Slides and Transcript
Slide 1 of 13
Video 2. Hoarding Disorder: DSM-5 Criteria, Clinical Features, Epidemiology, and Comorbidities.
Slide 2 of 13
Hoarding disorder gets my award for the most famous psychiatric disorder that never existed prior to DSM-5. In DSM-IV, it mentioned hoarding but only as one criterion for obsessive-compulsive personality disorder. It was not in the criteria for OCD and it was not listed as a stand-alone disorder.
OCD and OCPD are not at all correlated with each other.
There is also no correlation between hoarding disorder and OCPD as well. Because hoarding disorder did not exist until DSM-5, research and expertise have lagged in this area. So there really is a lack of scientific knowledge in many things that we would like. Despite the fact that hoarding disorder did not exist prior to DSM-5, it was very well known in the popular media and there were numerous TV shows about this. Many of the shows were exploitative and really took advantage of people with hoarding although there was at least one show that was done professionally and done with respectable professionals.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 13
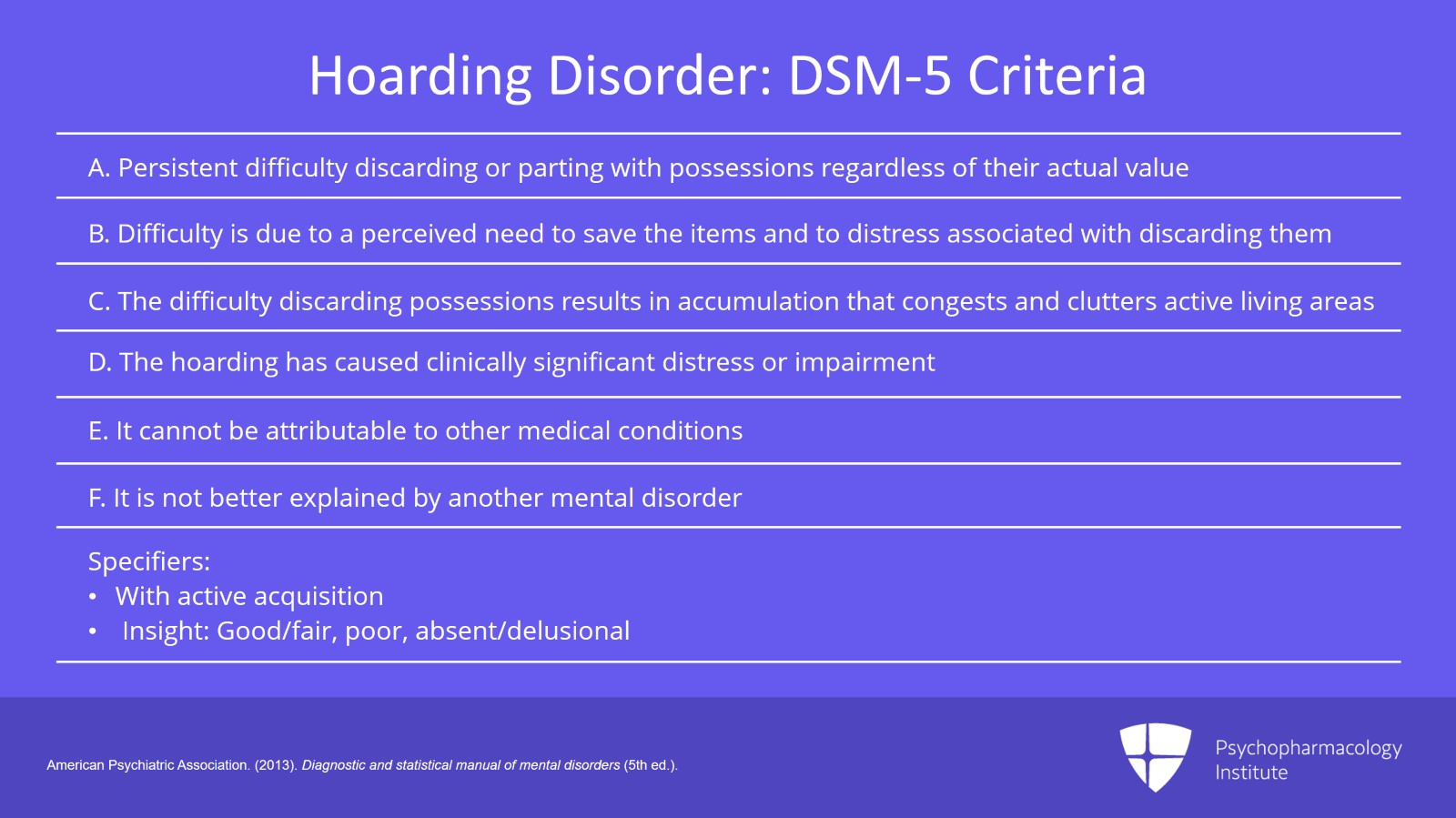
So what are the DSM-5 criteria for hoarding disorder?
The A criteria: Persistent difficulty discarding or parting with possessions regardless of their actual value. The difficulty throwing things away, it’s believing that trash is treasure.
B, difficulty is due to a perceived need to save the items and to distress associated with discarding them. There is an emotional attachment to these items and very distress associated with discarding them because they believe they have value that there does not exist.
The difficulty discarding possessions results in the accumulation of possessions that congest and clutter active living areas and substantially compromises their intended use. If living areas are uncluttered, it’s only because of the interventions of third parties. So in other words, to meet the criteria for hoarding, they have to have hoarding so bad that you cannot use the living areas for what they were originally intended for.
The hoarding of course has caused clinically significant distress or impairment in social, occupational or other important areas of functioning. And this includes maintaining a safe environment.
Hoarding cannot be attributable to other medical conditions such as brain injury or Prader-Willi syndrome.
And the hoarding is not better explained by symptoms of another mental disorder.
An example of this would be obsessions in OCD. This is probably the thing that I see that is most difficult to distinguish.
Many people with OCD will have what we call hoarding obsessions or hoarding compulsions. And simply what this is, people with OCD will have difficulty throwing something away because they need to check it repeatedly. So perhaps they are afraid to throw away an old bill because they need to check it 20 times to make sure they paid the exact amount. Because this is so anxiety provoking, they’re afraid to throw the bill away. So as a result, they keep it. So the fact that old bills from 10, 20, 30 years ago may be cluttering their house and are causing difficulty in their living areas, it’s not because they want to keep the bills, it’s not because the bills have any special attachment or meaning to them, it’s simply because the ritual of throwing away the bill is just too complex and it’s easier to avoid the ritual.
Specify with active acquisition. So if symptoms are accompanied by excessive collecting or buying or stealing of items that are not needed for or which there are no available space. Most of the people who are experts in hoarding disorder no longer give handouts for lecture. It’s very common at a hoarding disorder lecture where someone in the audience with hoarding disorder will take all the copies of the handout. That would be an example of excessive acquisition. People who steal things that they don’t need from the store in order to get multiple copies of it and to save it home, that would be another example of excessive acquisition.
Specify insight, good/fair, poor, absent or delusional.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Slide 4 of 13
So what are the clinical features of hoarding disorder?
Most people do have excessive acquiring, 80% to 90%. So that’s the vast majority of people.
They fail to discard possessions and the clutter makes this living space again unusable. They’re unable to use the couch. They’re unable to use their bed. They can’t lie down in bed because their bed is piled with clutter.
This causes marked impairment with them.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Gilliam, C. M., & Tolim, D. F. (2011). Compulsive hoarding. In Hudak, R. & Dougherty, D. D. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 13
They have a heightened responsibility and emotional attachment to objects. And they may not want to throw away an old dirty pizza box because they may say, I had dinner with my son three years ago and we ate from this pizza and I love this because it reminds me of my son. What you may consider trash has that kind of emotional attachment to them. There’s no sorting, organizing or discarding of these objects.
So they’re different than a collector. You go to someone who’s a collector. Everything is neatly arranged. People who hoard, they do not do that. Everything is just kind of scattered pell-mell. They know where it is. They know where all their junk is. Surprisingly, they can point you to a lot of it but there’s no rhyme or reason to their organization.
These people have very low motivation for treatment.
And the only times that their living spaces are uncluttered is if they live, for example, with their parents, if they’re children living with their parents and their parents can force them to clean, if they live with others that force them to clean or perhaps they live in a group home or some sort of government housing that again forces them to clean.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Hudak, R. & Dougherty, D. D. (2011). Compulsive hoarding. In Gilliam, C. M., & Tolim, D. F. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Slide 6 of 13
Now, the epidemiology.
The prevalence may be as high as 5% in this illness which would make it twice as common as OCD.
Most cases, most people with hoarding disorder do not meet criteria for OCD or obsessive-compulsive personality disorder. As I said, there’s no correlation between those three disorders.
This often begins in childhood but we don’t see it in children because their parents will clean their rooms or force them to clean their rooms. So therefore, it’s more prevalent in adults.
We don’t know if there’s relationship with gender or race. That still isn’t known.
Is hoarding one disorder or could there be three or four disorders and hoarding be kind of a larger category of disorders? Again, it’s possible but we don’t know.
References:
- Hudak, R. & Dougherty, D. D. (2011). Compulsive hoarding. In Gilliam, C. M., & Tolim, D. F. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 13
We do know that there’s a large impact to hoarding. Almost 2/3 of health departments have received a complaint about a hoarder in the last five years. Most often, they’re reported by their neighbors. So sometimes, the clutter gets so severe, the clutter moves outside the house. It will extend into the car. It extends into the yard. That’s when health departments get involved.
Deaths have been reported. People have been trapped in their house with fire unable to get out because of clutter. There have been famous cases of houses collapsing due to weight of clutter and people killed in the collapse.
People with hoarding have work impairment that’s so severe that it’s similar to those with psychotic disorders.
There are significant family consequences. People have a marked decrease in the rate of marriage and 1/3 of people with hoarding are below the poverty line.
References:
- Frost, R. O., Steketee, G., & Williams, L. (2000). Hoarding: A community health problem. Health and Social Care in the Community, 8(4), 229-234
Slide 8 of 13
Now, the vast majority of people with hoarding, 92% have another Axis 1 or Axis 2 psychiatric disorder to use prior to DSM-5 terminology there.
Dementia or organic brain syndromes are very common in people with hoarding.
Personality disorders also are very common, not OCPD, however, but other personality disorders can be very common.
ADHD can be a very common comorbidity in people with hoarding disorder as well as impulse control disorder.
References:
- Frost, R. O., Steketee, G., & Tolin, D. F. (2011). Comorbidity in hoarding disorder. Depression and Anxiety, 28(10), 876-884.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 13
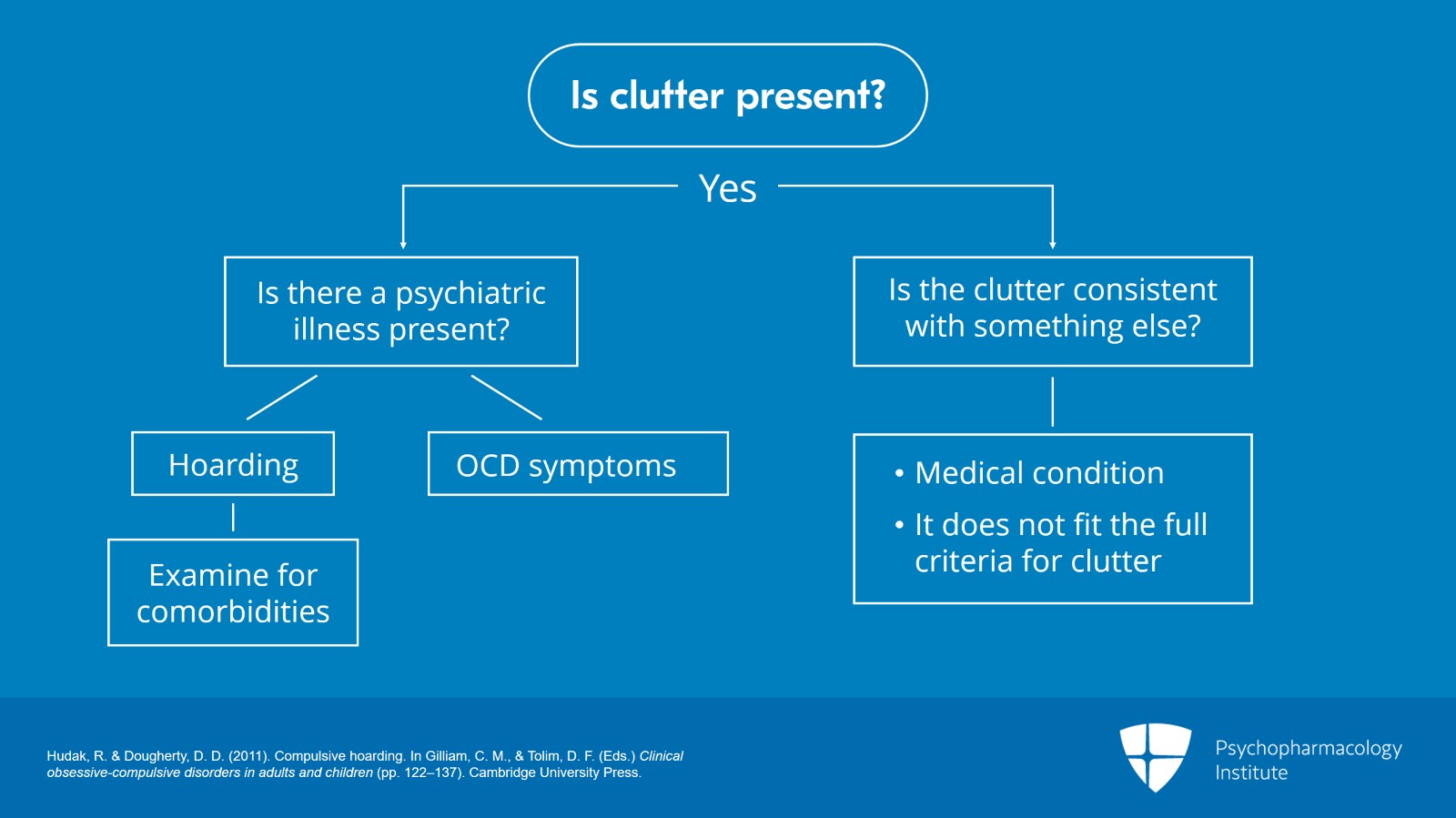
I have a diagnostic algorithm I tend to use for hoarding.
So first off, if you’re seeing a person, evaluating them, determine, is there clutter present? If they have clutter, determine, is there a psychiatric illness present or is the clutter just consistent with something else? It could be a medical condition. It could be that they’re a sloppy housekeeper. Maybe it doesn’t fit the full criteria for clutter.
Determine, is it hoarding or OCD hoarding? So someone does have the clutter and it does appear to be psychiatrically based. Is it hoarding? Or as I said before, is it the hoarding that simply comes from OCD symptoms, people having fears of throwing things away?
If there is hoarding, then the last piece, you must examine for comorbidity because the vast majority of these people will have comorbidity.
References:
- Hudak, R. & Dougherty, D. D. (2011). Compulsive hoarding. In Gilliam, C. M., & Tolim, D. F. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Slide 10 of 13
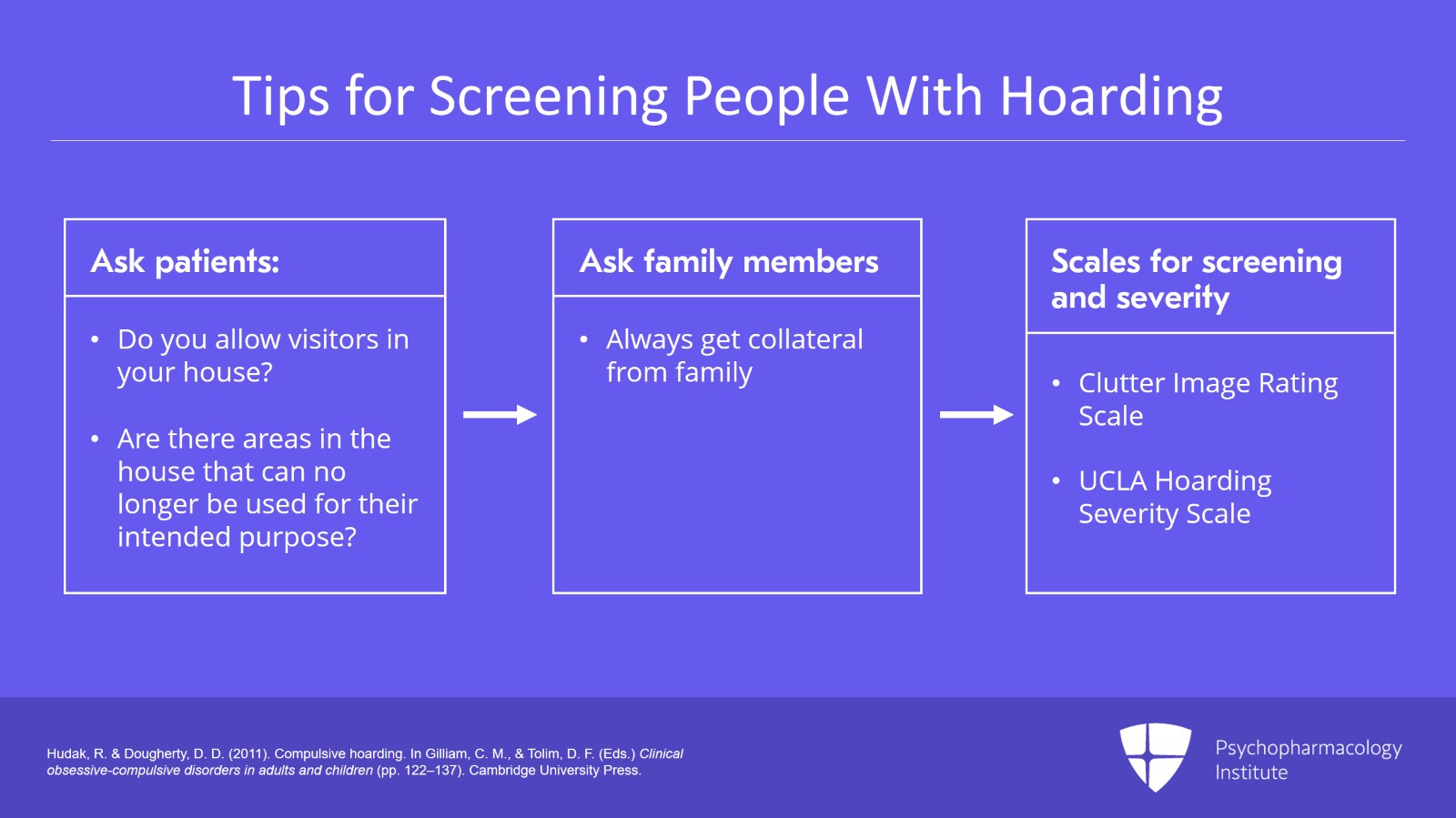
Some tips in order to help screen for people with hoarding.
Ask patients if they allow visitors in their house. Ask them if their family members will allow friends to come over into the house. Or are they too ashamed to have their friends over?
Ask them, are their areas in the house that can be no longer used for their intended purpose? In other words, tables or beds can’t be used because of clutter.
Always get collateral from family.
Now, there are photographic scales that can also be used that shows different levels of clutter. For example, there’s the Clutter Image Rating scale and there’s the UCLA Hoarding Severity Scale as well.
What you can use with the Clutter Image Rating scale is to show people, is this what your house looks like? It’s a series essentially of nine images that shows different parts of an example house with small amounts of clutter to large amounts of clutter. And you can show this to people and have them point out this is what their living space looks like. And that can be used to rate severity but I think it’s also a good screening tool as well.
References:
- Hudak, R. & Dougherty, D. D. (2011). Compulsive hoarding. In Gilliam, C. M., & Tolim, D. F. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 13
Key points.
Hoarding disorder is very common.
It has an insidious onset that may begin as early as childhood.
It can cause significant morbidity and even mortality.
Slide 12 of 13
There’s significant community health risks as most public health departments report receiving complaints about hoarding.
Patients should be screened for comorbidity as dementia, ADHD, personality disorders, impulse control disorders as well as other Axis I or Axis II disorders are very common.
Thank you.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.