Slides and Transcript
Slide 2 of 11
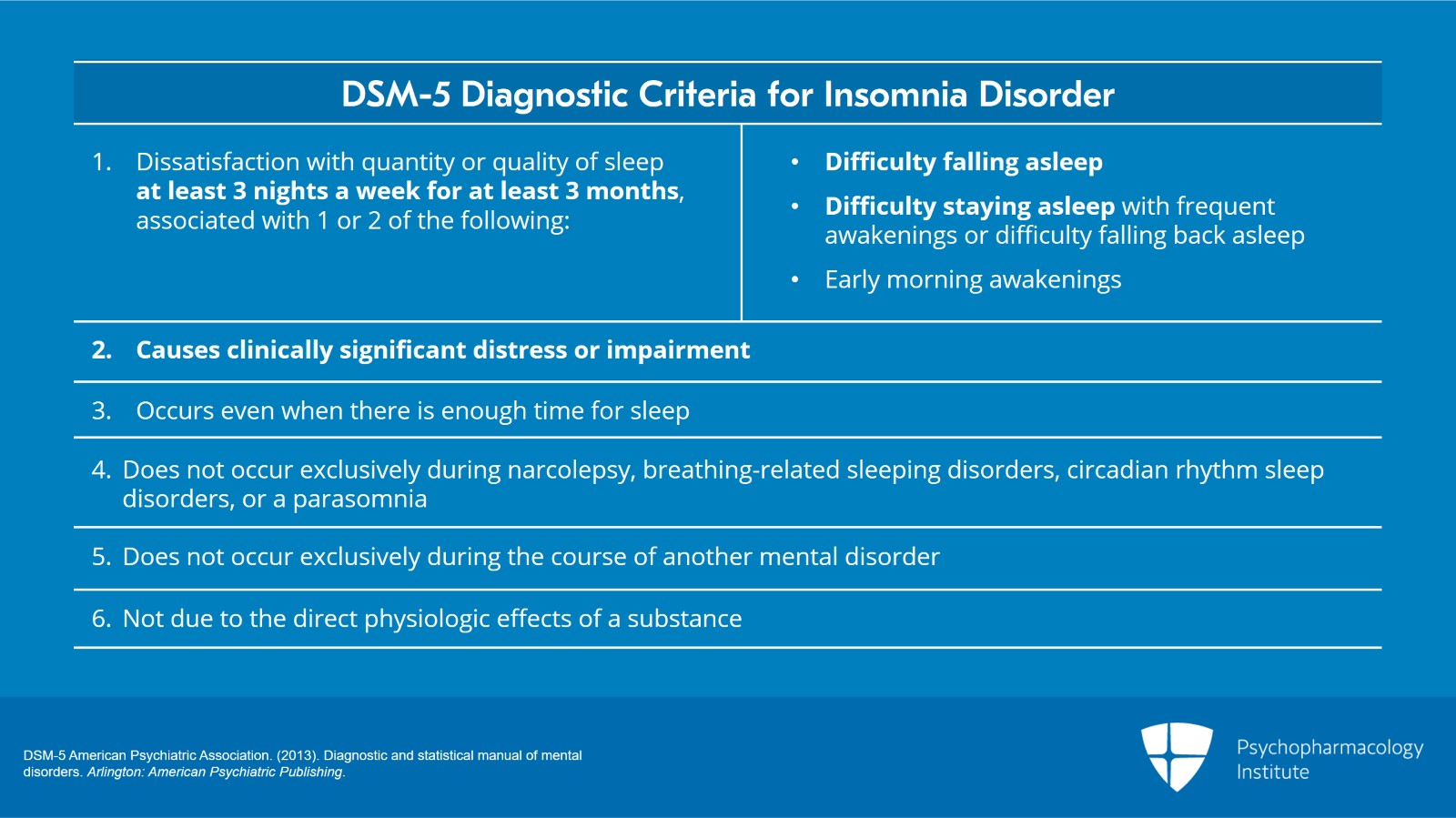
When you review the DSM-5 chapter on sleep-wake disorders, you'll see the diagnostic criteria for insomnia disorder that specify that the patient's complaints of difficulty falling or staying asleep typically occur three times a week or longer, have lasted three months or longer and are associated with daytime distress and impairment.
References:
- DSM-5 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. Arlington: American Psychiatric Publishing.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 11
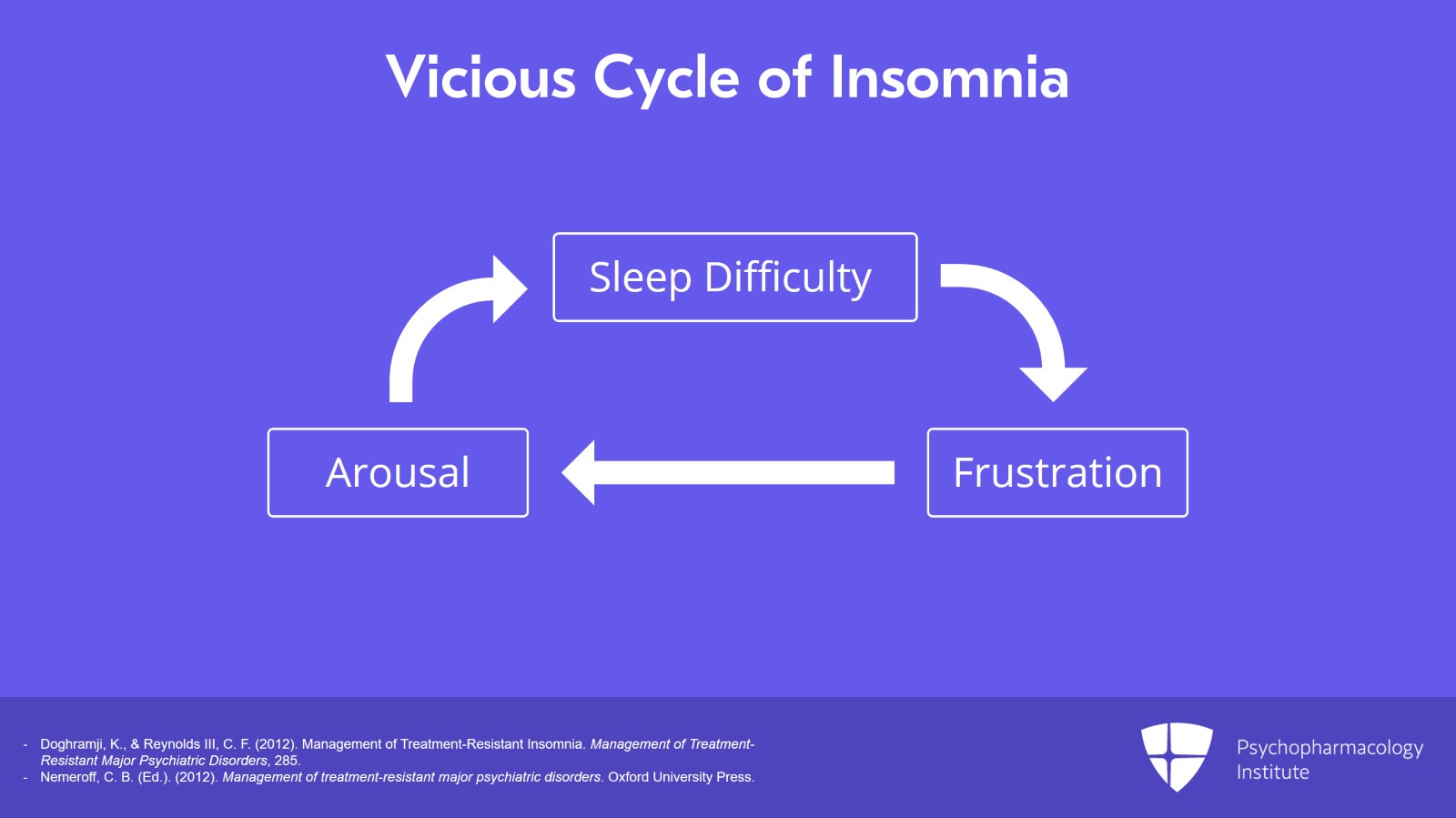
At the core of what we're doing is the vicious cycle displayed here, sleep difficulties leading to frustration to more arousal to further sleep difficulty. And ultimately, by means of our workup and intervention, we want to substitute a virtuous cycle for the vicious cycle depicted here.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285.
- Nemeroff, C. B. (Ed.). (2012). Management of treatment-resistant major psychiatric disorders. Oxford University Press.
Slide 4 of 11
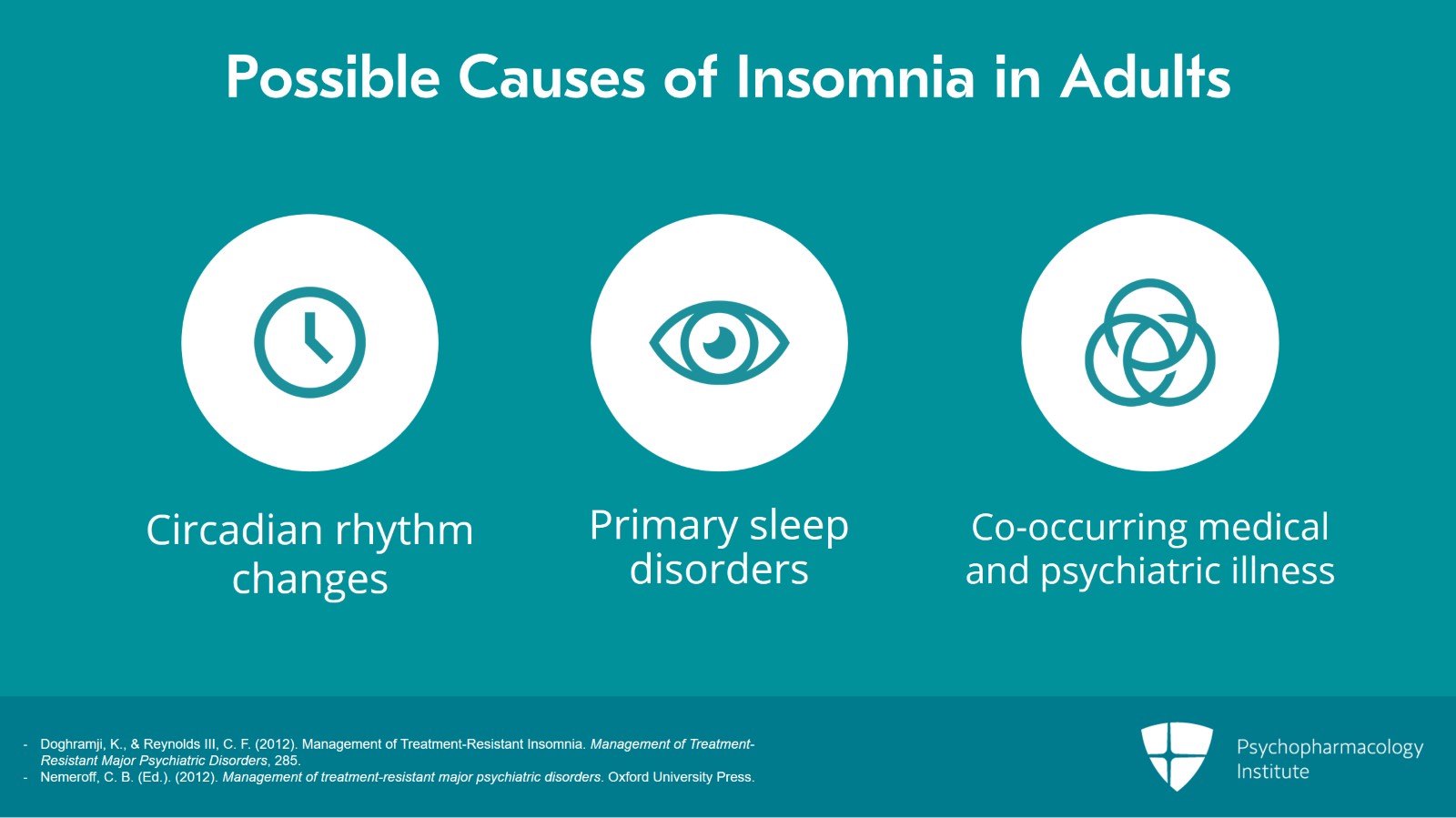
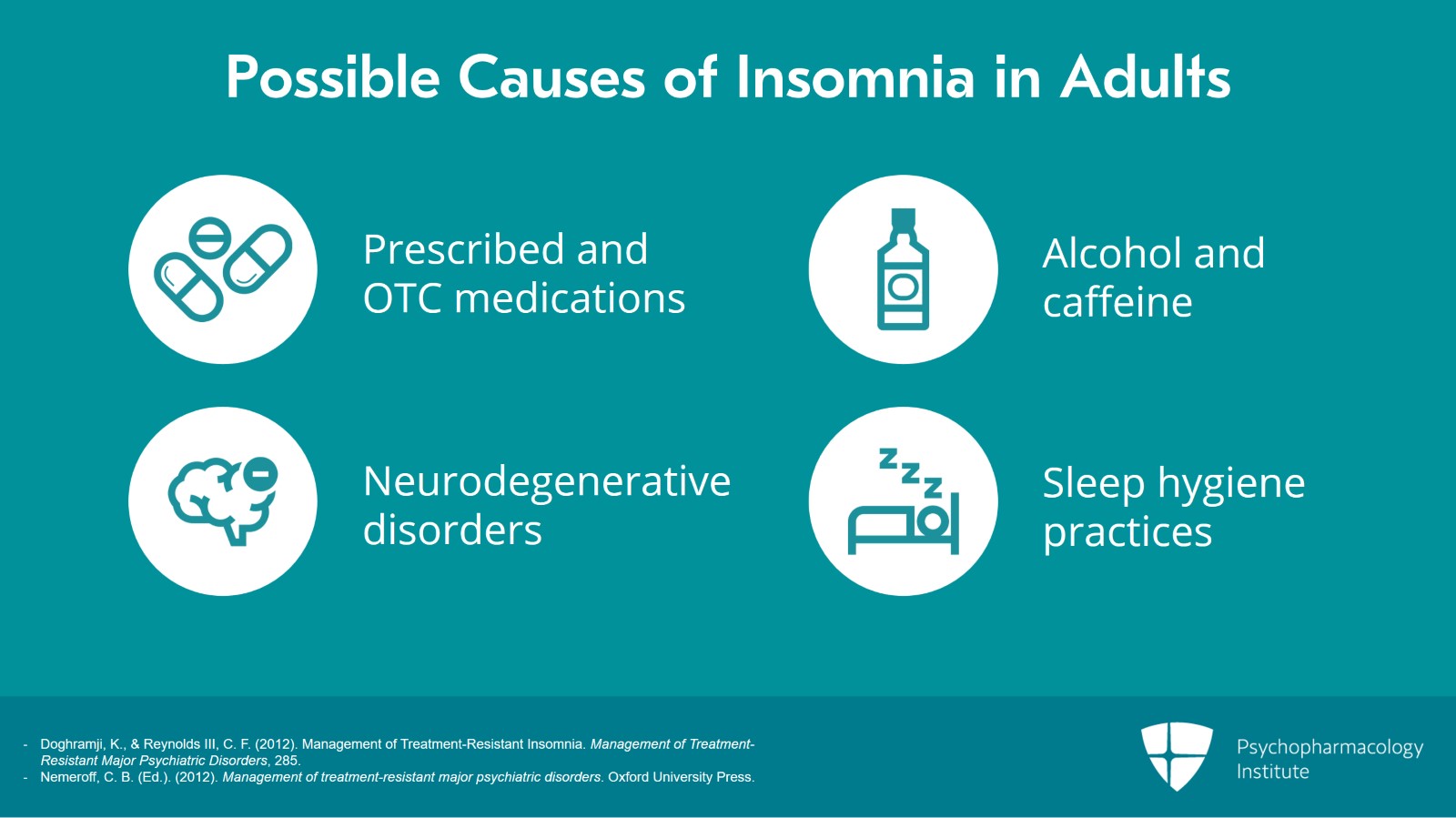
As part of the workup, consider possible causes of insomnia disorder in adults. Be mindful that the differential diagnoses include circadian rhythm changes whether delayed or advanced sleep phase syndromes, primary sleep disorders and of particular importance co-occurring medical and psychiatric illness.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285
- Nemeroff, C. B. (Ed.). (2012). Management of treatment-resistant major psychiatric disorders. Oxford University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 11
prescribed and over-the-counter medications and self-treatment with things like alcohol and caffeine. In older adults, also consider the possibility of a neurodegenerative disorder. Part of the history and evaluation also includes a review of sleep hygiene practices. Does the patient engage in practices that promote sleep or destroy sleep? We'll talk more about that later in the context of brief behavioral treatment for insomnia.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285
- Nemeroff, C. B. (Ed.). (2012). Management of treatment-resistant major psychiatric disorders. Oxford University Press.
Slide 6 of 11
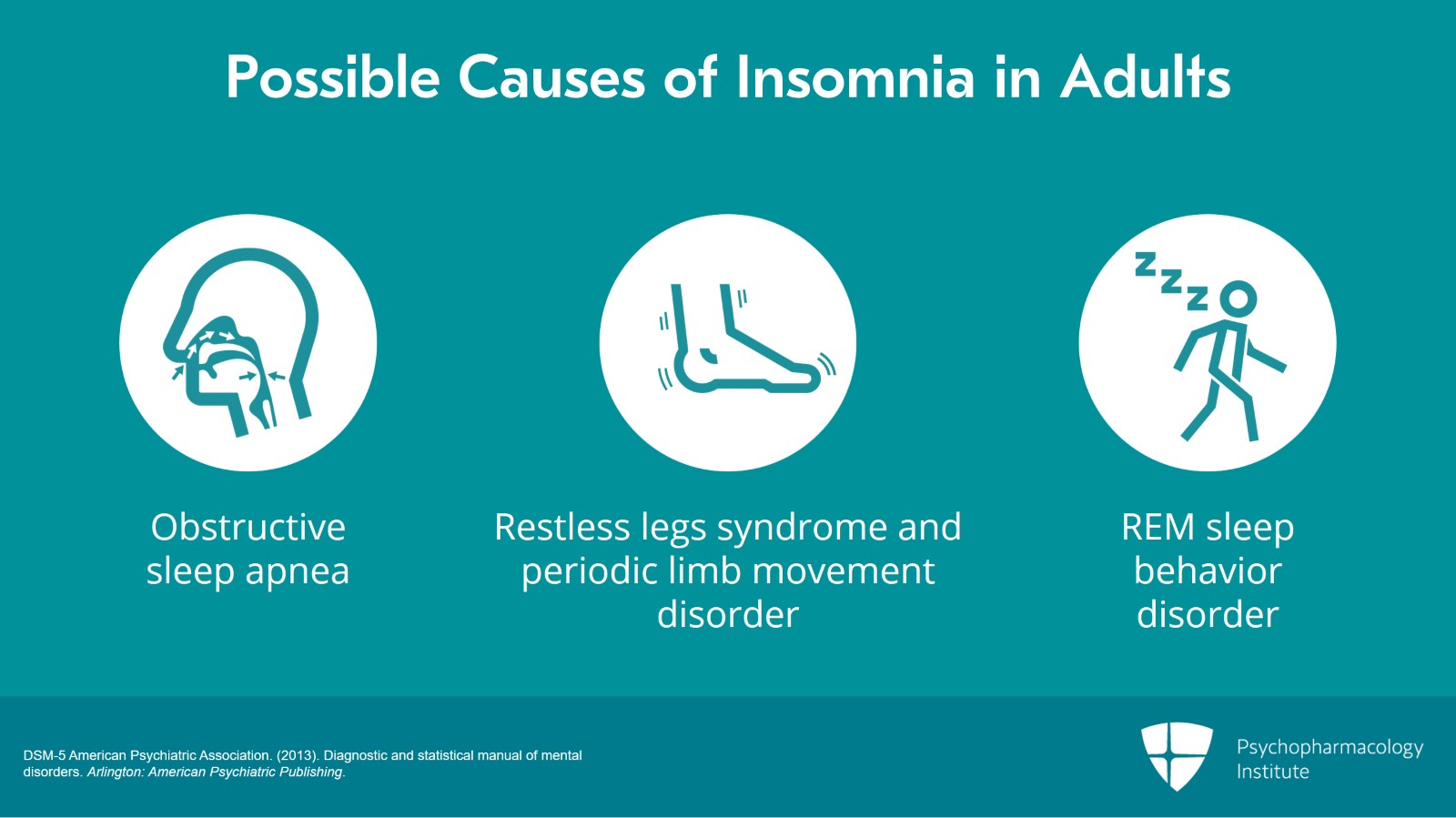
Consider as part of the differential diagnoses such primary sleep disorders as obstructive sleep apnea, for example, what we saw in Chip's case in the earlier tape and other issues like restless legs syndrome, periodic limb movement disorders and REM sleep behavior disorders. All of these are described with their diagnostic criteria in the DSM-5 chapter on sleep-wake disorders.
References:
- DSM-5 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. Arlington: American Psychiatric Publishing.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 11
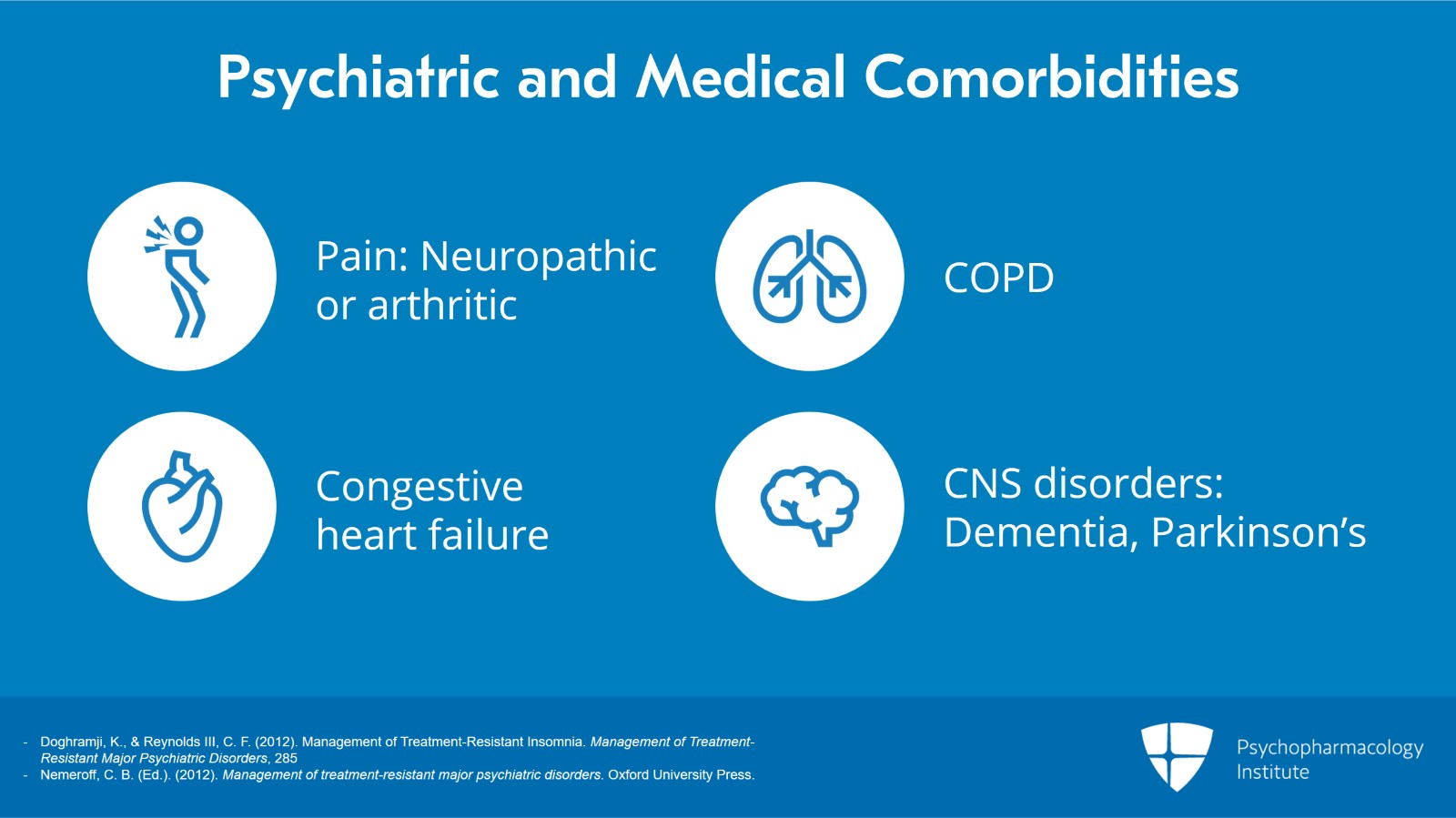
An important part of the evaluation also addresses psychiatric and medical comorbidities, for example, pain related to neuropathy or arthritis, congestive heart failure, COPD and other issues like this. In older adults, central nervous system disorders like dementia or Parkinson's also come to mind.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285
- Nemeroff, C. B. (Ed.). (2012). Management of treatment-resistant major psychiatric disorders. Oxford University Press.
Slide 8 of 11
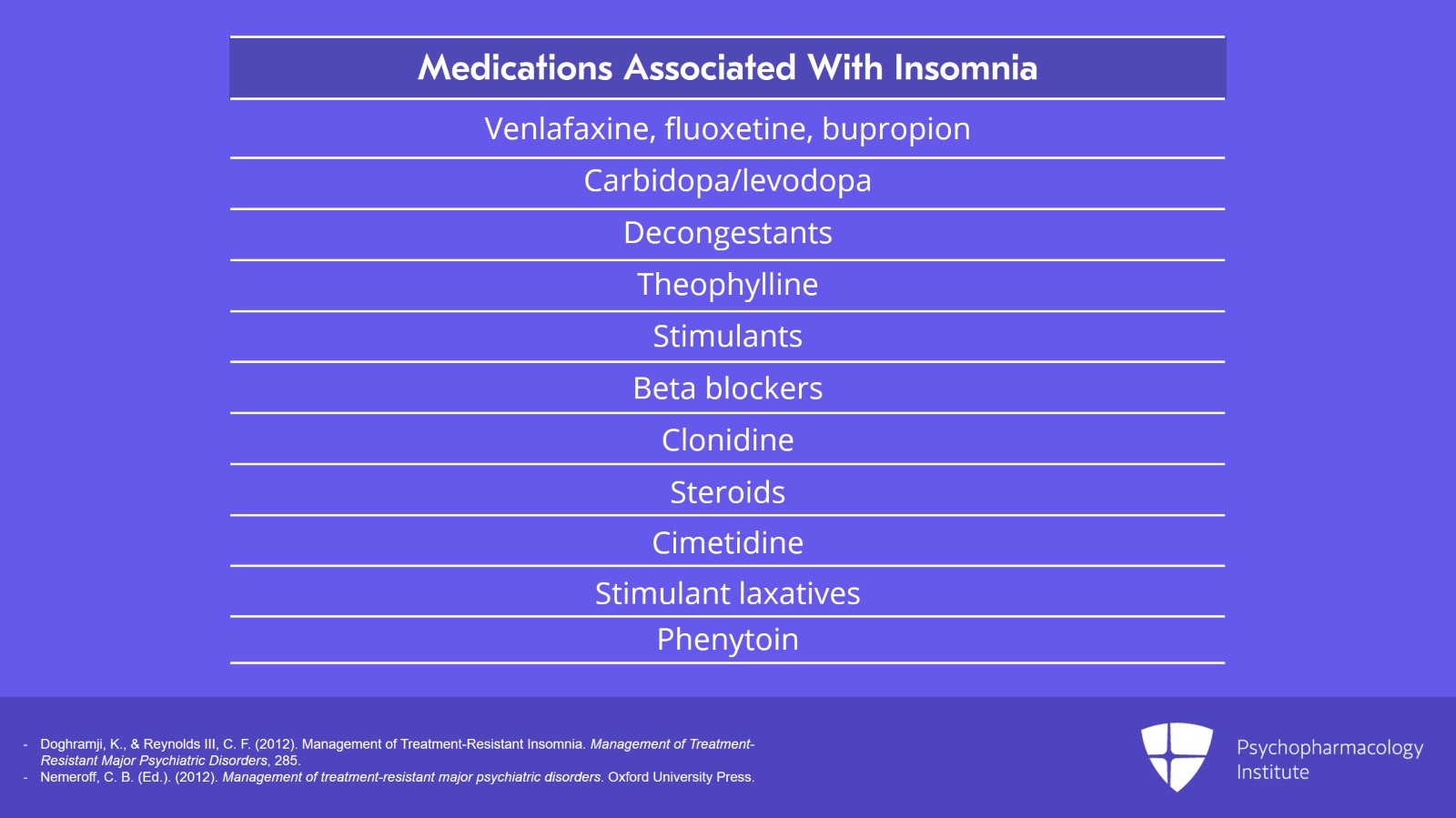
Consider also the medications being ingested by the patient and in particular at what time of day they are being taken. If a medication is arousing, for example, it may be better if it's prescribed for ingestion earlier in the day rather than later in the day. It's important to have a good handle on all the medications that a patient is using. We've dealt with issues like this at greater length in a chapter by Karl Doghramji and I published in Charlie Nemeroff's volume and I recommend that to you. It's captioned here.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285
- Nemeroff, C. B. (Ed.). (2012). Management of treatment-resistant major psychiatric disorders. Oxford University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 11
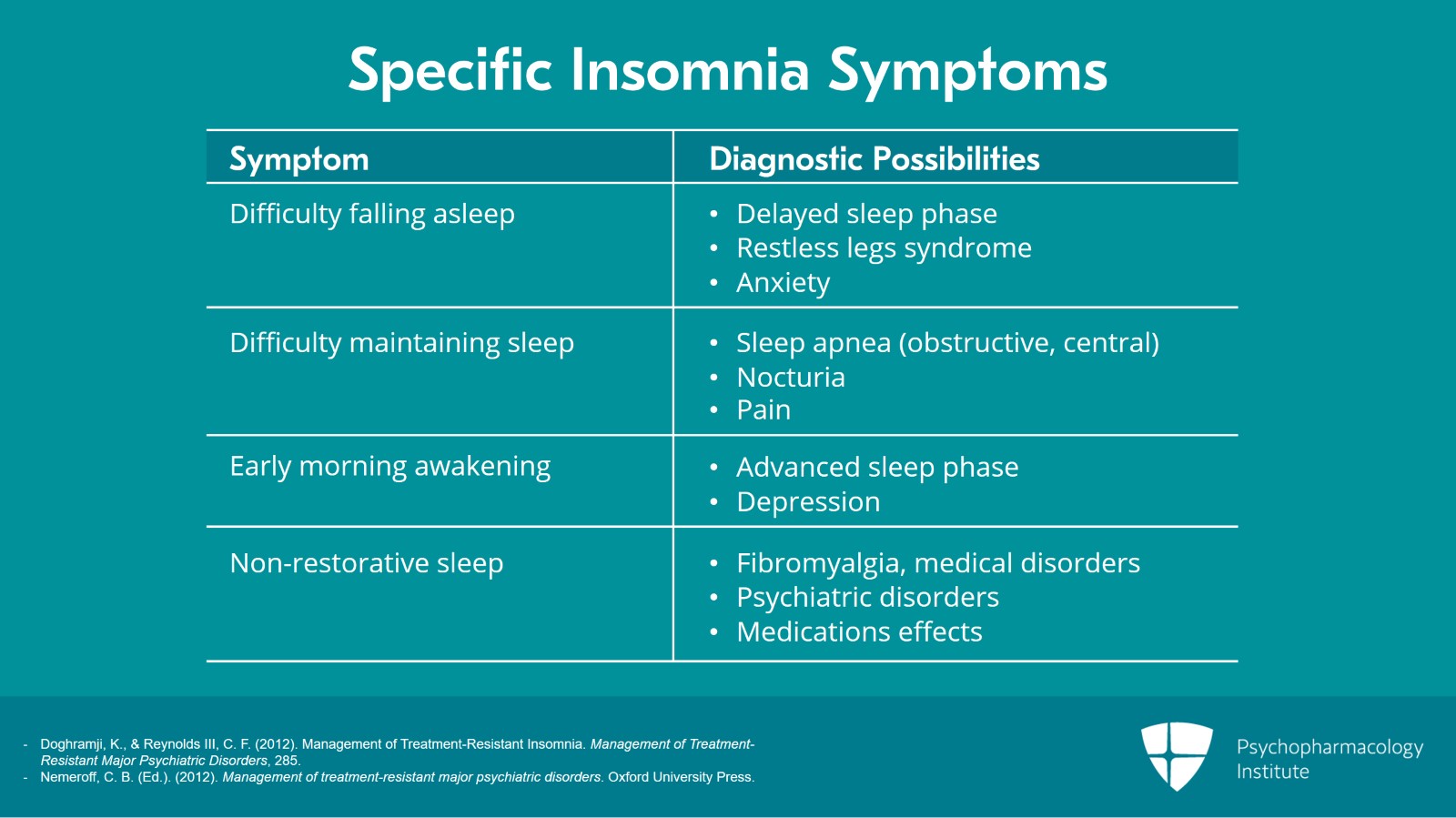
A useful part of the workup of insomnia disorder is to pay attention to the specific insomnia symptoms such as difficulty falling asleep, difficulty maintaining sleep, early morning awakening and nonrestorative sleep. Specific insomnia symptoms do aid in differential diagnosis and particularly so in the context of the patient's age. So for example, trouble falling asleep may signal a circadian rhythm sleep disorder such as a delayed sleep phase syndrome in a younger patient. Early morning awakening by contrast especially in an older patient could signal another type of circadian rhythm sleep disorder namely advanced sleep phase syndrome or possibly clinical depression. Difficulty maintaining sleep may result from pain or from a breathing-related sleep disorder as we saw in the case of Chip.
References:
- Doghramji, K., & Reynolds III, C. F. (2012). Management of Treatment-Resistant Insomnia. Management of Treatment-Resistant Major Psychiatric Disorders, 285
- Nemeroff, C. B. (Ed.). (2012). Management of treatment-resistant major psychiatric disorders. Oxford University Press.
Slide 10 of 11
And these are the key points to take home. It's important in other words to place insomnia symptoms within both a 24-hour or circadian context of sleep-wake rhythms as well as within the context of the particular patient's medical and psychiatric history. I would emphasize that like pain, symptoms of insomnia are often determined by many things. Understanding these factors helps to arrive at a specific treatment plan for the shared decision making with the patient and with their caregiver.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.