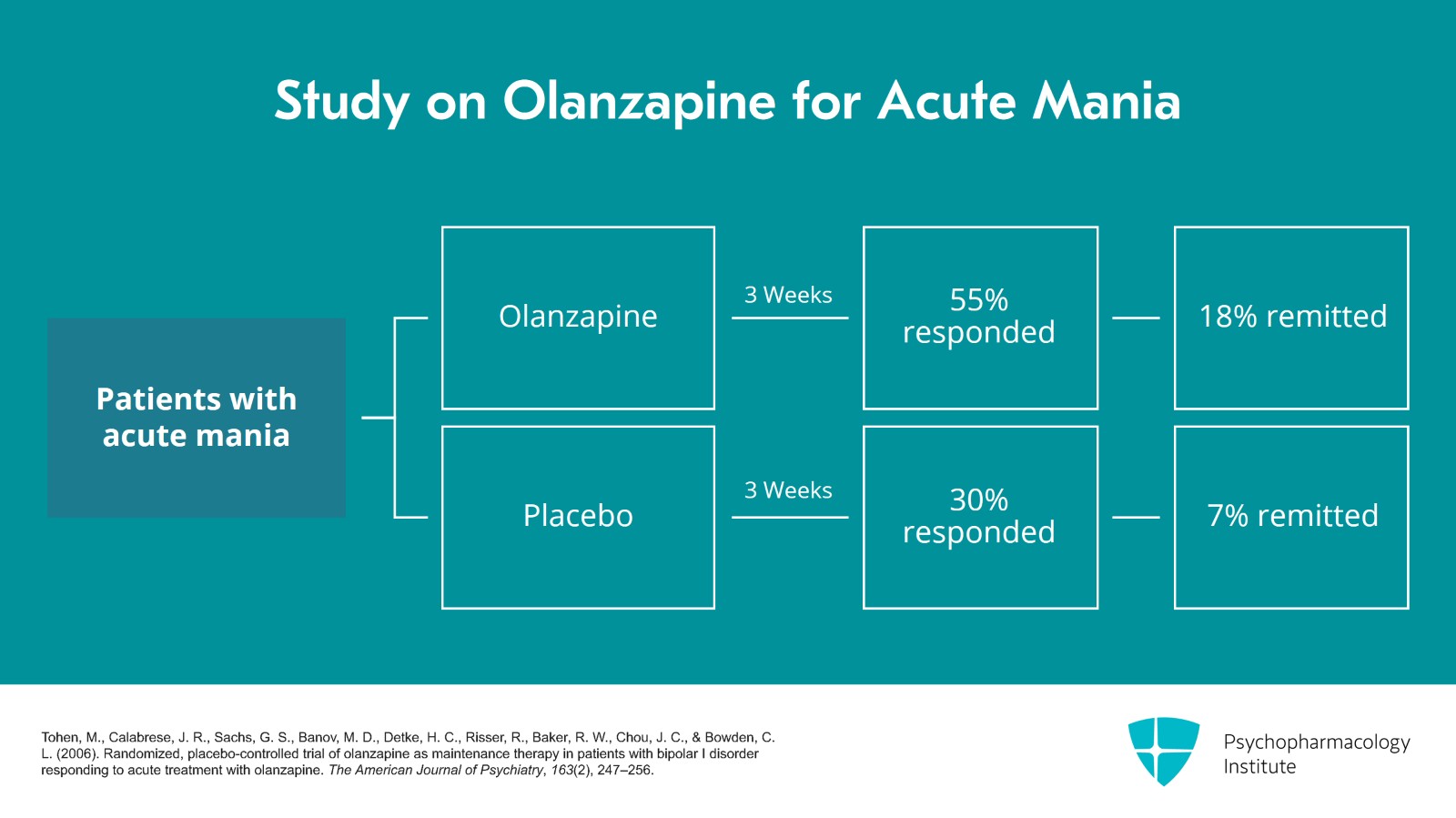
Now, I also would like to go over a little data on how well does olanzapine work for the olanzapine lovers out there. What is the evidence of how effective it is versus placebo? So in a pooled analysis of several studies of olanzapine for acute mania versus placebo, I have the results shown here, the response after three weeks which is your, again your typical endpoint for mania studies, the percentage of patients who responded, response was defined as greater than a 50% improvement in the Young Mania Rating Scale, 55% responded to olanzapine after three weeks versus placebo 30% responded. Okay. So it was better than placebo but it wasn't a fantastic result. We only have 55% responding after three weeks. And if you want to know how many remitted after three weeks, defined as a Young Mania Rating Scale of less than 7, only 18% remitted on olanzapine after three weeks versus 7% on placebo. So this belief in olanzapine as some kind of fantastic treatment is not supported by evidence. Placebo also works in a significant number of people.
References:
- Tohen, M., Calabrese, J. R., Sachs, G. S., Banov, M. D., Detke, H. C., Risser, R., Baker, R. W., Chou, J. C., & Bowden, C. L. (2006). Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. The American Journal of Psychiatry, 163(2), 247–256.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 20
Now, what about other SGAs other than olanzapine. We have aripiprazole, paliperidone and asenapine. Asenapine did have some efficacy in mania but lower effect size versus placebo than the others we have already discussed. None have efficacy for bipolar depression, none of those. So that's why we don't like to use them for classic mania. They're ranked lower than risperidone, olanzapine, or lithium.
References:
- Cipriani, A., Barbui, C., Salanti, G., Rendell, J., Brown, R., Stockton, S., Purgato, M., Spineli, L. M., Goodwin, G. M., & Geddes, J. R. (2011). Comparative efficacy and acceptability of antimanic drugs in acute mania: A multiple-treatments meta-analysis. The Lancet, 378(9799), 1306-1315.
Slide 12 of 20
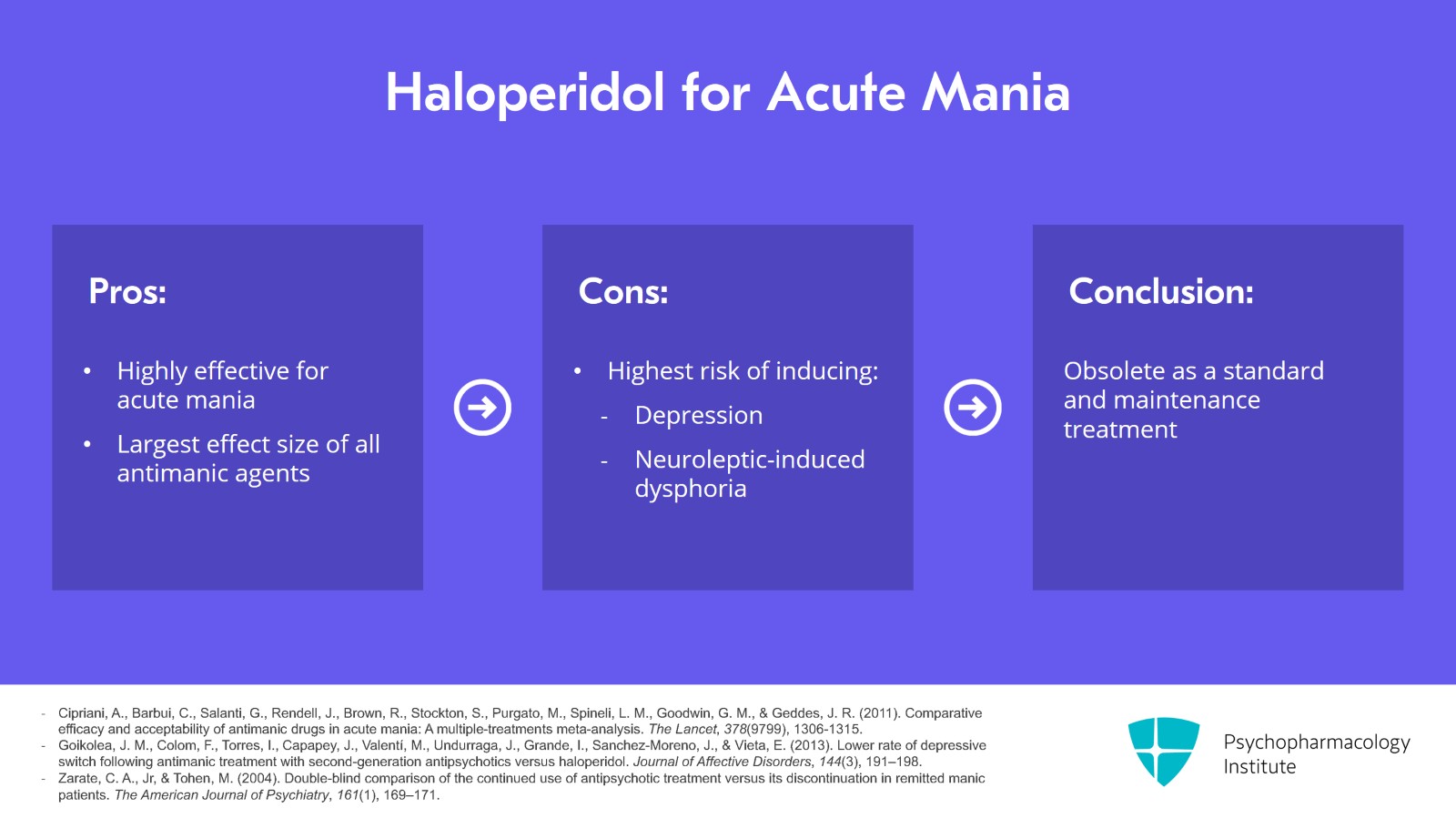
Now, what about haloperidol? You may wonder why we don't have that anywhere. You haven't seen it at all so far in our algorithms for mania. Well, it is highly effective for acute mania. In that same meta-analysis, it had the largest effect size of all antimanic agents of 0.56 putting it larger than the risperidone which is 0.5. It's 56% better than placebo rather than 50% better than placebo which is what we had with risperidone. It was the best. So but why is haloperidol unacceptable despite having the highest efficacy for acute mania? Because haloperidol has the highest risk of inducing depression and another similar related problem, neuroleptic-induced dysphoria versus all other antimanic agents. And those are the last things we want. We are willing to give up a little bit of efficacy to not have the patient switching into mania and hating that dysphoria side effect of being on haloperidol and stopping their meds right away which happens so often with haloperidol. So we think it's obsolete as a treatment, as a treatment to use as your standard treatment and to maintain people.
References:
- Cipriani, A., Barbui, C., Salanti, G., Rendell, J., Brown, R., Stockton, S., Purgato, M., Spineli, L. M., Goodwin, G. M., & Geddes, J. R. (2011). Comparative efficacy and acceptability of antimanic drugs in acute mania: A multiple-treatments meta-analysis. The Lancet, 378(9799), 1306-1315.
- Goikolea, J. M., Colom, F., Torres, I., Capapey, J., Valentí, M., Undurraga, J., Grande, I., Sanchez-Moreno, J., & Vieta, E. (2013). Lower rate of depressive switch following antimanic treatment with second-generation antipsychotics versus haloperidol. Journal of Affective Disorders, 144(3), 191–198.
- Zarate, C. A., Jr, & Tohen, M. (2004). Double-blind comparison of the continued use of antipsychotic treatment versus its discontinuation in remitted manic patients. The American Journal of Psychiatry, 161(1), 169–171.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 20
We could use it acutely briefly for IM use to quell a very severe agitated manic patient but not as a treatment to continue for treating the mania.
References:
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 14 of 20
Now, I want to say a few more words about why we don't have valproate first line. Why have we demoted it? First of all, we recommend against valproate for first-line use because of inferior acute efficacy. Valproate also has minimal quality evidence of efficacy for maintenance of mania and it's not FDA approved for maintenance for mania or depression.
References:
- Tamayo, J. M., Zarate, C. A., Jr, Vieta, E., Vázquez, G., & Tohen, M. (2010). Level of response and safety of pharmacological monotherapy in the treatment of acute bipolar I disorder phases: A systematic review and meta-analysis. The International Journal of Neuropsychopharmacology, 13(6), 813–832.
- Yee, C. S., Vázquez, G. H., Hawken, E. R., Biorac, A., Tondo, L., & Baldessarini, R. J. (2021). Long-term treatment of bipolar disorder with valproate: Updated systematic review and meta-analyses. Harvard Review of Psychiatry, 29(3), 188–195.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 20
Weight gain is more on valproate than lithium in head-to-head trials. Now, we do have some small inadequate studies in acute depression. I do want to point that out. It's not totally lacking in studies but they're small and of poor quality.
References:
- Bowden, C. L., Brugger, A. M., Swann, A. C., Calabrese, J. R., Janicak, P. G., Petty, F., Dilsaver, S. C., Davis, J. M., Rush, A. J., & Small, J. G. (1994). Efficacy of divalproex vs lithium and placebo in the treatment of mania. The Depakote Mania Study Group. JAMA, 271(12), 918–924.
- Osser, D. (2021). Psychopharmacology algorithms. Wolters Kluwer.
Slide 16 of 20
So to conclude video 5, the key points, lithium is the first-line recommended treatment for acute classic mania. It may not have a better effect size than some antipsychotics but it uniquely has efficacy and FDA approval for preventing future manias and depressions.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 20
Now, of all the SGAs, quetiapine comes closest to being competitive as a first-line choice with lithium. It also has a smaller effect size than some other antipsychotics but it has strong efficacy as a treatment for bipolar depression which in our view considerably adds to its advantages over other SGAs.
Slide 18 of 20
Other SGAs are effective, some with high efficacy like risperidone which is higher than olanzapine but also pretty high. But they are not effective for treating or preventing depressions.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 20
Other SGAs are effective, some with high efficacy like risperidone which is higher than olanzapine but also pretty high. But they are not effective for treating or preventing depressions.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.