Slides and Transcript
Slide 2 of 26
Well, this is really the big question currently. Anecdotal evidence would say yes. Randomized controlled trials are definitely needed with doses that are practical and outcomes that are able to be measured. I'm going to talk a little bit about the historic use of antipsychotics as a means of managing delirium and then we're going to dive into specific agents. So antipsychotics have really been the mainstay of delirium management for decades. They're used to manage agitation and they're used to mitigate perceptual disturbances.
References:
- Maldonado, J. R. (2017). Acute brain failure. Critical Care Clinics, 33(3), 461-519.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 26
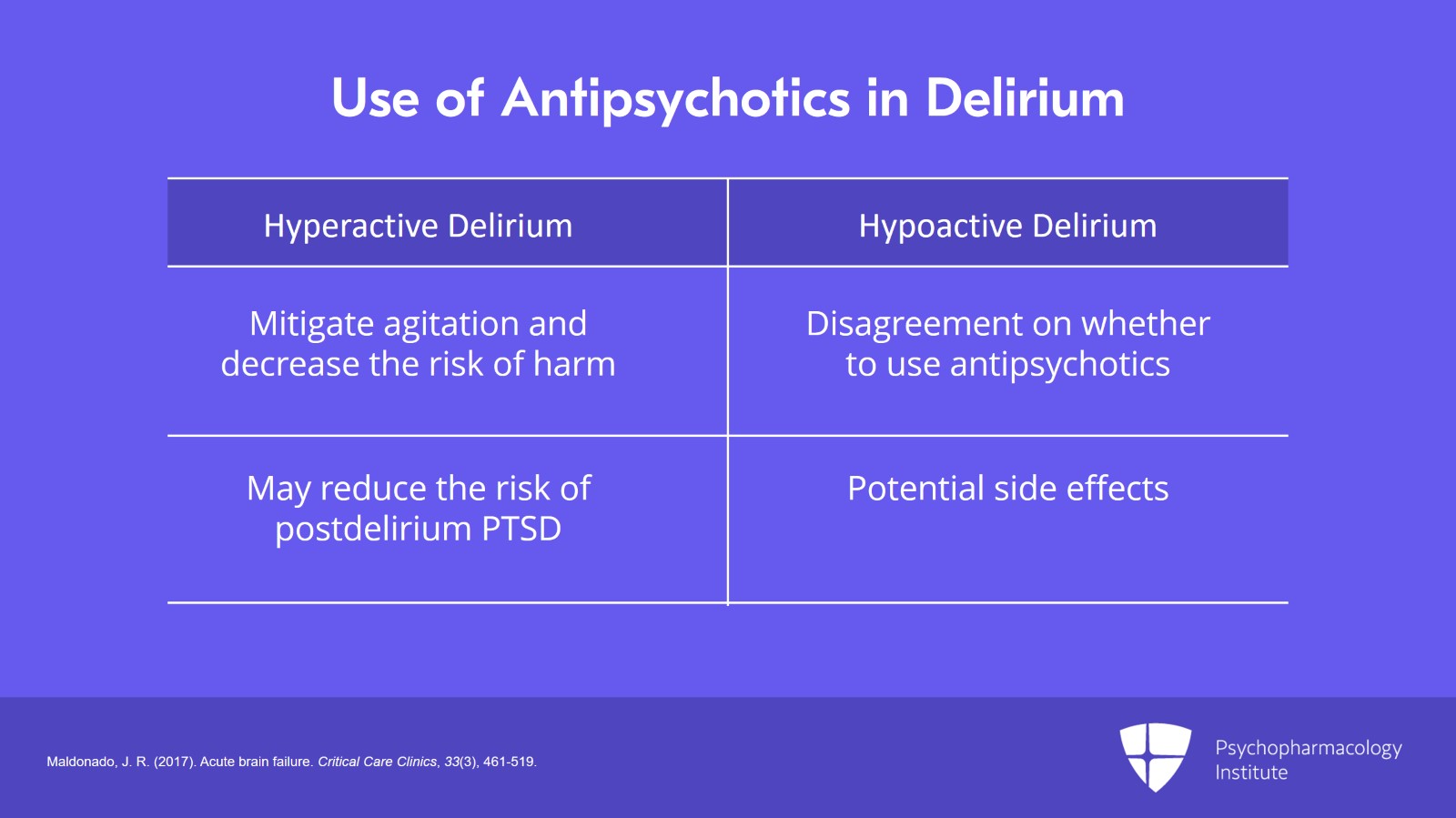
Individual psychiatrists will vary in terms of which delirious patients they prescribe antipsychotics to but most consult psychiatrists would agree that there are two broad groups for whom antipsychotics can be particularly helpful, those with a hyperactive delirium in which the antipsychotic is being used to mitigate agitation and decrease the risk of harm to the patient and to staff and those with significant perceptual disturbances for whom the antipsychotics may reduce the risk of a post-delirium PTSD. It's important to keep in mind that there's a large group that is not part of those two groups where patients have a hypoactive delirium without perceptual disturbances and there's really a lot of disagreement on whether to use antipsychotics in those patients. Some people believe that antipsychotics will still help with some symptoms that those patients might be experiencing where others feel like the risk of the antipsychotics and the potential side effects probably don't outweigh the benefit in those settings.
References:
- Maldonado, J. R. (2017). Acute brain failure. Critical Care Clinics, 33(3), 461-519.
Slide 4 of 26
In terms of the choice of specific agent, in the '80s and '90s, intravenous haloperidol and chlorpromazine were really the two major agents that were used. But in the past 20 years, second-generation antipsychotics have been used with increased frequency to help manage delirium. The choice of antipsychotics often ends up being based on receptor profile, side effects and really the personal preference of the prescribing or consulting physician.
References:
- Maldonado, J. R. (2017). Acute brain failure. Critical Care Clinics, 33(3), 461-519.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 26
Talking about individual agents, we'll start with intravenous haloperidol. The use of IV haloperidol in delirium dates back to the 1970s. And originally, haloperidol was chosen because it has a very high affinity for D2 receptors with little effect on serotonergic, alpha, histamine or cholinergic receptors. This is important because it tends to be a relatively clean drug and does not have anticholinergic side effects which might worsen the delirium. Importantly, haloperidol also acts as a sigma-1 antagonist though it's unclear what effect that has for delirious patients.
References:
- Chang, W., Francis Lam, Y. W., Jann, M. W., & Chen, H. (1992). Pharmacokinetics of haloperidol and reduced haloperidol in Chinese schizophrenic patients after intravenous and oral administration of haloperidol. Psychopharmacology, 106(4), 517-522.
Slide 6 of 26
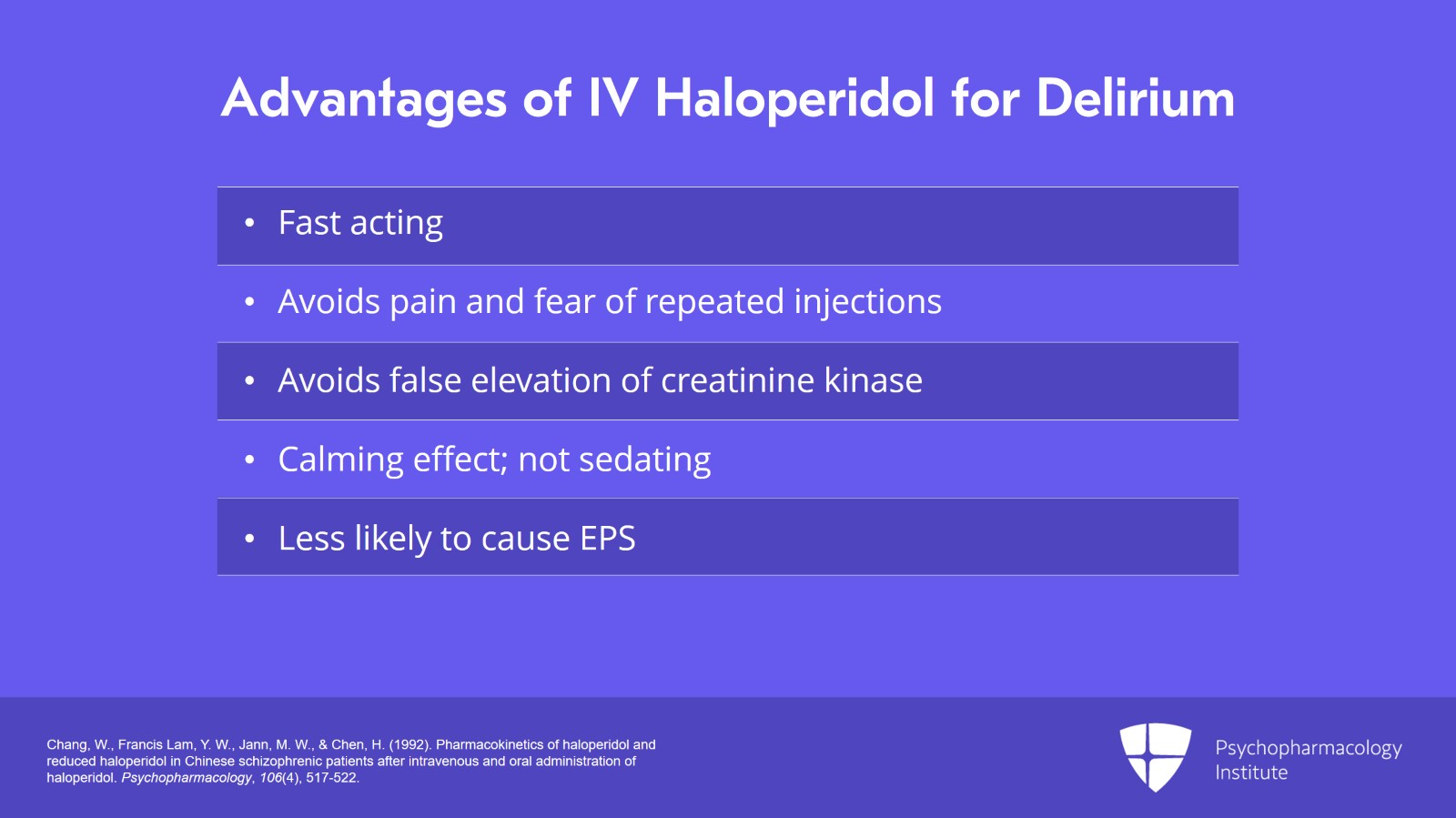
Traditionally, the intravenous route of haloperidol was preferred over other routes because it was fast acting. It avoided the pain and the fear that were often caused by repeated IM injections and it also avoided a false elevation of creatinine kinase which may be important if somebody develops symptoms that look potentially like neuroleptic malignant syndrome. IV haloperidol is twice as potent as the oral form, has a faster time to onset and a long-lasting effect. Very importantly, it is said to be calming but not sedating, meaning that when given by itself IV haloperidol will not snow the patient or make them unarousable. IV haloperidol is also shown to cause EPS very infrequently and is thought to be far less likely to cause EPS than other forms of haloperidol including oral and intramuscular varieties.
References:
- Chang, W., Francis Lam, Y. W., Jann, M. W., & Chen, H. (1992). Pharmacokinetics of haloperidol and reduced haloperidol in Chinese schizophrenic patients after intravenous and oral administration of haloperidol. Psychopharmacology, 106(4), 517-522.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 26
However, keep in mind that intravenous haloperidol does potentiate the sedative effects of other agents. So if it's given in conjunction with a sedating agent or at a time when a sedating agent has been given within the few hours surrounding the use of intravenous haloperidol, that may result in the patient becoming snowed or overly sedated because of the potentiating effects.
References:
- Chang, W., Francis Lam, Y. W., Jann, M. W., & Chen, H. (1992). Pharmacokinetics of haloperidol and reduced haloperidol in Chinese schizophrenic patients after intravenous and oral administration of haloperidol. Psychopharmacology, 106(4), 517-522.
Slide 8 of 26
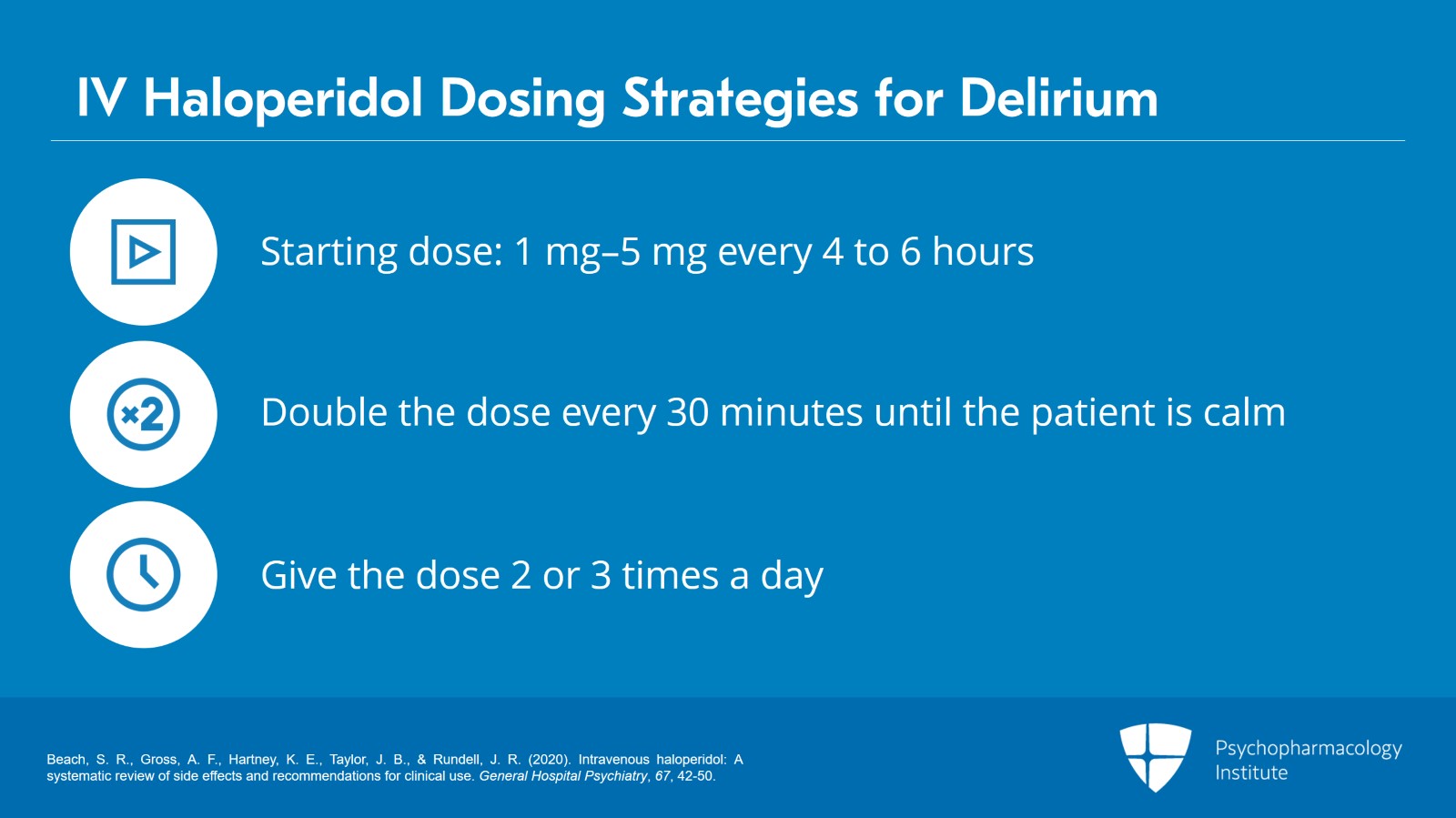
Typical starting doses are anywhere from 1 to 5 mg every four to six hours though sometimes reduced doses of less than 1 mg are used in frail or elderly patients. Prior algorithms suggest doubling the dose every 30 minutes until the patient is calm but not sedated. This is thought to be because for unclear reasons the effect of IV haloperidol does not seem to be cumulative. So if you give the patient the same dose repeatedly, they're unlikely to respond more to a subsequent dose than they did to the initial dose. However, if you increase the dose, there seems to be an increased likelihood of response. Once the desired effect is achieved, that dose is usually given as a standing dose two to three times a day.
References:
- Beach, S. R., Gross, A. F., Hartney, K. E., Taylor, J. B., & Rundell, J. R. (2020). Intravenous haloperidol: A systematic review of side effects and recommendations for clinical use. General Hospital Psychiatry, 67, 42-50.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 26
I think it's important to keep in mind that sometimes the approach of doubling the dose every 30 minutes can lead to doses that seem absurd or seem unlikely to have an effect. We tolerate pretty high doses of haloperidol on our consult service and will sometimes give single doses of up to even 50 mg. And while some of our attendings have experienced giving single doses of hundreds of milligrams, we generally stop before we get to that point and recommend that alternative agents be utilized if agitation persists.
References:
- Beach, S. R., Gross, A. F., Hartney, K. E., Taylor, J. B., & Rundell, J. R. (2020). Intravenous haloperidol: A systematic review of side effects and recommendations for clinical use. General Hospital Psychiatry, 67, 42-50.
Slide 10 of 26
I want to address one concern that's often brought up with regard to intravenous haloperidol and that is the potential effect on QT prolongation and torsade. Our group recently completed a systematic review of this issue and our conclusion is that the concerns about QT prolongation with intravenous haloperidol may be significantly overblown. The current FDA recommendation is for the use of telemetry at all doses of intravenous haloperidol though this is not commonly done in most hospital settings. However, recent perspective studies indicate that doses up to 20 mg are actually not associated with any significant QT prolongation and those are pretty good randomized placebo-controlled trials. So we have put forth a set of revised recommendations.
References:
- Beach, S. R., Gross, A. F., Hartney, K. E., Taylor, J. B., & Rundell, J. R. (2020). Intravenous haloperidol: A systematic review of side effects and recommendations for clinical use. General Hospital Psychiatry, 67, 42-50.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 26
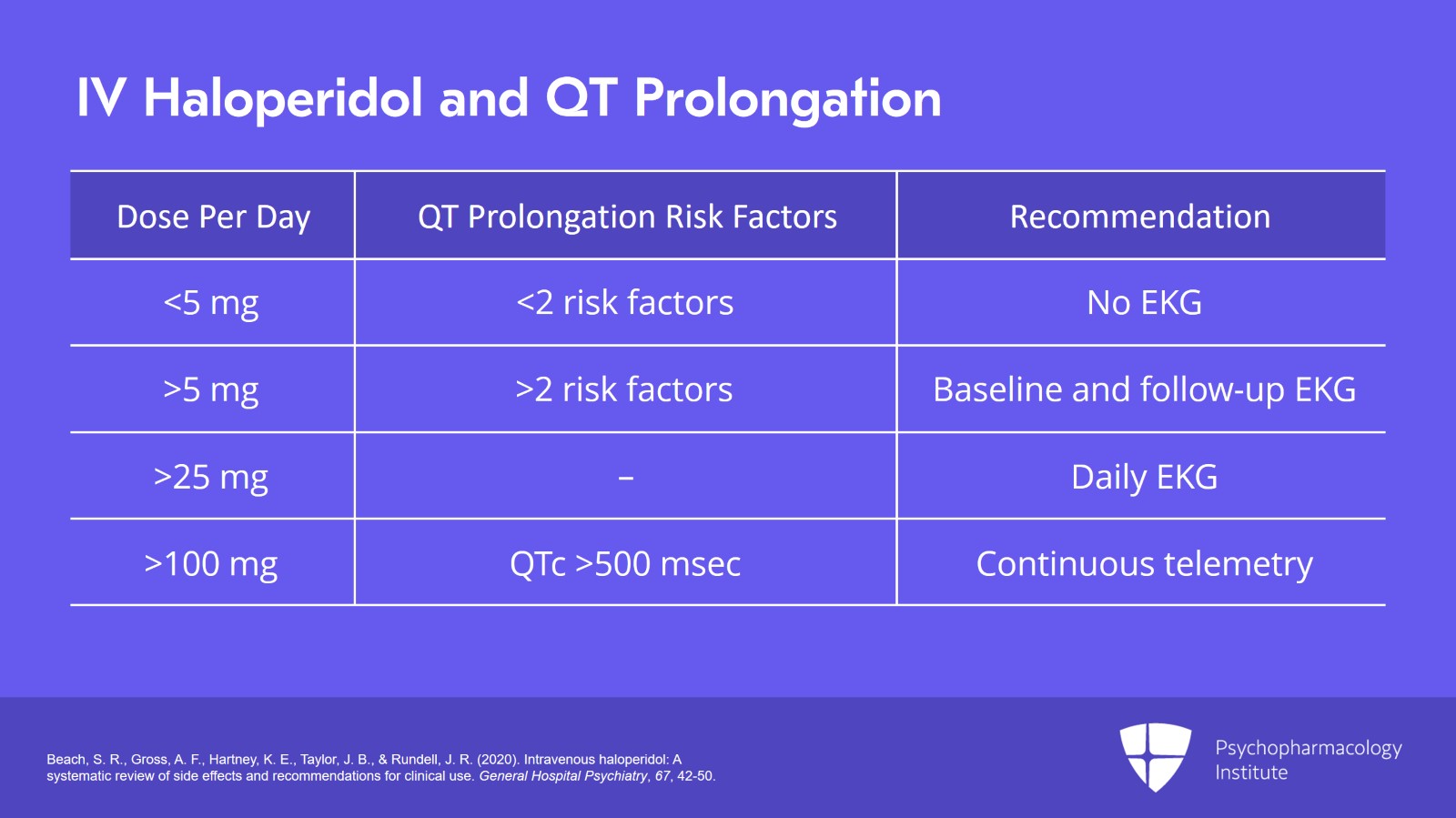
Our recommendations suggest that no EKG monitoring at all should be required if the total dose is less than 5 mg daily and less than two other risk factors for QT prolongation or torsade are present. For patients who are getting more than 5 mg daily or have two or more risk factors, we recommend a baseline EKG and at least one follow-up EKG preferably 30 to 60 minutes after administration. Most hospitals and most psychiatry consult services are sort of reflexively recommending daily EKGs for patients with intravenous haloperidol. And our review found that this is probably only indicated for patients who receive a total cumulative dose of greater than 25 mg of IV haloperidol. And then finally for the patients receiving the highest dose, doses greater than 100 mg or who are at the highest risk for torsade, those with a QTc properly corrected of over 500 msec, for those patients, we would think about continuous telemetry or alternative agents.
References:
- Beach, S. R., Gross, A. F., Hartney, K. E., Taylor, J. B., & Rundell, J. R. (2020). Intravenous haloperidol: A systematic review of side effects and recommendations for clinical use. General Hospital Psychiatry, 67, 42-50.
Slide 12 of 26
Another thing that was really important in our review was a finding that there is really minimal evidence to suggest that any other antipsychotic is actually safer than intravenous haloperidol with regard to QT prolongation. So we often hear that in cases where the QT gets prolonged, we'll switch to quetiapine or switch to olanzapine because that's a little bit safer than intravenous haloperidol. There's really no good evidence to suggest that that's true. And in fact, I would say if there's enough concern about QT prolongation that you want to stop using IV haloperidol, I would recommend using a non-antipsychotic agent for that patient.
References:
- Beach, S. R., Gross, A. F., Hartney, K. E., Taylor, J. B., & Rundell, J. R. (2020). Intravenous haloperidol: A systematic review of side effects and recommendations for clinical use. General Hospital Psychiatry, 67, 42-50.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 26
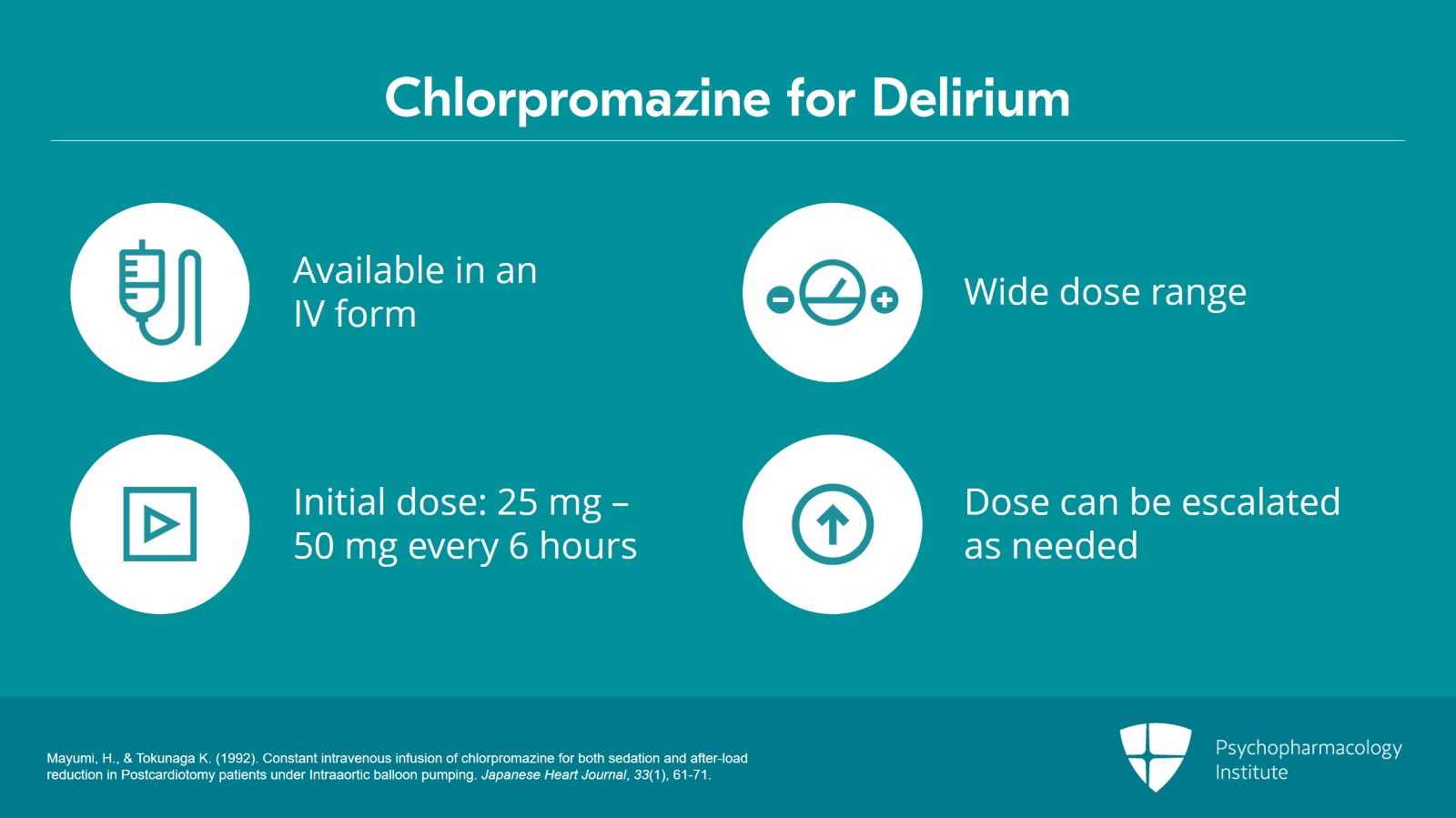
Switching now to another agent that was traditionally used for delirium, chlorpromazine. Chlorpromazine was also widely used because it was available in an IV form and because it had a wide dose range. Typically, people would start at something like 25 to 50 mg every six hours but the dose could be escalated quickly as needed.
References:
- Mayumi, H., & Tokunaga K. (1992). Constant intravenous infusion of chlorpromazine for both sedation and after-load reduction in Postcardiotomy patients under Intraaortic balloon pumping. Japanese Heart Journal, 33(1), 61-71.
Slide 14 of 26
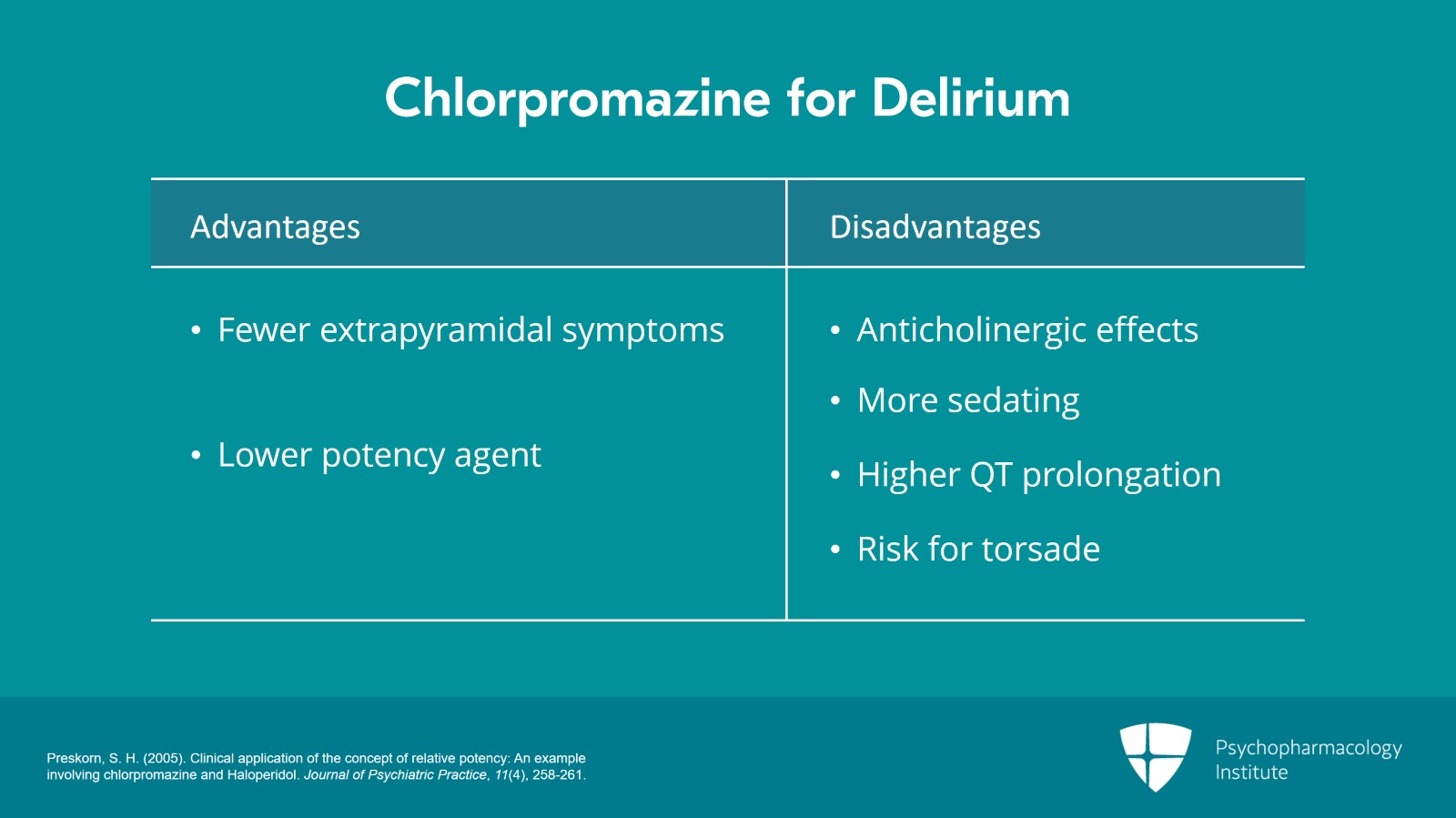
Another advantage of chlorpromazine is that it tends to cause less extrapyramidal symptoms because it's a lower potency agent. However, its low potency means that it has more significant alpha-1 and anticholinergic effects. And that is tricky to balance in a delirious patient when we know that anticholinergic medications cause or contribute to delirium. Chlorpromazine is more sedating than haloperidol. Sometimes, that can be a benefit but sometimes that can be a risk. And remember that the sedating properties are again due to anticholinergic effects. Finally, keep in mind that chlorpromazine being a low potency phenothiazine is actually associated with a high amount of QT prolongation and a significant risk for torsade when compared to other agents. Low potency phenothiazines are actually the class that are most represented in cases of QT prolongation or torsade. So chlorpromazine remains a very viable option. It's great because of its availability in IV form and its lower likelihood to cause EPS but there are a few things that you need to be mindful of when using it.
References:
- Preskorn, S. H. (2005). Clinical application of the concept of relative potency: An example involving chlorpromazine and Haloperidol. Journal of Psychiatric Practice, 11(4), 258-261.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 26
As I mentioned, over the past two decades, second-generation or atypical antipsychotics have become much more prevalent in terms of their use. They tend to be more sedating. And again, this can sometimes be a good thing in delirium. It can sometimes be a bad thing in delirium. They were originally used because they were felt to be safer in terms of side effects. They were thought to cause less EPS. They were thought to cause less QT prolongation. But these comparisons really don't have robust supporting data. And again, it's important to keep in mind that many atypical antipsychotics have prominent anticholinergic effects and this is partially what drives their lower potency.
References:
- Maldonado, J. R. (2017). Acute brain failure. Critical Care Clinics, 33(3), 461-519.
Slide 16 of 26
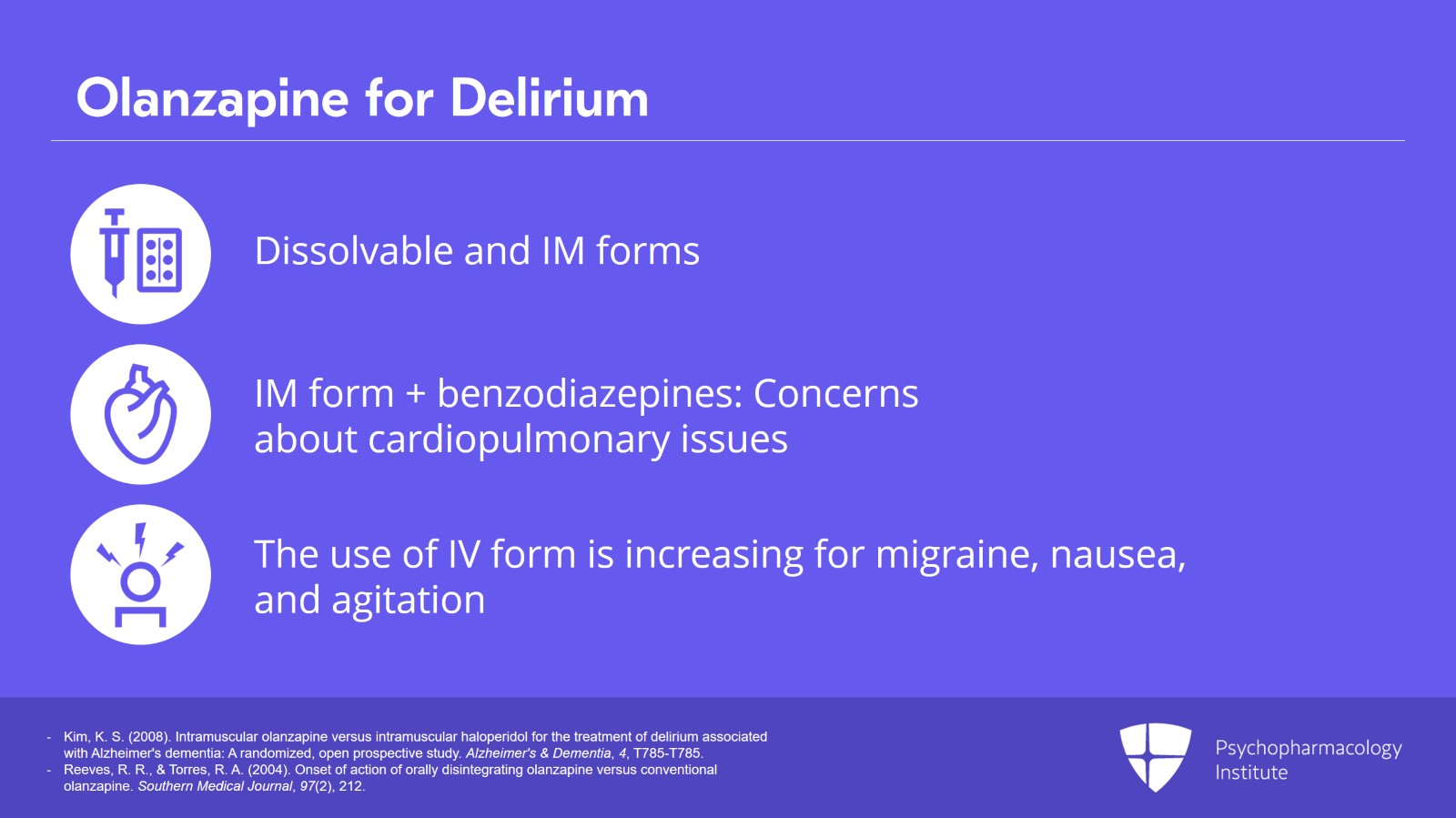
Starting with olanzapine, olanzapine is available in dissolvable and intramuscular forms which increase its ability to be given to a variety of patients. Remember that the intramuscular form does have some concerns. If given with benzodiazepines, there are concerns for cardiopulmonary issues and so you have to be careful about giving IM olanzapine if the patient is also receiving benzodiazepines. Important for psychiatrists to recognize is that in some hospital settings particularly in emergency rooms IM olanzapine is starting to be given in the IV form. This is actually similar to the way that IV haloperidol gained traction where the IM form is just given through the IV. And this is being used in emergency department settings to manage primarily migraine headache and nausea though in some cases it's started to be used for agitation. So it's important for psychiatrists to be aware of that growing trend as well.
References:
- Kim, K. S. (2008). Intramuscular olanzapine versus intramuscular haloperidol for the treatment of delirium associated with Alzheimer's dementia: A randomized, open prospective study. Alzheimer's & Dementia, 4, T785-T785.
- Reeves, R. R., & Torres, R. A. (2004). Onset of action of orally disintegrating olanzapine versus conventional olanzapine. Southern Medical Journal, 97(2), 212.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
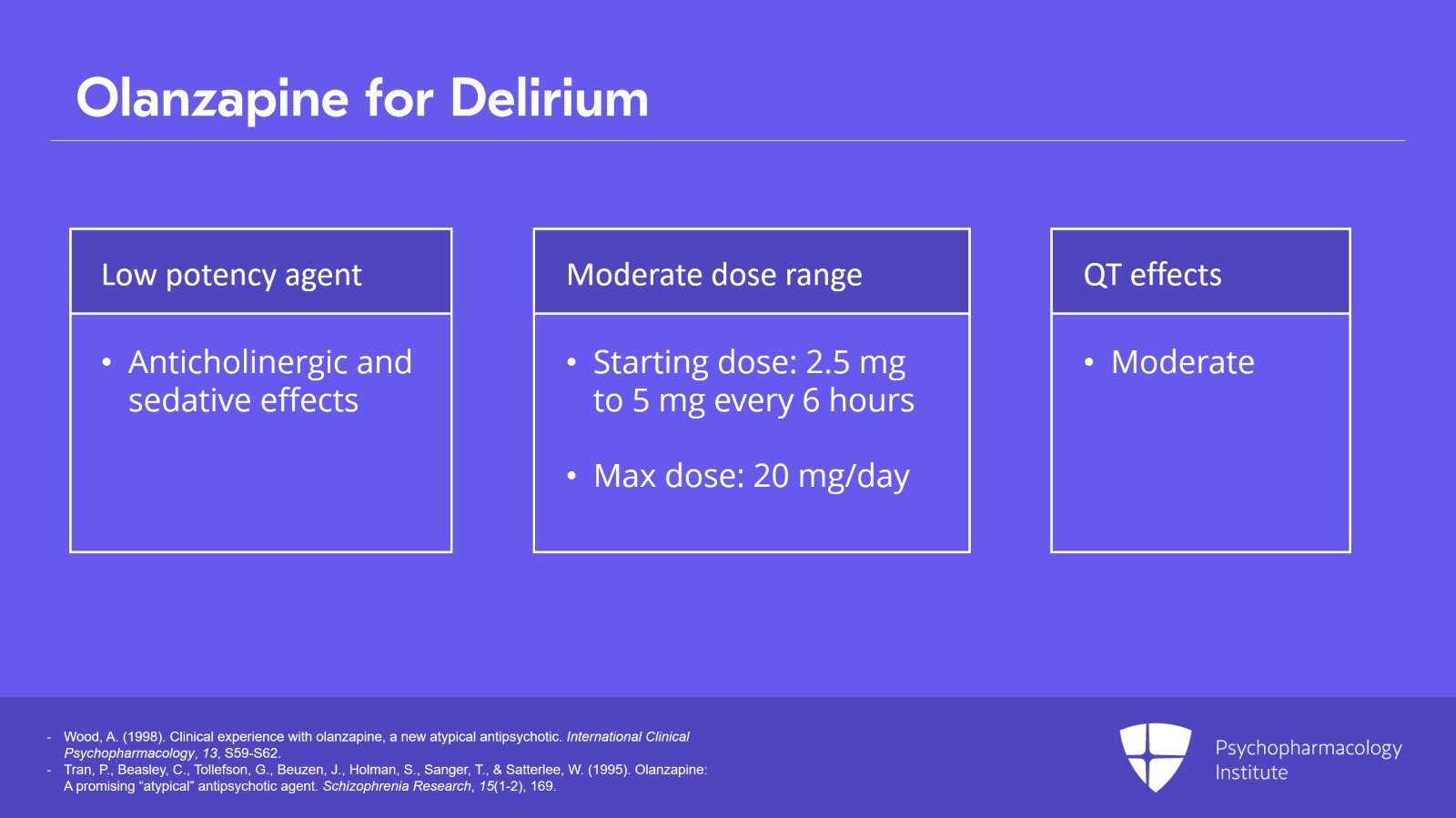
Slide 17 of 26
Olanzapine is a low potency agent. It's a dirty drug affecting multiple receptors and that includes anticholinergic effects and it tends to be quite sedating. Another drawback of olanzapine is that it has a pretty moderate dose range. So we typically start it for delirium at 2.5 to 5 mg every six hours but we don't have a lot of ceiling to go up because the max dose remains about 20 mg daily. The QT effects of olanzapine are moderate. So it's in the large group of antipsychotics that are somewhat in the middle. There's older lore that it's safer than other agents but that really hasn't borne out. And we really can't even say that it's safer than intravenous haloperidol.
References:
- Wood, A. (1998). Clinical experience with olanzapine, a new atypical antipsychotic. International Clinical Psychopharmacology, 13, S59-S62.
- Tran, P., Beasley, C., Tollefson, G., Beuzen, J., Holman, S., Sanger, T., & Satterlee, W. (1995). Olanzapine: A promising “atypical” antipsychotic agent. Schizophrenia Research, 15(1-2), 169.
Slide 18 of 26
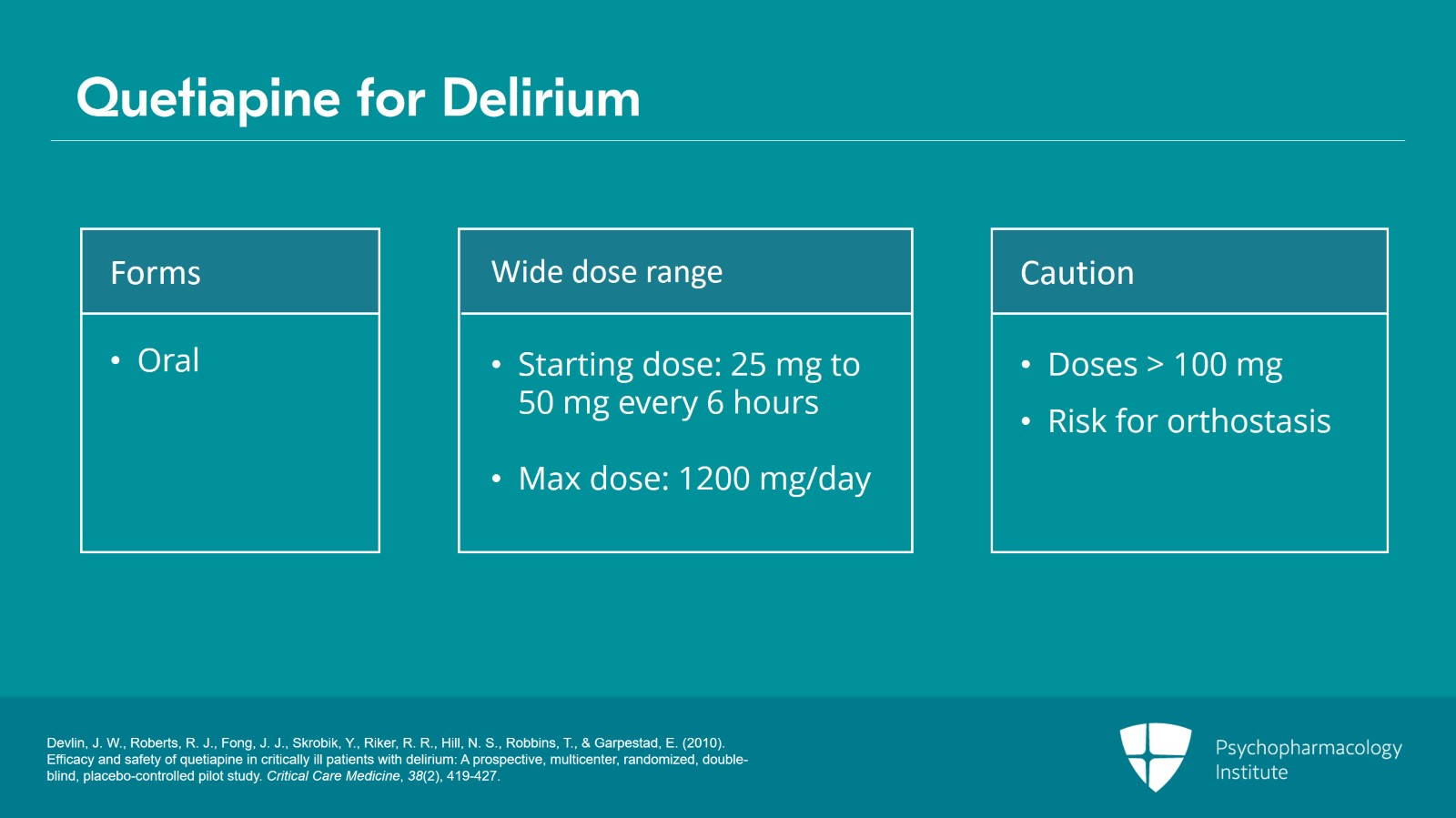
Another second-generation antipsychotic that is commonly used in delirium is quetiapine. Quetiapine is only available in oral form but it does have the advantage of having an exceedingly wide dose range. Doses typically start at 25 to 50 mg every six hours but doses up to 1200 mg a day are tolerated. It is important to be cautious about increasing doses by more than 100 mg a day due to the risk for orthostasis.
References:
- Devlin, J. W., Roberts, R. J., Fong, J. J., Skrobik, Y., Riker, R. R., Hill, N. S., Robbins, T., & Garpestad, E. (2010). Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Critical Care Medicine, 38(2), 419-427.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 26
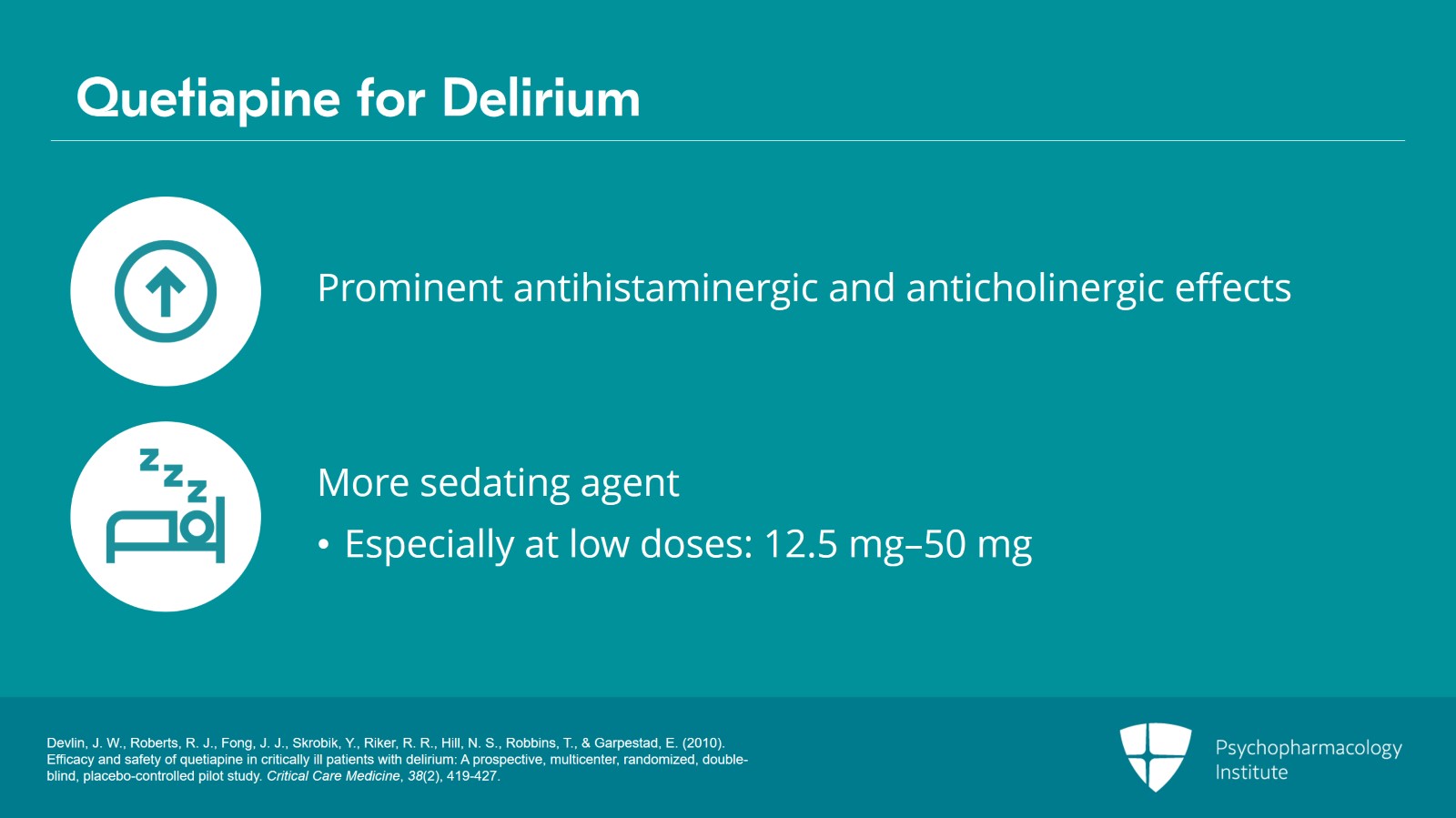
Again, quetiapine is a drug that interacts at multiple receptors and has prominent antihistaminergic and anticholinergic effects. This makes it more sedating as an agent. Importantly, especially at low doses like 12.5 to 50 mg, quetiapine is primarily acting through anticholinergic and antihistaminergic effects. So, if we think that the important mechanism of action of an antipsychotic with regard to delirium has to do with dopamine blockade, you're really not getting a lot of that with low-dose quetiapine.
References:
- Devlin, J. W., Roberts, R. J., Fong, J. J., Skrobik, Y., Riker, R. R., Hill, N. S., Robbins, T., & Garpestad, E. (2010). Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Critical Care Medicine, 38(2), 419-427.
Slide 20 of 26
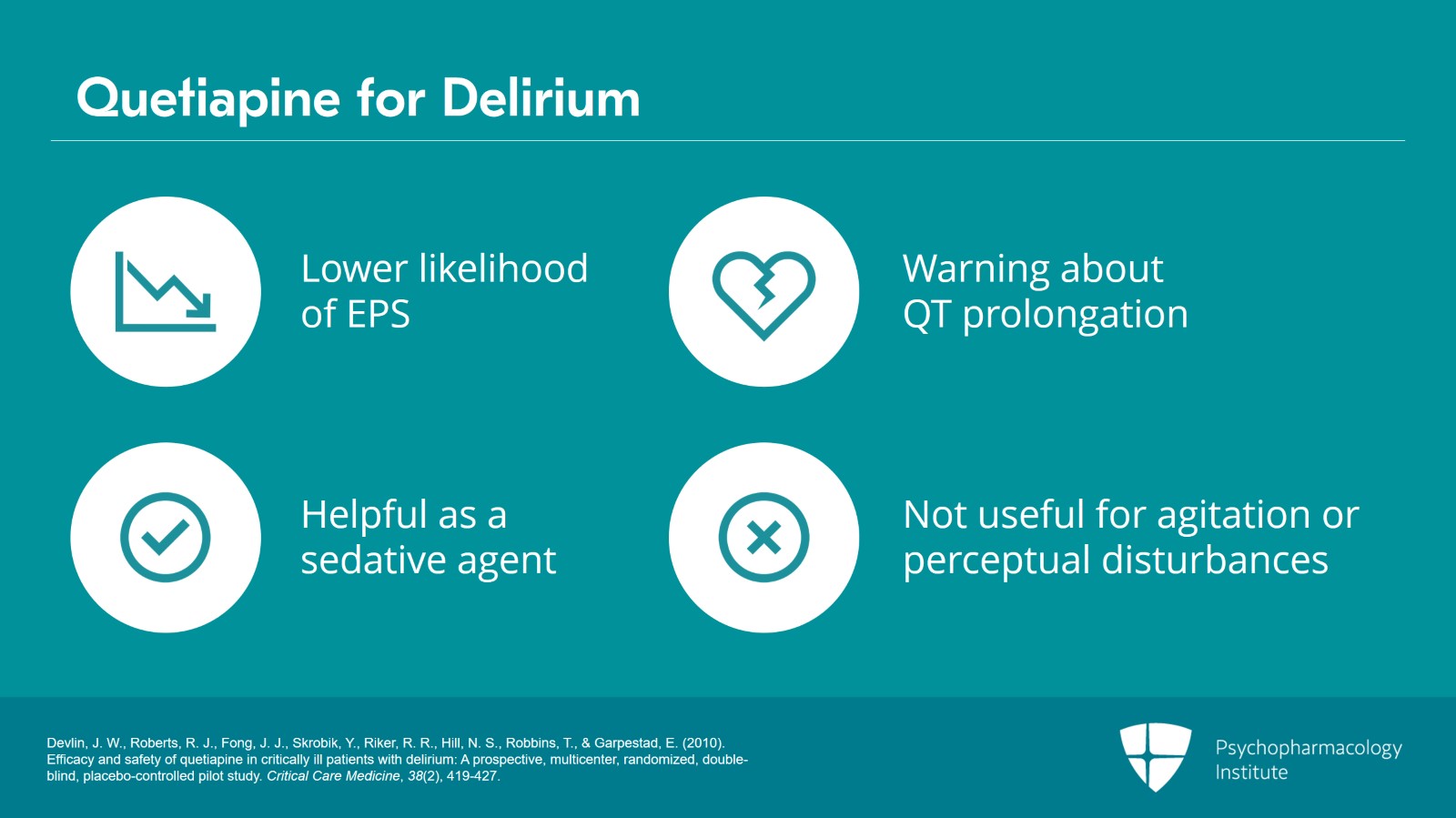
It is preferred by neurologists because of the lower likelihood to cause EPS but it does have an FDA warning about QT prolongation. Probably, it's not any different than any of the other drugs sort of in the middle range of QT prolongation but it's important to keep in mind that it's not fully safe from the standpoint of QT prolongation. So overall, I think quetiapine can be helpful when you're looking for a sedative agent. It can be particularly helpful as a soporific agent in the evenings for delirious patients. But I hesitate to use it for agitation or for perceptual disturbances at low doses because you're really not getting much other than an anticholinergic effect.
References:
- Devlin, J. W., Roberts, R. J., Fong, J. J., Skrobik, Y., Riker, R. R., Hill, N. S., Robbins, T., & Garpestad, E. (2010). Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Critical Care Medicine, 38(2), 419-427.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 26
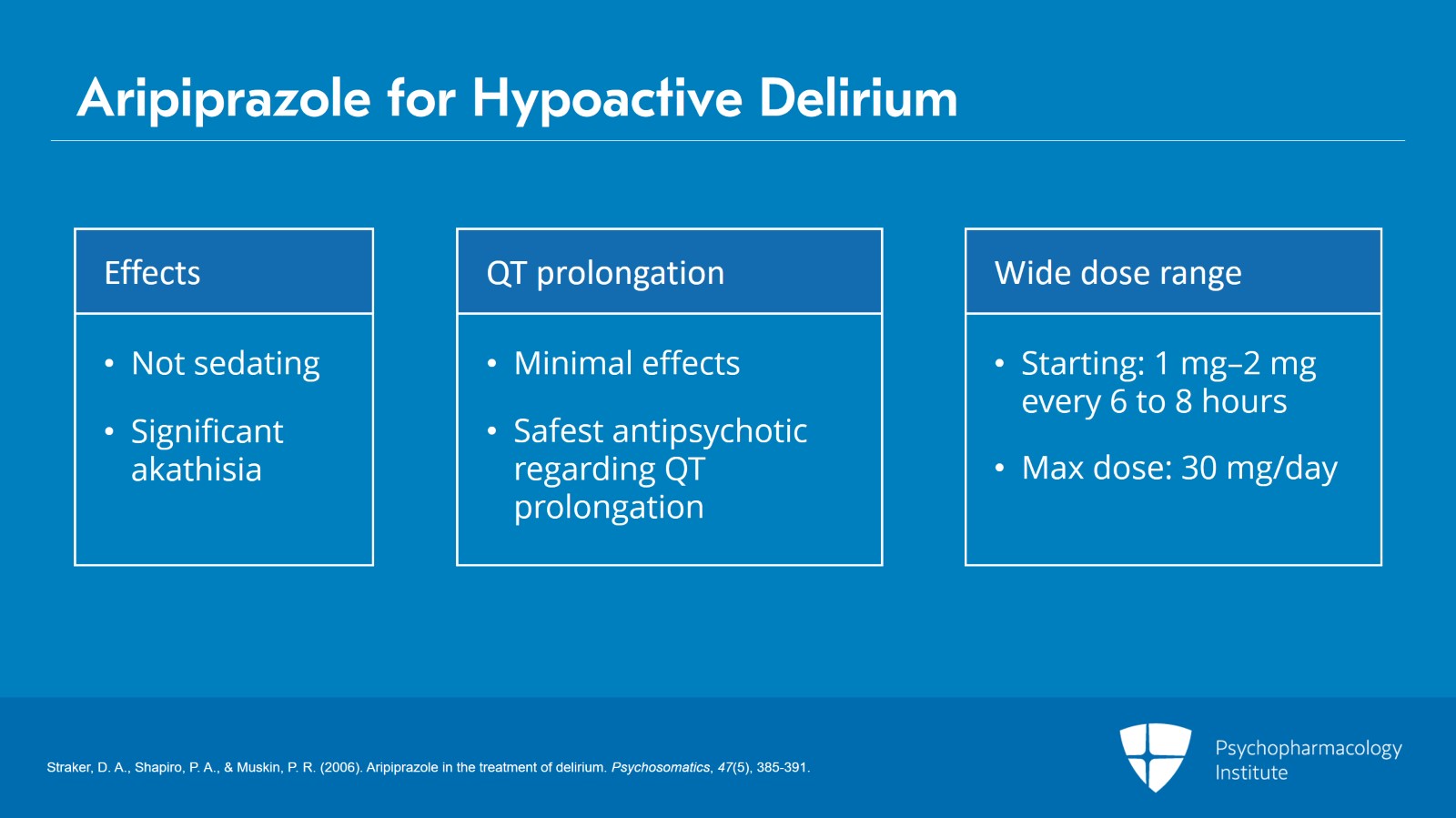
For patients with a hypoactive delirium who may have prominent perceptual disturbances, another agent that has grown in popularity is aripiprazole. Aripiprazole unlike many of the other agents we've talked about is not particularly sedating. So it does not tend to sedate patients or even really calm patients but it can be great for effects on perceptual disturbances. And though aripiprazole is mostly a low potency agent, it is important to remember that it can cause significant akathisia and that's something to monitor patients for if you're using it for delirium. It has minimal effects on QT and is probably the safest antipsychotic with regard to QT prolongation. It has a fairly wide dose range. Doses typically start at 1 to 2 mg every six to eight hours but doses up to 30 mg a day may be tolerated.
References:
- Straker, D. A., Shapiro, P. A., & Muskin, P. R. (2006). Aripiprazole in the treatment of delirium. Psychosomatics, 47(5), 385-391.
Slide 22 of 26
With regard to other second-generation agents, ziprasidone is used in some settings but concerns about QT prolongation remain prominent. And newer agents like lurasidone are occasionally used but really don't have a lot of evidence or even anecdotal experience at this point.
References:
- Leucht, S., Cipriani, A., Spineli, L., Mavridis, D., Örey, D., Richter, F., Samara, M., Barbui, C., Engel, R. R., Geddes, J. R., Kissling, W., Stapf, M. P., Lässig, B., Salanti, G., & Davis, J. M. (2014). Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. FOCUS, 12(2), 192-204.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 26
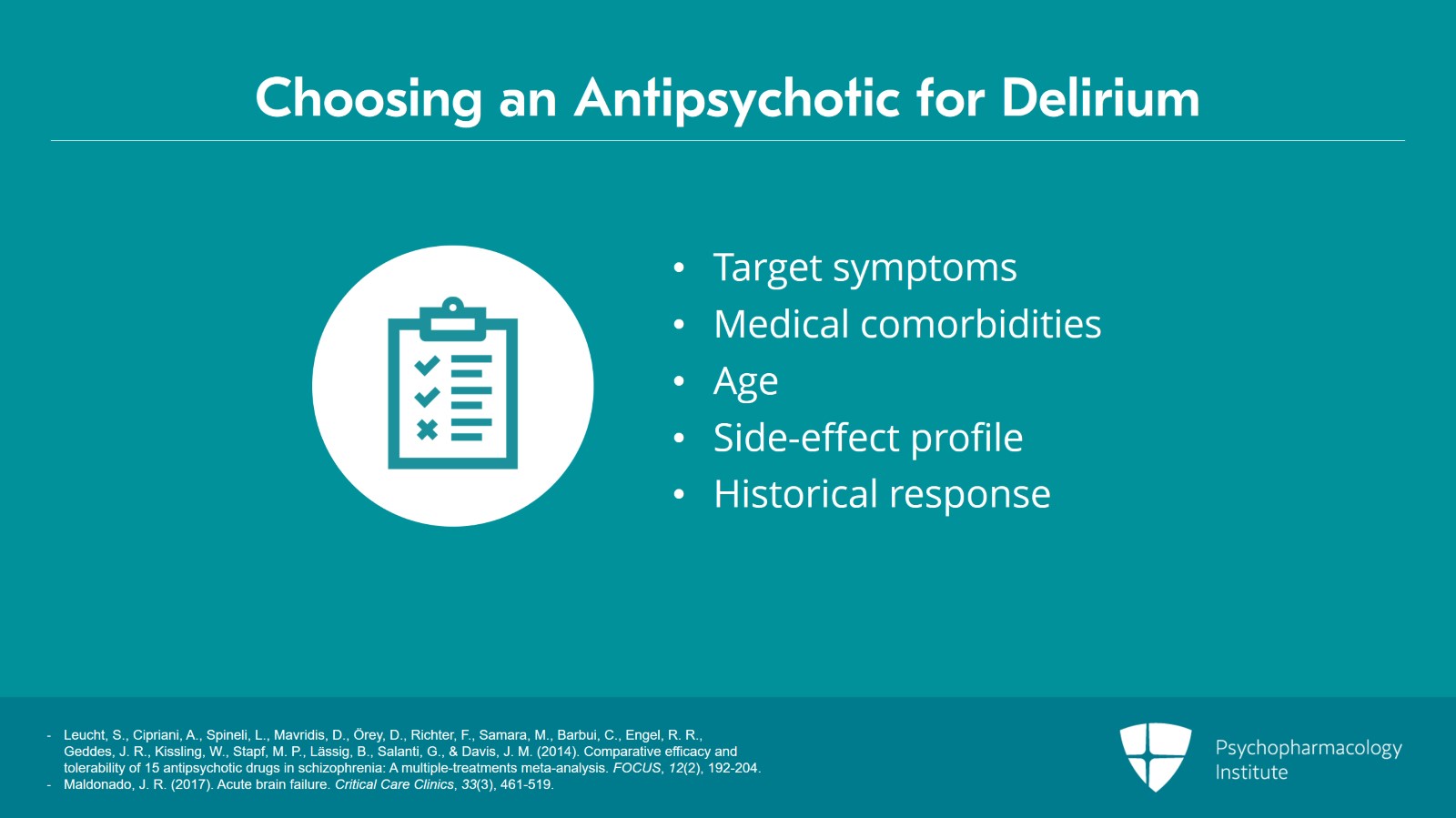
So overall, the choice of antipsychotic should be largely based on target symptoms, medical comorbidities, age, side effect profile and historical response.
References:
- Leucht, S., Cipriani, A., Spineli, L., Mavridis, D., Örey, D., Richter, F., Samara, M., Barbui, C., Engel, R. R., Geddes, J. R., Kissling, W., Stapf, M. P., Lässig, B., Salanti, G., & Davis, J. M. (2014). Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. FOCUS, 12(2), 192-204.
- Maldonado, J. R. (2017). Acute brain failure. Critical Care Clinics, 33(3), 461-519.
Slide 24 of 26
If you move towards a pharmacologic strategy to help mitigate agitation or perceptual disturbances, intravenous haloperidol may be a good option because it's fast acting and it avoids the pain, fear and elevation of creatinine kinase that is caused by repeated IM injections. Although atypical antipsychotics were originally used to help manage delirium primarily because they were felt to be safer in terms of side effects, these comparisons do not actually have robust supporting data.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 25 of 26
Quetiapine is preferred by neurologists because of lower rates of EPS but it's important to keep in mind that at low doses quetiapine is primarily exerting effects through anticholinergic and antihistaminergic actions. And finally, aripiprazole may be a particularly good strategy for patients with a hypoactive delirium who have prominent perceptual disturbances.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.