Slides and Transcript
Slide 1 of 16
So what are the guiding principles overall for treating bipolar disorder during pregnancy?
Slide 2 of 16
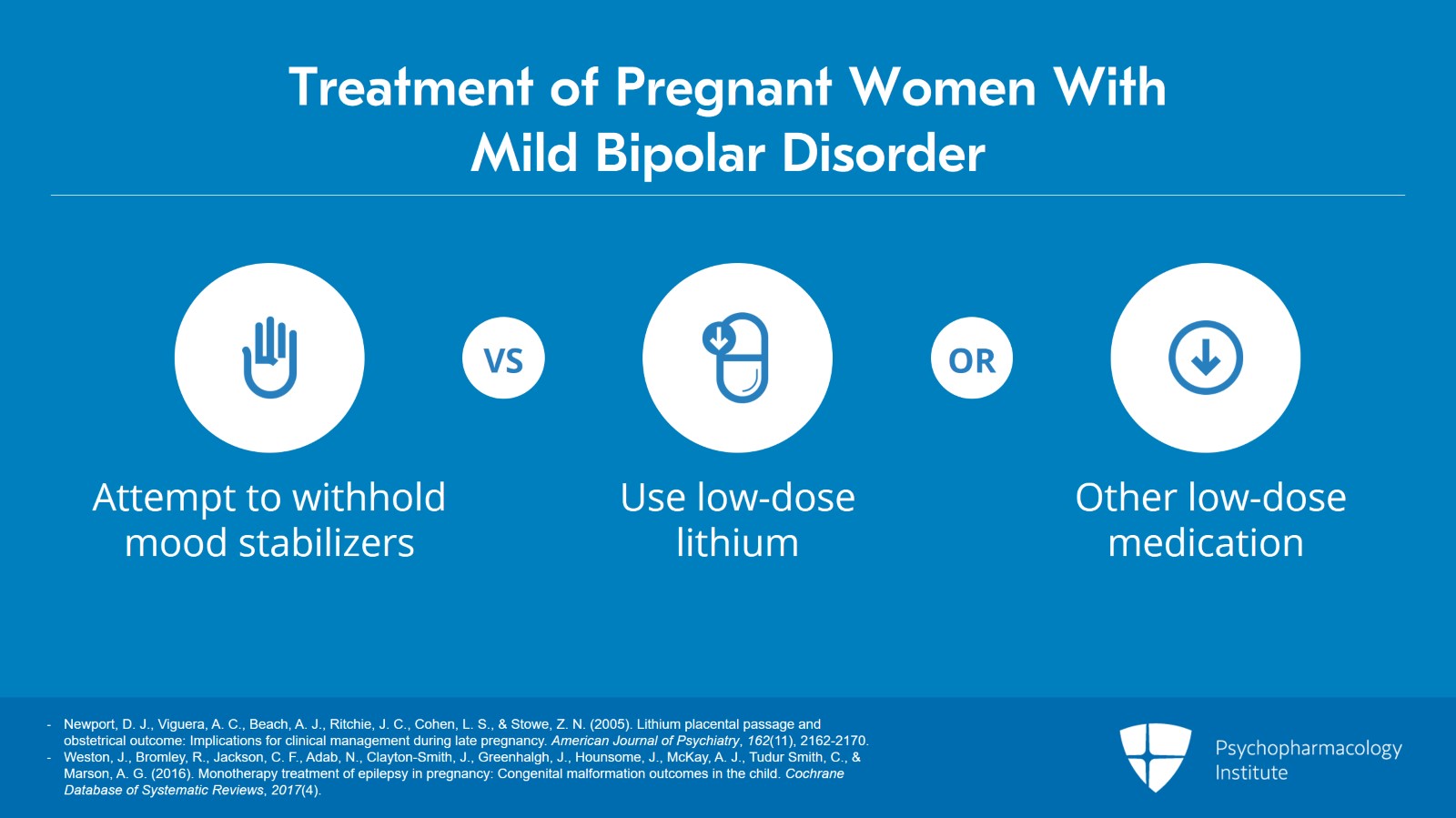
Well, if a patient has extremely mild illness and has been stable without medication for many years, you can gingerly attempt to withhold mood stabilizers during the first trimester versus using low-dose lithium or maybe other low-dose medications such as an atypical during the first trimester.
References:
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
- Weston, J., Bromley, R., Jackson, C. F., Adab, N., Clayton-Smith, J., Greenhalgh, J., Hounsome, J., McKay, A. J., Tudur Smith, C., & Marson, A. G. (2016). Monotherapy treatment of epilepsy in pregnancy: Congenital malformation outcomes in the child. Cochrane Database of Systematic Reviews, 2017(4).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 16
But please, if you do this, monitor very, very carefully for early relapse because even if this patient has been stable without medication for years, if she really has bipolar disorder, she is at risk for decompensation during pregnancy and certainly during the postpartum.
References:
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
- Weston, J., Bromley, R., Jackson, C. F., Adab, N., Clayton-Smith, J., Greenhalgh, J., Hounsome, J., McKay, A. J., Tudur Smith, C., & Marson, A. G. (2016). Monotherapy treatment of epilepsy in pregnancy: Congenital malformation outcomes in the child. Cochrane Database of Systematic Reviews, 2017(4).
Slide 4 of 16
For the patient with moderate-to-severe illness, we recommend continuing the mood stabilizers that work and any other psychiatric medications as needed to maintain stability throughout pregnancy.
References:
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
- Weston, J., Bromley, R., Jackson, C. F., Adab, N., Clayton-Smith, J., Greenhalgh, J., Hounsome, J., McKay, A. J., Tudur Smith, C., & Marson, A. G. (2016). Monotherapy treatment of epilepsy in pregnancy: Congenital malformation outcomes in the child. Cochrane Database of Systematic Reviews, 2017(4).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 16
What are reasonable treatment choices for bipolar illness in pregnancy? Well, lithium basically still is the gold standard but lamotrigine can be used as well for patients who have a predominantly depressive type of bipolar disorder.
References:
- Cunnington, M., & Tennis, P. (2005). Lamotrigine and the risk of malformations in pregnancy. Neurology, 64(6), 955-960.
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
- Weston, J., Bromley, R., Jackson, C. F., Adab, N., Clayton-Smith, J., Greenhalgh, J., Hounsome, J., McKay, A. J., Tudur Smith, C., & Marson, A. G. (2016). Monotherapy treatment of epilepsy in pregnancy: Congenital malformation outcomes in the child. Cochrane Database of Systematic Reviews, 2017(4).
Slide 6 of 16
These have well-characterized reproductive safety profiles and relatively low absolute risks especially as compared to decompensation risks with women who have bipolar disorder.
References:
- Cunnington, M., & Tennis, P. (2005). Lamotrigine and the risk of malformations in pregnancy. Neurology, 64(6), 955-960.
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 16
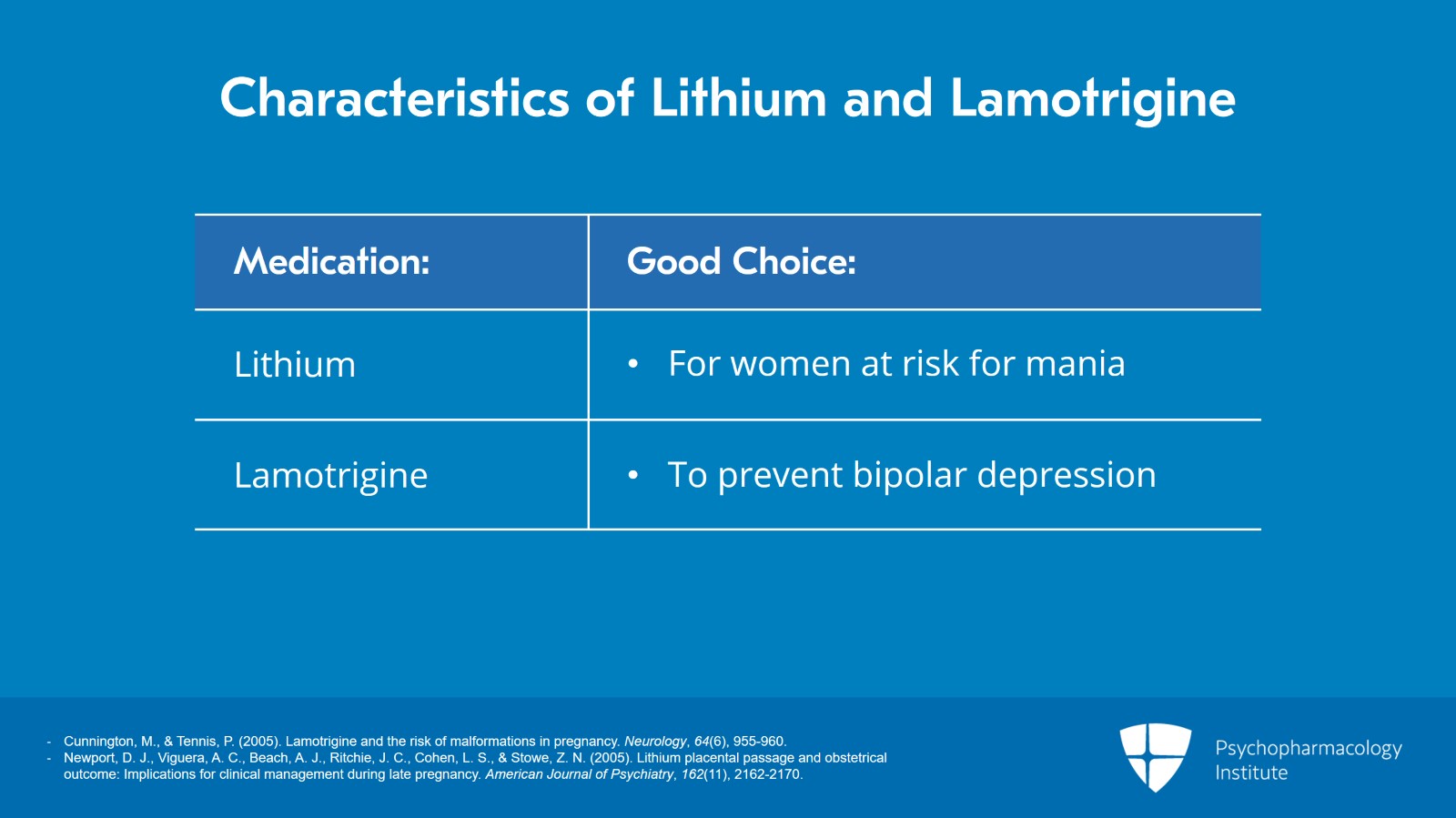
Lithium is a particularly good choice for women at risk for mania and lamotrigine is a good choice to prevent bipolar depression but not necessarily mania.
References:
- Cunnington, M., & Tennis, P. (2005). Lamotrigine and the risk of malformations in pregnancy. Neurology, 64(6), 955-960.
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Slide 8 of 16
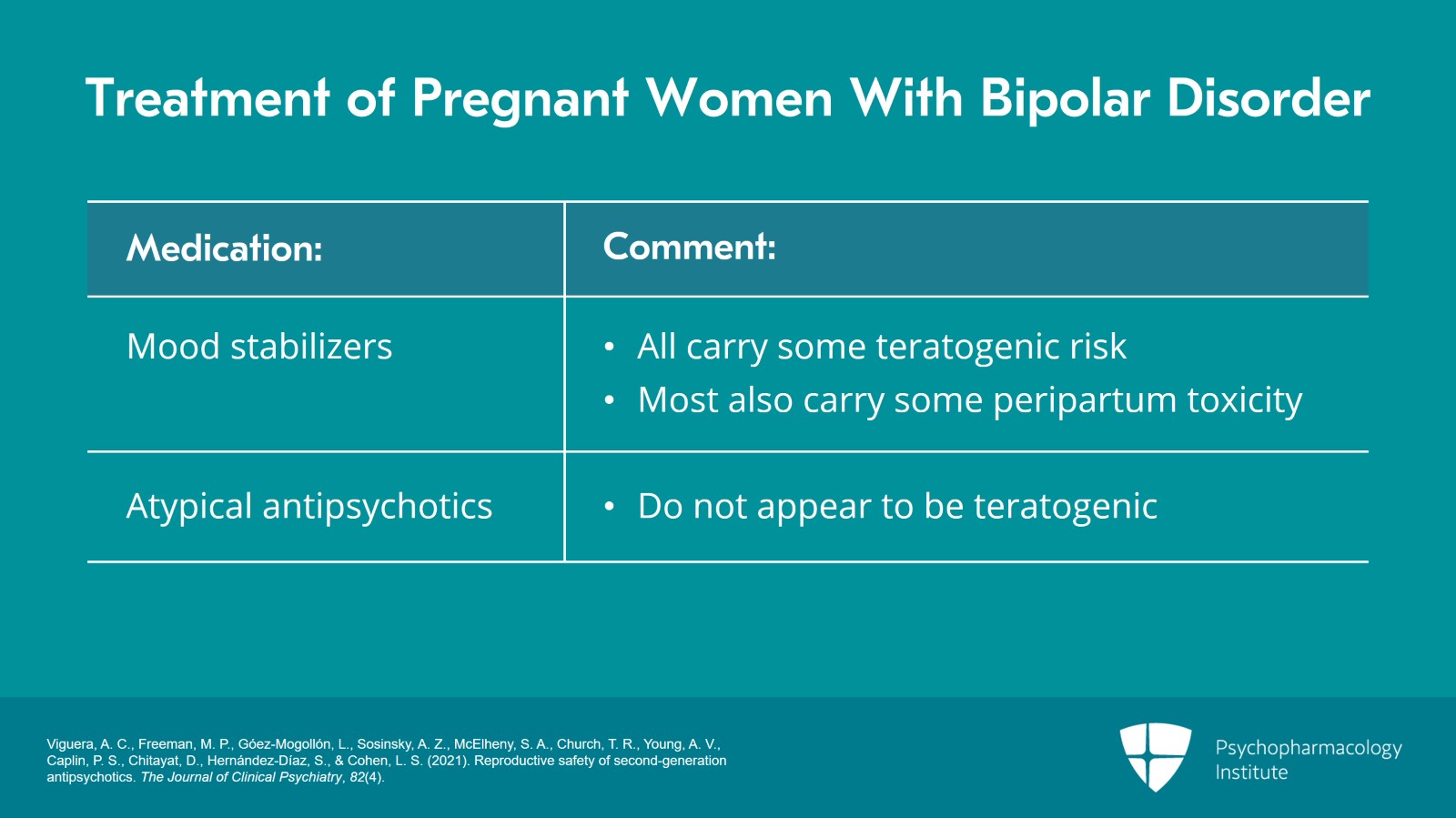
Atypical antipsychotics, well, the data is growing and they do not appear to be teratogenic.
References:
- Viguera, A. C., Freeman, M. P., Góez-Mogollón, L., Sosinsky, A. Z., McElheny, S. A., Church, T. R., Young, A. V., Caplin, P. S., Chitayat, D., Hernández-Díaz, S., & Cohen, L. S. (2021). Reproductive safety of second-generation antipsychotics. The Journal of Clinical Psychiatry, 82(4).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 16
So in summary, when treating the bipolar pregnant patient, all mood stabilizers carry some teratogenic risk and most of them also carry some peripartum toxicity. When it comes to atypical antipsychotics, they do not appear to be teratogenic.
References:
- Viguera, A. C., Freeman, M. P., Góez-Mogollón, L., Sosinsky, A. Z., McElheny, S. A., Church, T. R., Young, A. V., Caplin, P. S., Chitayat, D., Hernández-Díaz, S., & Cohen, L. S. (2021). Reproductive safety of second-generation antipsychotics. The Journal of Clinical Psychiatry, 82(4).
Slide 10 of 16
And of course, treatment choice is made case by case. Use the safest regimen to maintain and maximize maternal mood stability and fetal safety.
References:
- Viguera, A. C., Freeman, M. P., Góez-Mogollón, L., Sosinsky, A. Z., McElheny, S. A., Church, T. R., Young, A. V., Caplin, P. S., Chitayat, D., Hernández-Díaz, S., & Cohen, L. S. (2021). Reproductive safety of second-generation antipsychotics. The Journal of Clinical Psychiatry, 82(4).
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 16
We have to remember there are no simple decisions for psychiatrically ill pregnant women with bipolar disorder. Good outcomes depend on the physical and emotional health of the pregnant mother.
References:
- Newport, D. J., Viguera, A. C., Beach, A. J., Ritchie, J. C., Cohen, L. S., & Stowe, Z. N. (2005). Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. American Journal of Psychiatry, 162(11), 2162-2170.
Slide 12 of 16
I would also recommend that you consider an article for your patients that I published with a co-writer, a co-researcher, Dr. Sonya Rasminsky, in the Washington Post and the article is in the On Parenting section, The "good enough" mother begins in pregnancy. And basically, it talks about how one has to accept inherent uncertainty and ask what can I live with given the conditions that I have now as opposed to assuring a perfect outcome because after all every baby deserves a healthy mother and parent and every mother deserves to ensure parenthood.
References:
- Burt, V. K., & Rasminsky, S. (2017, January 4). The “good enough” mother begins in pregnancy. Washington Post.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 16
The key points here are pregnant women with moderate to severe bipolar illness should continue the mood stabilizers and other psychiatric medications that have kept them stable. Lithium and lamotrigine are reasonable treatment choices for bipolar illness in pregnancy.
Slide 14 of 16
Lithium is still a first choice for bipolar pregnant women because it works well for both depression and mania. Lamotrigine may be considered as well for pregnant bipolar women although it's thought to be better at preventing depression than mania.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 16
The database for atypical antipsychotics in pregnancy is growing and suggests that these agents do not appear to be teratogenic. And finally, treatment of bipolar disorder in pregnancy is decided best on a case-by-case basis and is made after considering the data and the clinical profile of each patient.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.