Text version
New International Schizophrenia Guidelines Published
In this Quick Take today, I am basically going to make you aware that a new schizophrenia guideline was just published. It appeared in the Lancet Psychiatry in March of 2025.
The title of the publication is “INTEGRATE: international guidelines for the algorithmic treatment of schizophrenia”. These guidelines were developed by a large group of psychiatrists from 30 countries. It covered all UN regions, so it is truly an international effort.
I need to add a disclaimer here. I was one of the members of the INTEGRATE Advisory Group that participated in the guideline process. This involved, among other things, an umbrella review to develop a survey. That survey was then used to achieve consensus among invited experts worldwide, with feedback from focus groups, including people with lived experience.
Download PDF and other files
Why New Schizophrenia Guidelines Were Needed
Now, you should ask, did we really need a new schizophrenia guideline? I think the answer is yes. Many existing guidelines are either outdated or confusing.
In contrast, the INTEGRATE guidelines represent a nice summary of what we would currently consider high-quality schizophrenia care. This applies to any country, and they’re presented in an algorithm any clinician could easily follow. Having authoritative international consensus guidelines represents an important step in reducing variability in schizophrenia care.
And you may think, variability, what’s wrong with that? Well, variability in Medicine can be a sign of substandard care. Let me explain:
- For example, there is no reason why clozapine utilization for treatment-resistant schizophrenia varies between Germany, the United States, South Korea or Nigeria or within regions in a country.
- It is simply a problem of not using clozapine appropriately as clozapine is the treatment of choice for any patient with treatment-resistant schizophrenia regardless of where the patient lives.
- Having one guideline that is universal may be a good first step at least towards optimal schizophrenia care for all.
Strengths and Assumptions of INTEGRATE Algorithm
I would say the strength of these guidelines is that they are dynamic and flexible enough to allow for patient-centered care but that they are not too complex. They provide clinicians with an algorithm that they can actually follow.
If every clinician just follows the proposed algorithm, we would greatly increase the quality of care across all patients with schizophrenia.
As for the guidelines themselves, they make several basic assumptions:
- Shared decision making is key
- Acting early if a patient is not improving
- Focusing on medication side effects as an integral part of treatment decisions
Download PDF and other files
First-Episode Psychosis Recommendations
Let me walk you through the algorithm for a first-episode psychosis patient:
- Start with Aripiprazole (if no preference) Begin with aripiprazole, 5 mg/day, and titrate based on response.
- Use Long-Acting Injectables Early LAIs should be considered early, not just for poor adherence. After establishing tolerability and efficacy with oral meds, offer to switch to a long-acting formulation—even in first-episode patients.
- Consider Discontinuation in Select Cases If a patient achieves full remission, the guidelines suggest discussing a slow discontinuation of antipsychotics over six months, after two years of treatment.
- Introduce Clozapine Promptly When Indicated Clozapine should be offered as early as 12 weeks into treatment, after two unsuccessful trials of antipsychotics.
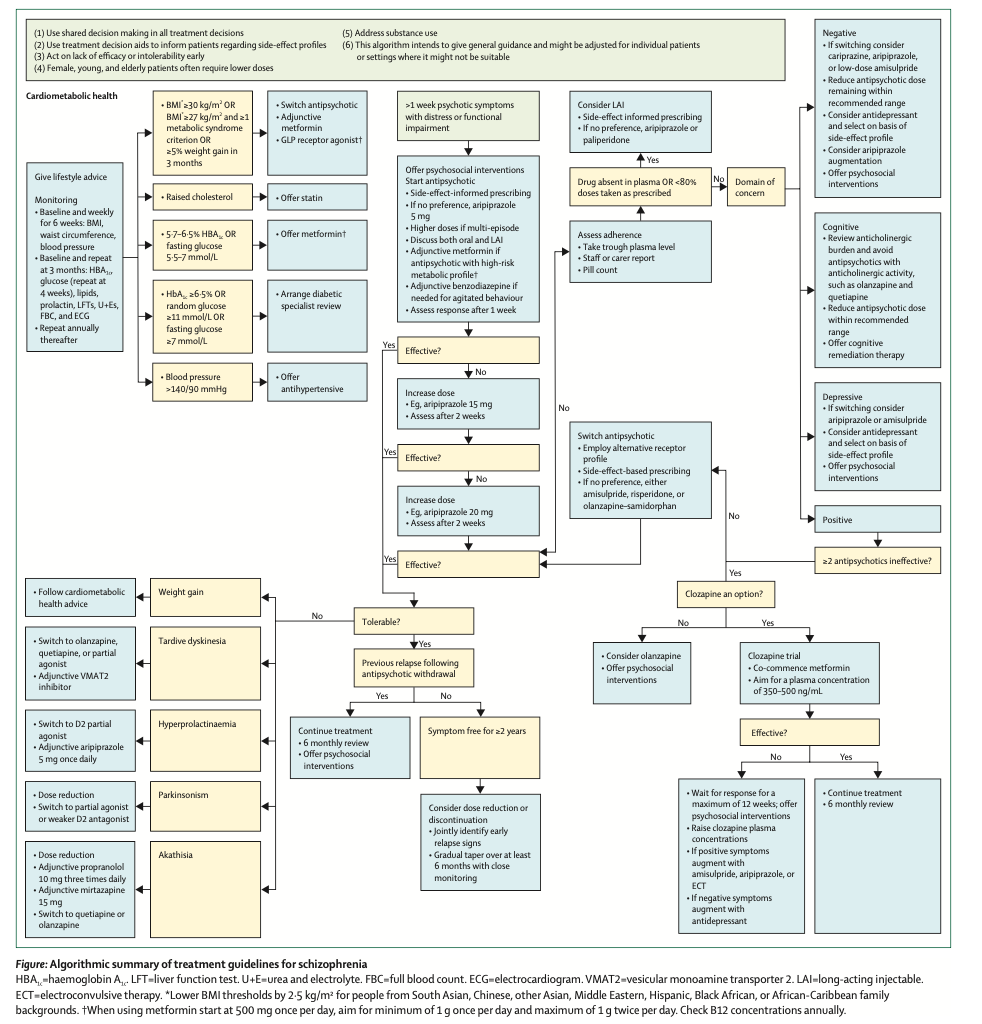
An algorithmic summary of the treatment guidelines. Right click to download the image.
Medical Management Recommendations
The guidelines also include medical management recommendations, such as using metformin routinely if prescribing a metabolically high-risk antipsychotic. If you implement these recommendations, you’ll be offering excellent care to your first-episode patients.
Download PDF and other files
Limitations of the Guidelines
There are some shortcomings to note:
- The guidelines are limited to psychopharmacology which represents an important pillar of schizophrenia care but it is insufficient treatment by itself without psychosocial supports and rehabilitation.
- The guidelines could also not weigh the role of the new non-dopaminergic antipsychotic, xanomeline plus trospium, which was just approved in the United States.
- They also don’t address the role of GLP agonists for weight management.
Bottom Line: Uniform, Practical Guidelines
This is my bottom line for today. The field now has uniform, not-country-specific, universal, practical guidelines for the pharmacological management of schizophrenia. They are going to be current for at least a few years, with the plan to update them regularly.
I think these guidelines are an important step. They help establish what good pharmacological treatment for patients with schizophrenia ought to look like.
I encourage you to go to the publication and look at the algorithm that summarizes the guidelines. Apply them to your own practice. And please, please also post this algorithm in your clinic. It’s a great teaching tool to educate your patients. Also, if you work with trainees, nurse practitioners, or residents, it’s great to teach them how to apply optimal care for this patient group.
Download PDF and other files
Abstract
INTEGRATE: international guidelines for the algorithmic treatment of schizophrenia
Robert A McCutcheon, Ph.D.; Toby Pillinger, Ph.D.; ∙ Ioana Varvari, MRCPsych; Sean Halstead, M.D.; Olatunde O Ayinde, MS; Nicolás A Crossley, Ph.D.; et al.
Summary
Schizophrenia is a mental illness involving multiple symptom domains and is often associated with substantial physical health comorbidities. Guidelines exist, but these tend to be country-specific and are often missing a concise yet comprehensive algorithmic approach. From May 1, 2023, to Jan 1, 2025, International Guidelines for Algorithmic Treatment (INTEGRATE) authors from all UN regions collaborated to develop a consensus guideline focused on the pharmacological treatment of schizophrenia. Following an umbrella review of the literature, input from expert workshops, a consensus survey, and lived experience focus groups, a consensus algorithmic guideline and associated digital tool were developed. Key recommendations include a focus on metabolic health from treatment initiation, timely assessment and management of non-response, symptom domain-specific interventions, mitigation of side-effects, and the prompt use of clozapine in cases of treatment resistance.
Reference
McCutcheon, R. Ph.D.; Pillinger, T. Ph.D.; Varvari, I. MRCPsych; Halstead, S. M.D.; Ayinde, O. MS; Crossley, N. Ph.D.; et al. (2025). INTEGRATE: international guidelines for the algorithmic treatment of schizophrenia. The Lancet Psychiatry, Volume 12, Issue 5, 384 – 394.



