I wanted to say something about experimental pharmacological treatments. One aspect of psychiatric research that’s slow for the moment is that there aren’t many new drugs coming through the usual discovery pathways. That’s via industry.
There has been more of a focus on repurposing pharmacological treatments that are available anyway, which then can be rapidly repurposed for their use in patients with treatment-resistant depression.
I will just start by talking about anti-inflammatory agents.
And it has been known for some time that patients with depression particularly resistant depression have peripheral markers of inflammation,

for example, increased levels of C-reactive protein (CRP), the interleukin-6 (IL-6) and tumor necrosis factor.
More directly, we know that when patients who aren’t depressed receive inflammatory cytokines such as interferon, they have a high risk of experiencing the symptoms of major depression subsequently.

This raises the idea that perhaps drugs that have an anti-inflammatory effect might be useful to treat depression particularly resistant depressed patients,

particularly those depressed patients who have evidence of inflammatory markers in their peripheral blood tests.
I would like to mention the study which employed two conventional antidepressants first. This was an investigation that randomized a large number of patients with depression
to either the serotonergic agent, escitalopram or the noradrenergic agent, the tricyclic nortriptyline.
And what they also found was that overall there was no difference in outcome between the two drugs.
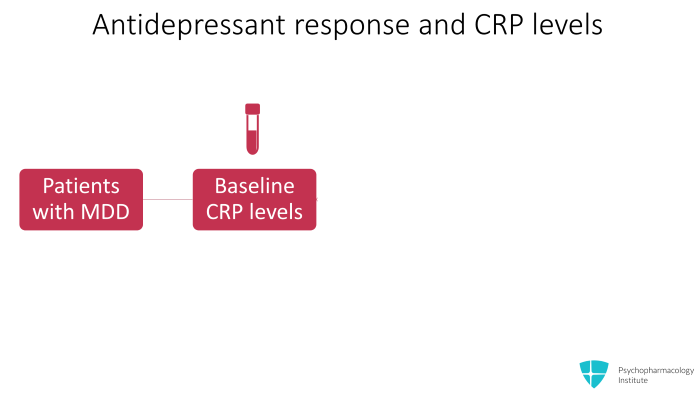
However, if you split the patients according to their baseline levels of C-reactive protein (CRP), then there did seem to be a differential response.
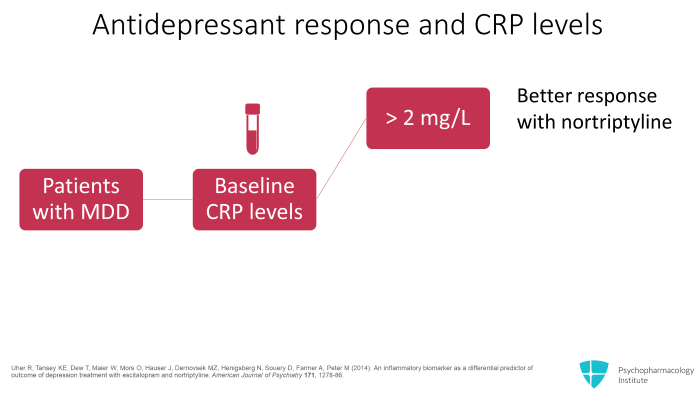
Patients who had CRP levels above 2 mg/L did rather better with nortriptyline than with the escitalopram.
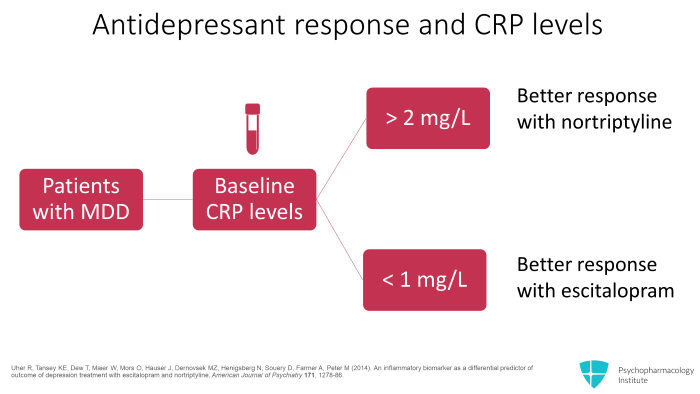
However, the converse was the case for patients with low levels of CRP of less than 1. They did better with escitalopram than they did with nortriptyline.
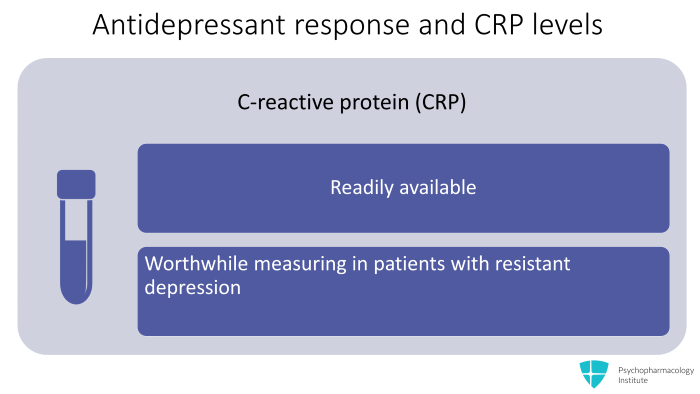
Because CRP is a readily available laboratory test, it might be worthwhile measuring in patients with resistant depression
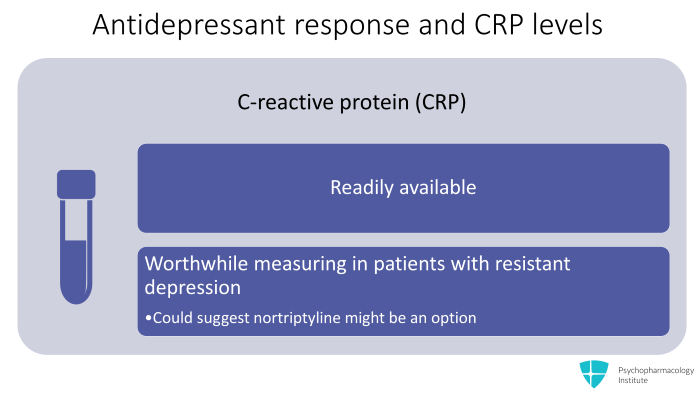
because it suggests that perhaps if it is raised, nortriptyline might be an option.
Of course, the evidence for inflammation in patients with resistant depression also suggests that there might be a role for specific anti-inflammatory treatments in improving depressive symptomatology.
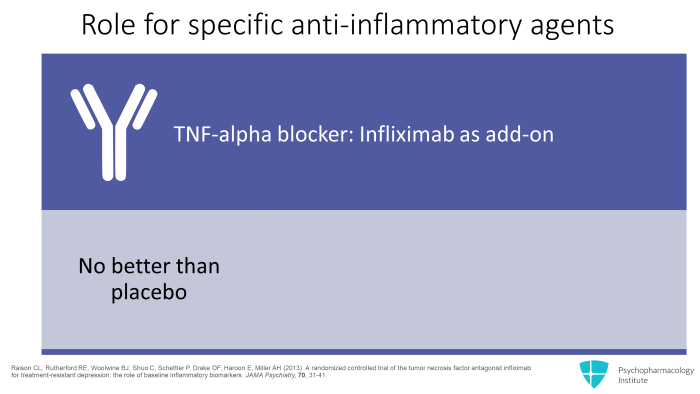
There is one trial with a TNF-alpha blocker, infliximab, which was added to the medication of treatment with resistant depression. In general, this didn’t seem to do better than placebo in the overall group of patients.
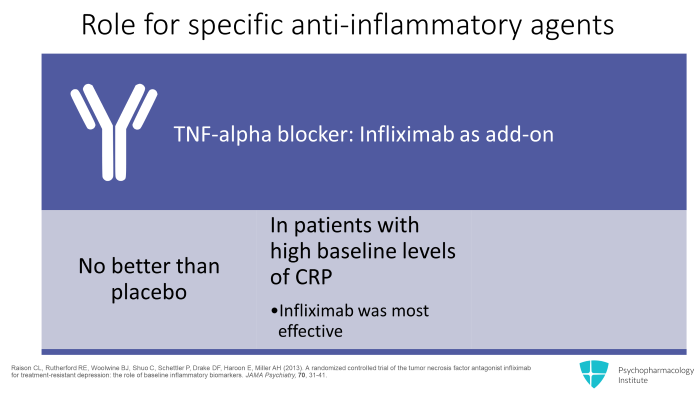
But in those patients who had high baseline levels of CRP suggesting evidence of inflammation, infliximab was most effective.
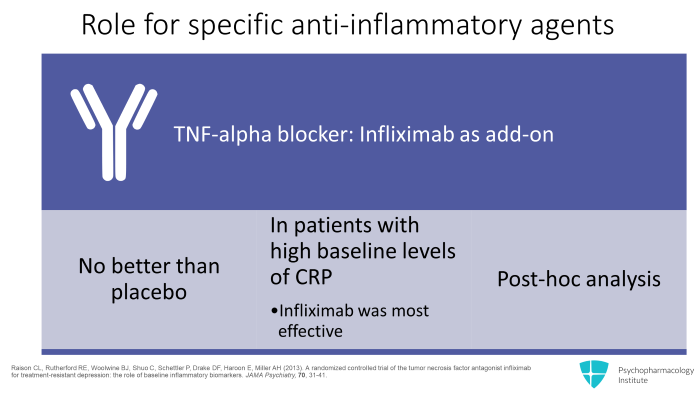
It is important to note though that this was a post-hoc analysis and so it will be important for this sort of study to be replicated prospectively.
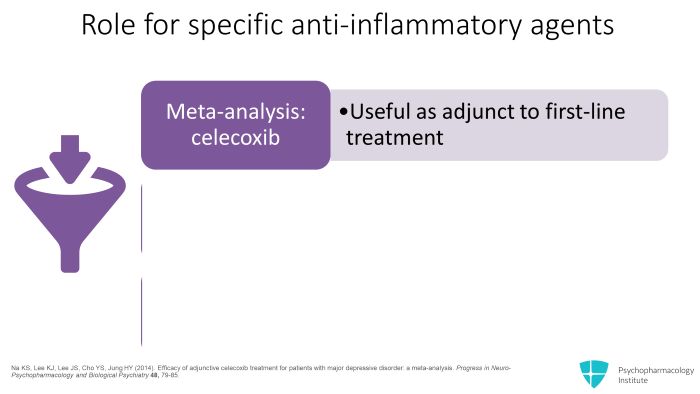
There is very little else from the point of view of specific experimental pharmacological studies but there was a meta-analysis which suggests that the COX-2 inhibitor drug, celecoxib is a useful adjunct to the first line treatment of major depression with either serotonergic or noradrenergic and antidepressants.
In terms of one’s practice, I think the evidence for using drugs such as NSAIDs isn’t clear whether that would be helpful.

Possibly, celecoxib is worth trying if one is aware of the various medical contraindications and side effects that might be associated with its use.
The key points I made there is that inflammatory processes may play an important role in depression particularly in patients who have resistant depression that doesn’t respond to conventional pharmacological treatments.
And a meta-analysis suggests that the COX-2 drug, celecoxib might be helpful as an adjunct to first-line treatment in serotonergic and noradrenergic antidepressants
but it hasn’t been systematically studied yet in patients with treatment-resistant depression.
References
- Raison CL, Miller AH (2011). Is depression an inflammatory disorder? Current Psychiatry Reports 13, 467-75.
- Udina M, Castellví P, Moreno-España J, Navinés R, Valdés M, Forns X, Langohr K, Solà R, Vieta E, Martín-Santos R (2012). Interferon-induced depression in chronic hepatitis C: a systematic review and meta-analysis . Journal of Clinical Psychiatry, 73, 1128-38.
- Uher R, Tansey KE, Dew T, Maier W, Mors O, Hauser J, Dernovsek MZ, Henigsberg N, Souery D, Farmer A, Peter M (2014). An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline . American Journal of Psychiatry 171, 1278-86.
- Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, Haroon E, Miller AH (2013). A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers . JAMA Psychiatry, 70, 31-41.
- Na KS, Lee KJ, Lee JS, Cho YS, Jung HY (2014). Efficacy of adjunctive celecoxib treatment for patients with major depressive disorder: a meta-analysis. Progress in Neuro-Psychopharmacology and Biological Psychiatry 48, 79-85.



