Slides and Transcript
Slide 2 of 22
Now, I will say that insight-oriented therapies, don’t seem to help the core obsessive and compulsive symptoms.
To date, the effective treatments include individual or family-based cognitive behavioral therapy which includes exposure and response prevention therapy and the potent serotonin reuptake inhibitors.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 22
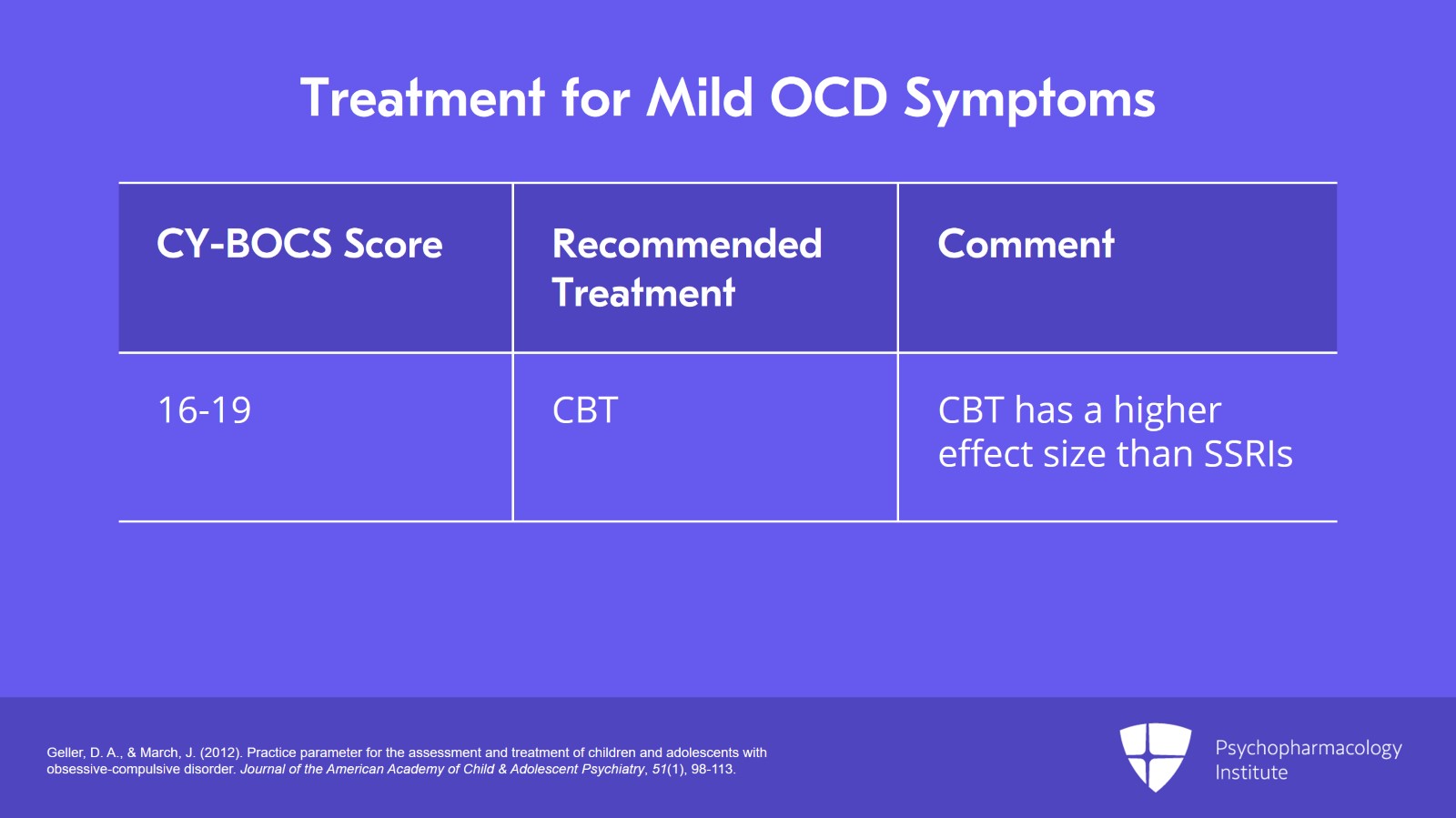
There seems to be a general consensus in the field that mild obsessive-compulsive symptoms, which are characterized by a Children’s Yale-Brown Obsessive-Compulsive Scale score of 16 to 19, the recommended treatment here is CBT alone.
And the data to date suggest that CBT has a higher effect size than the selective serotonin reuptake inhibitor.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 4 of 22
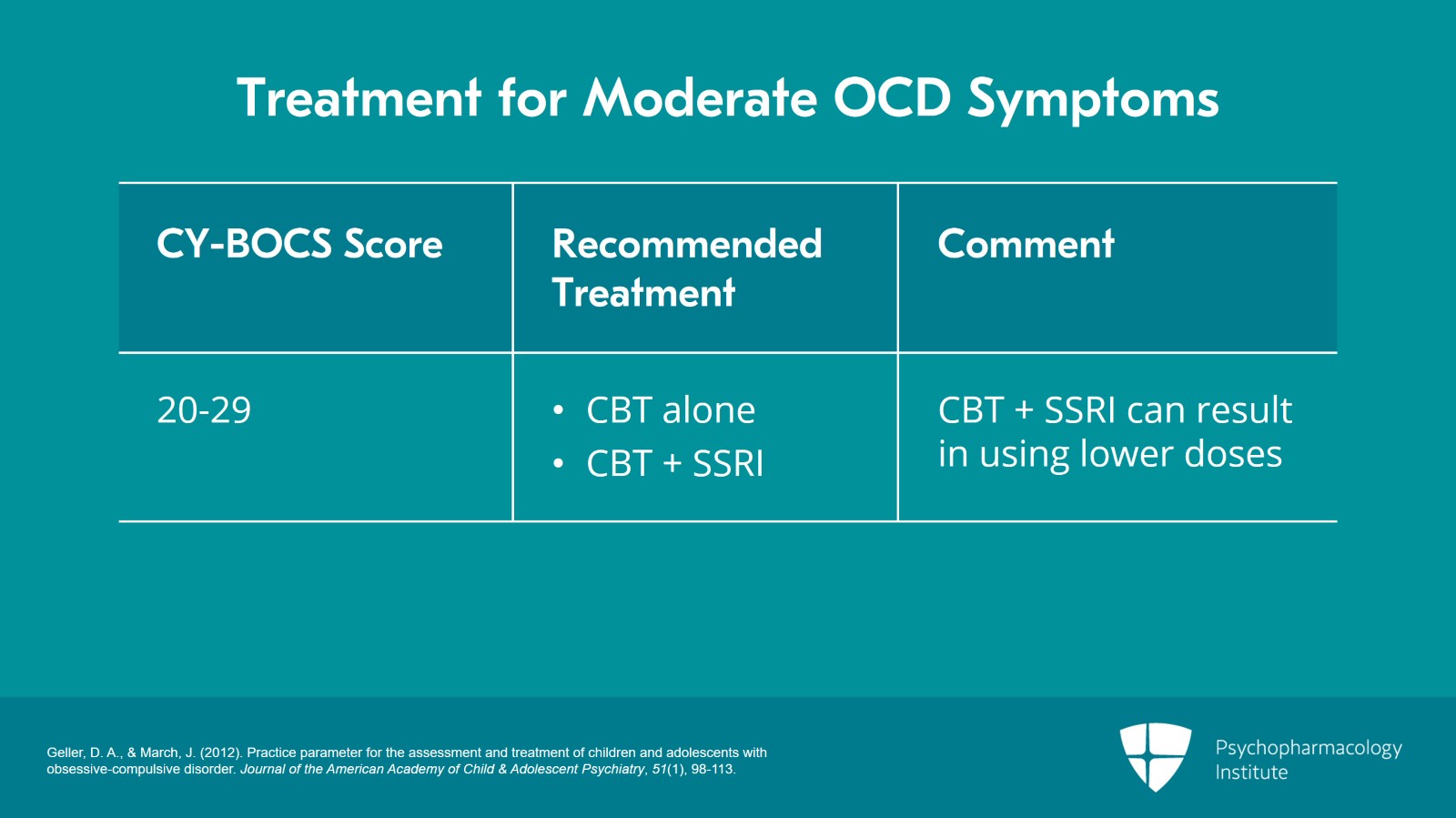
For moderate OCD symptoms with a CY-BOCS score of 20 to 29, we recommend starting with either CBT alone or CBT plus SSRI.
Now, obviously, there are some families who will not consider medicine under any circumstance.
There are some who want to try cognitive behavioral therapy first before they go to medicine, and some who think the symptoms are significantly disabling that they’re willing to try both cognitive behavioral therapy and selective serotonin reuptake inhibitor treatment initially.
I would also emphasize that there’s good data to show that if you use cognitive behavioral therapy with medication you can end up using lower doses of medication oftentimes and that may result in fewer side effects.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
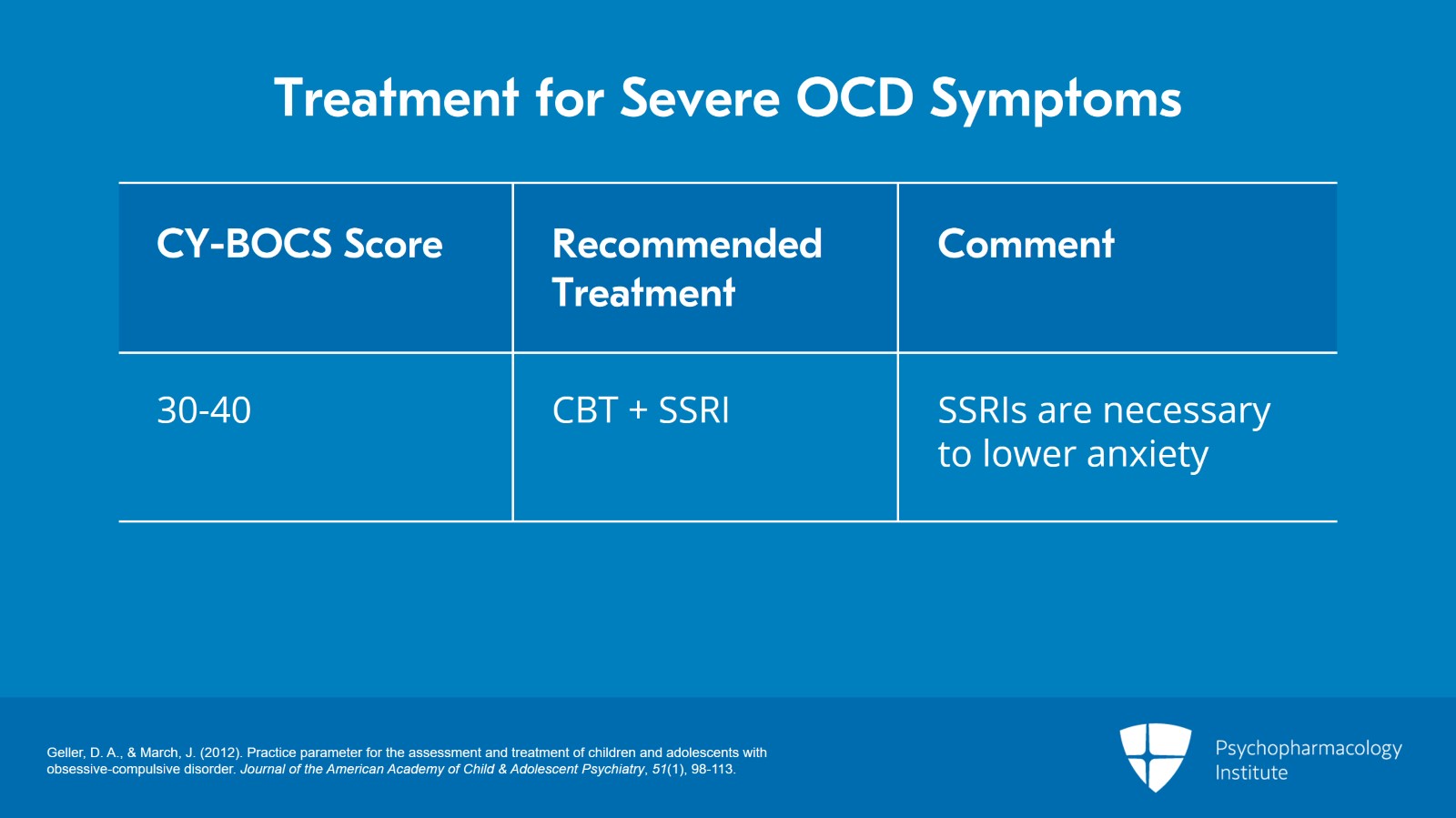
Slide 5 of 22
For severe OCD symptoms, that’s a CY-BOCS score of 30 to 40 we recommend starting with CBT plus SSRI. Typically, those symptoms are so severe that cognitive behavioral therapy alone is not sufficient to take down the anxiety to levels where it can work. And so, you need a medication intervention to at least bring the anxiety to a level where the cognitive behavioral therapy strategies can work.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 6 of 22
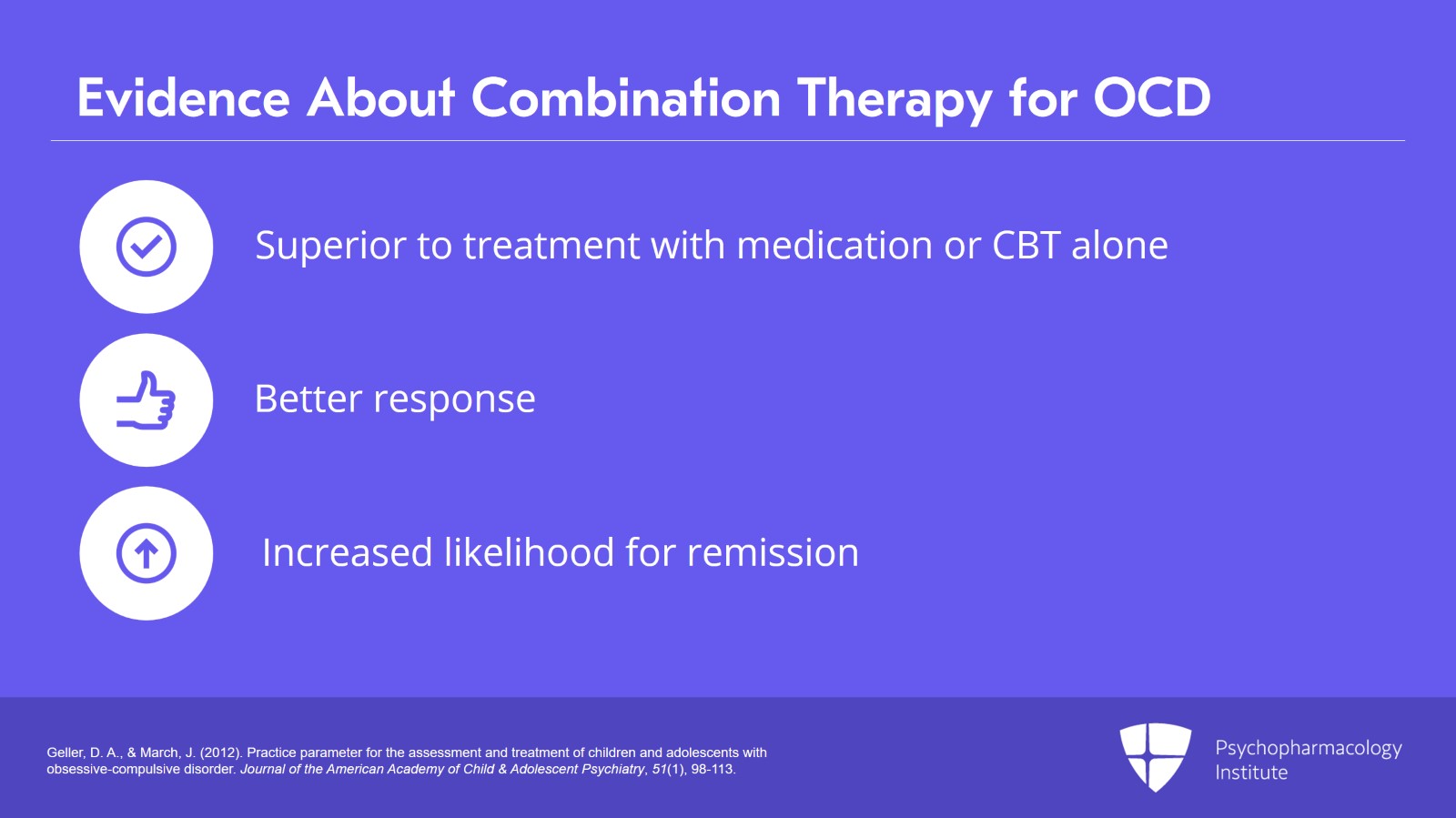
Now, in some of the trials, the data are pretty good that combination therapy, that is cognitive behavioral therapy plus a selective serotonin reuptake inhibitor was superior to treatment with medication alone, to treatment with cognitive behavioral therapy alone, and superior to placebo.
So, there was a bigger and better response and that there was an increased likelihood for remission with using both cognitive behavioral therapy and selective serotonin reuptake inhibitor.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 22
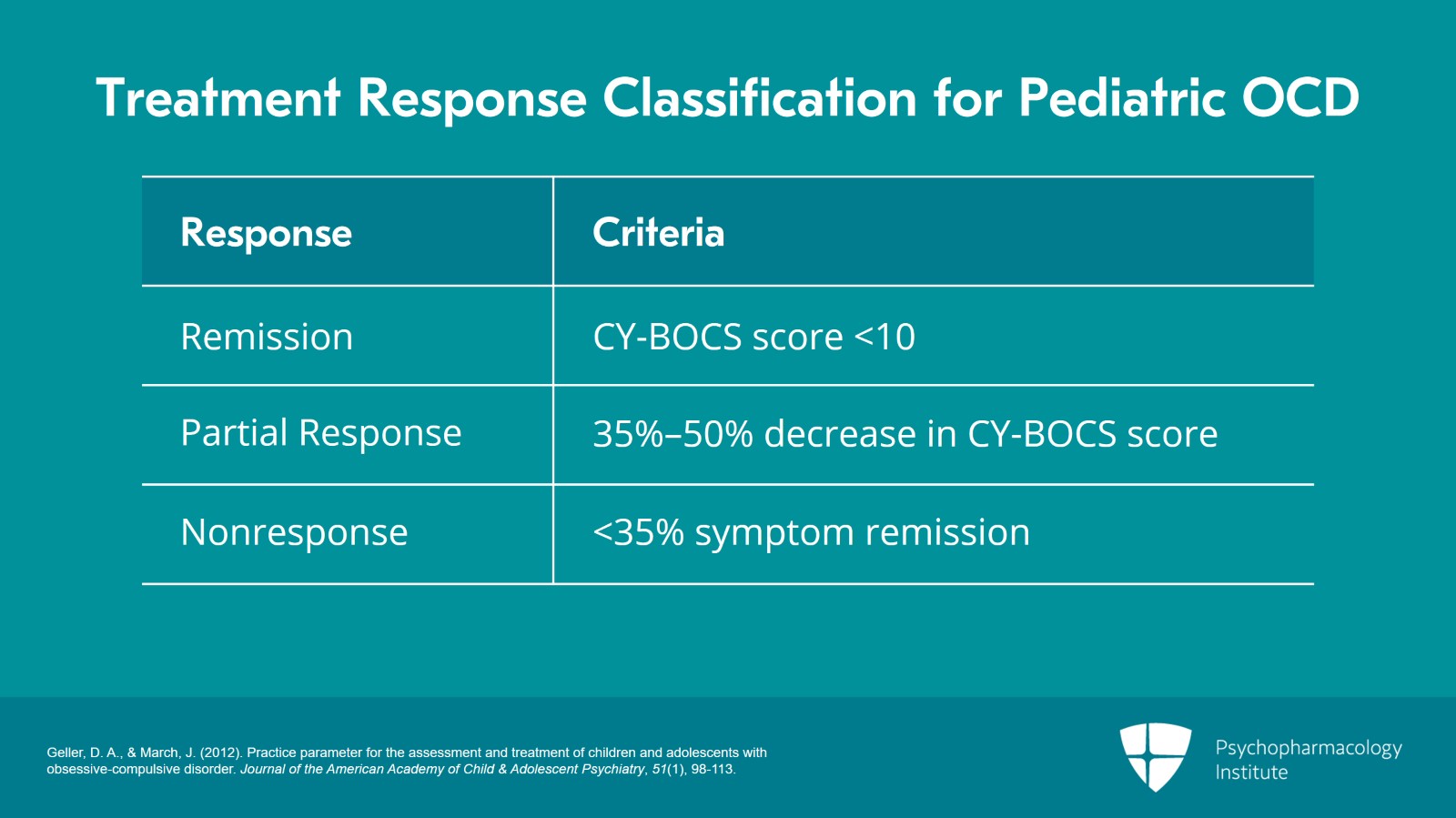
Remission is characterized by a CY-BOCS score of less than 10, that’s not often obtained in obsessive-compulsive disorder treatment. Particularly in children and adolescents, often there is a response but there can be continued functional impairment.
Partial response, here, we’re talking a 35% to 50% decrease in CY-BOCS score after a minimum of 10 weeks of an optimal tolerated dose.
For nonresponse, that’s a less than 35% symptom remission.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 8 of 22
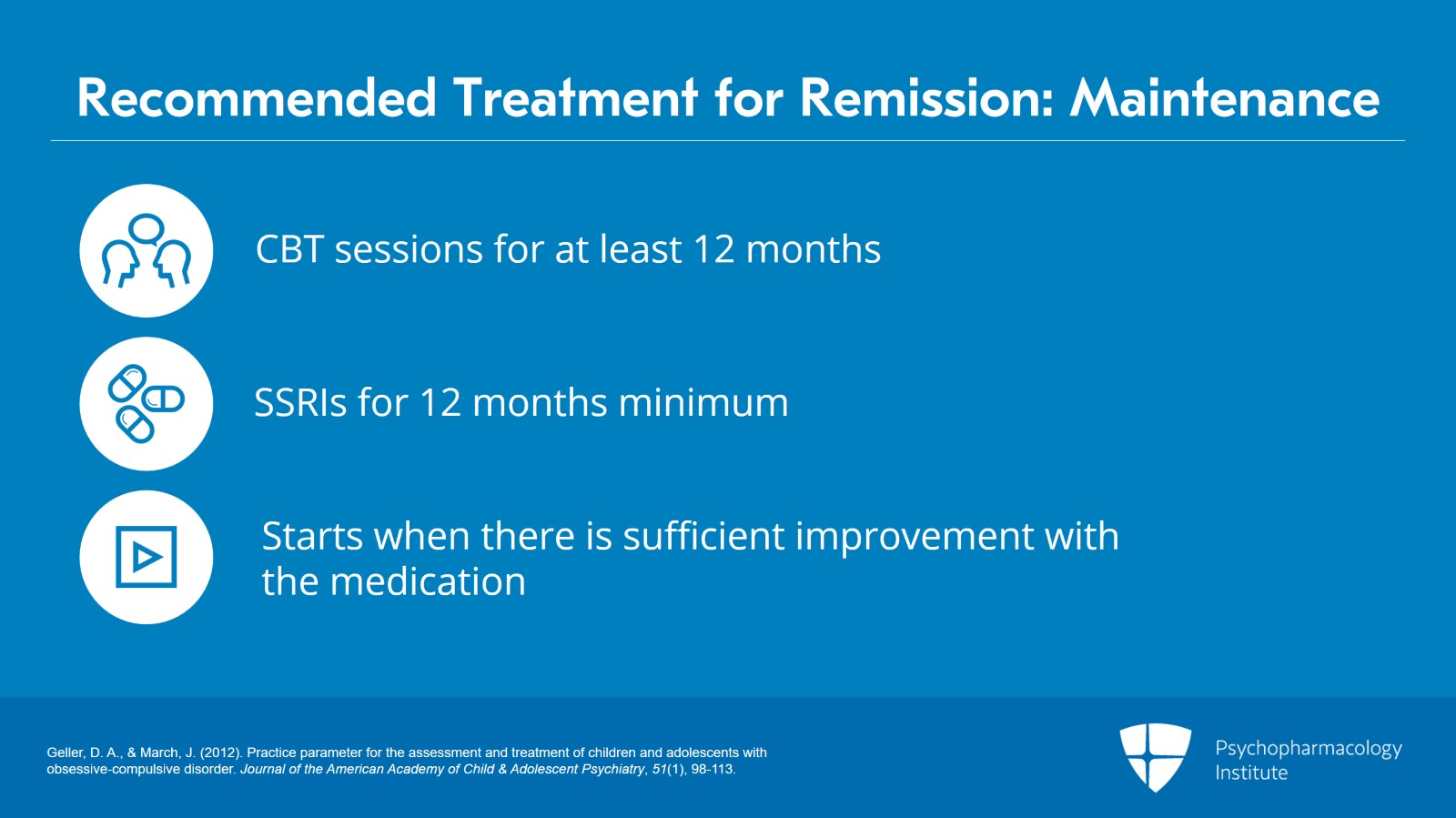
In terms of remission, what we recommend here is a maintenance cognitive behavioral therapy, our program will give booster sessions for at least 12 months as needed, maintenance of SSRI at an optimal dose for 12 months minimum.
So what we recommend in our clinic is, in terms of medication, once there is a medication with sufficient improvement at that dose that’s when the clock starts for one year.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 22
Partial response, in this case, you can switch to another SSRI. That’s a perfectly reasonable recommendation.
That being said, some people are somewhat hesitant to do this because they feel like, “Well, if I switch to another SSRI, will I lose the 35% to 50% symptom reduction?” And so one thing that can be done if it hasn’t been done previously is augment with cognitive behavioral therapy, and another is to augment with the serotonin reuptake inhibitor which is also a norepinephrine reuptake inhibitor, clomipramine. Augmentation with clomipramine can significantly increase treatment response and there are studies that have shown this.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 10 of 22
For nonresponse, your options are to switch to another SSRI, augment with cognitive behavioral therapy if not previously administered, augment with clomipramine, or augmenting with an atypical antipsychotic such as risperidone, quetiapine, aripiprazole, and treating the comorbid disorders concurrently.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 22
Medication dosing guidelines for pediatric OCD.
The mantra as any child and adolescent psychiatrist and most pediatricians know is start low, go slow.
I’ve seen more medication approaches, more medicines that are perfectly reasonable ruined by increasing the dose too rapidly. But all you’re typically doing when you do that is increasing the risk for side effects and taking away from the child’s ability to become tolerant and adjust to the medicine.
So I like to let medication work for at least two to three weeks before adjusting the dose upward because we know that even at the lower doses the longer they’re in the system, at least for many patients, you can see more effectiveness.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 12 of 22
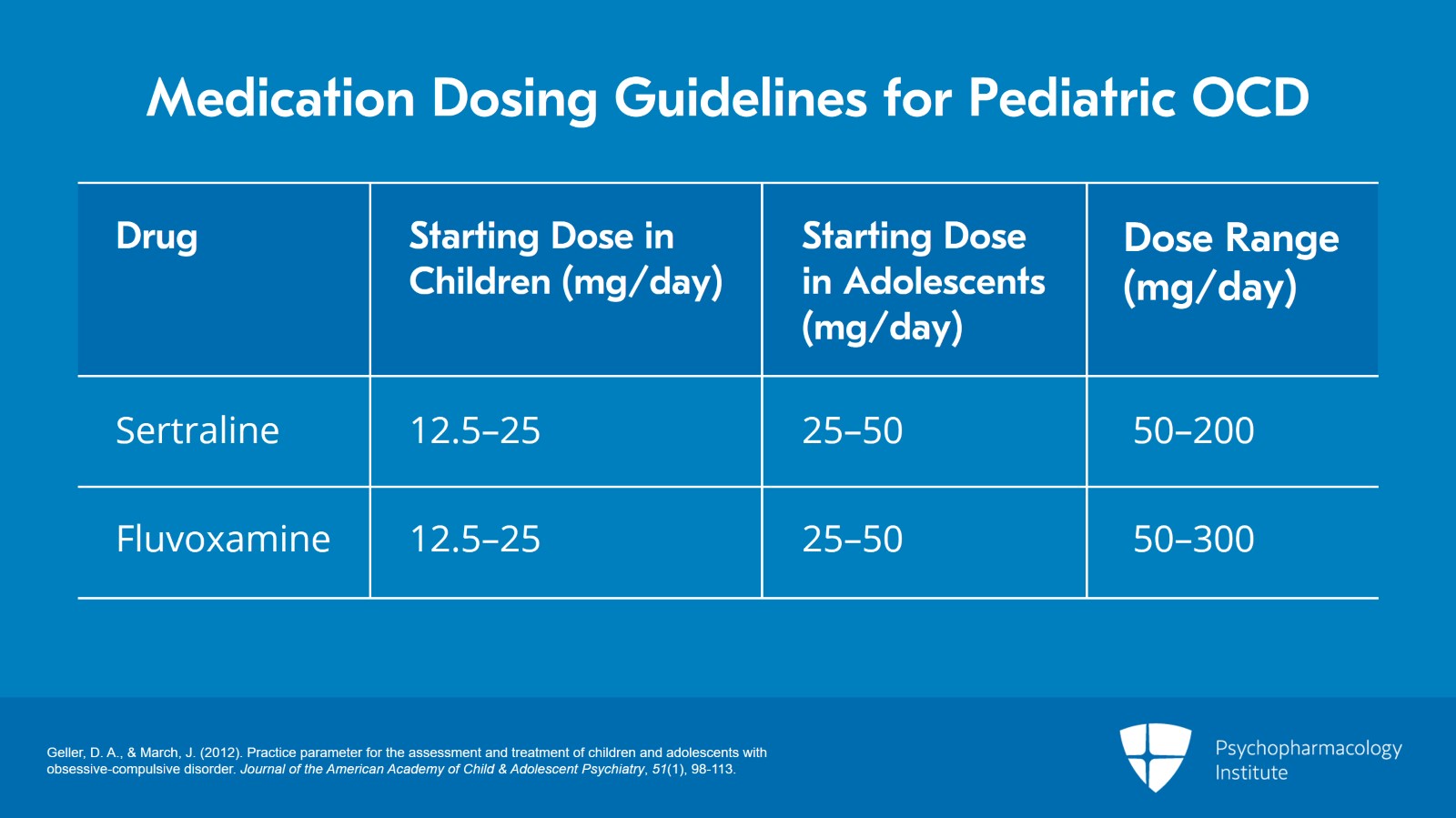
So, for sertraline, starting dose in a child is 12.5 mg to 25 mg per day, in an adolescent 25 mg to 50 mg per day. I typically like to start at 25 mg, again starting low. And the typical dose range is anywhere from 50 mg to 200 mg per day.
For fluvoxamine, the starting dose in a child is 12.5 mg to 25 mg per day and in an adolescent it’s 25 mg to 50 mg. Now, I’m more conservative so I like to start out at 25 mg in an adolescent and titrate the medicine gradually. Why do I do that? Because I have a number of patients where that’s enough, where I’ve not had to go up higher.
On the other hand, the dose range for fluvoxamine is 50 mg to 300 mg and I wouldn’t stop increasing the dose gradually until I got to the upper limits because there may be an effective treatment response.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 22
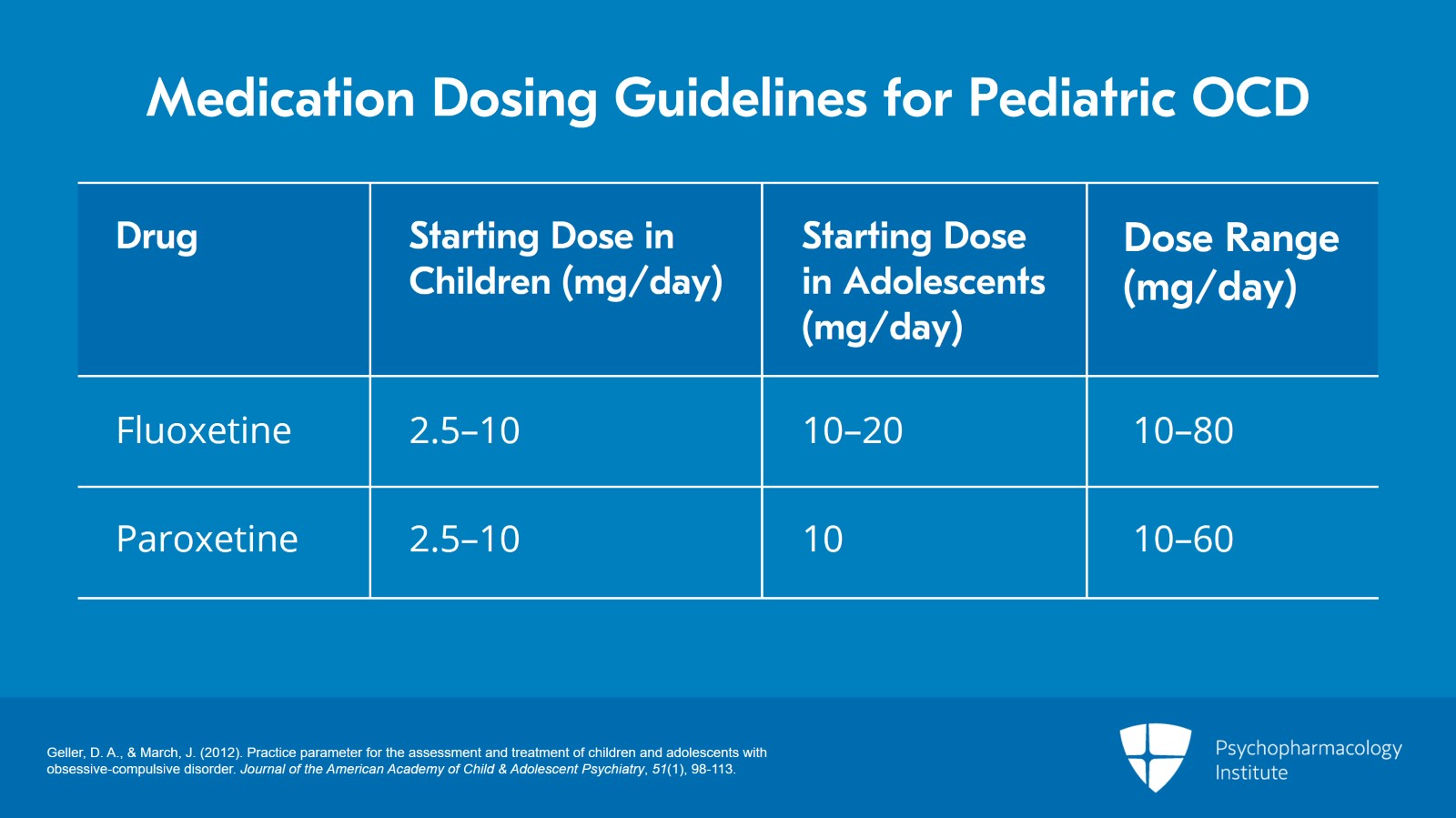
For fluoxetine, the starting dose in a child is 2.5 mg to 10 mg per day. In an adolescent, that starting dose is 10 mg to 20 mg. And again, I never start higher than 10 mg per day. I like to give children and adolescents as long as possible to get used to the medicine. I find that if they’re more tolerant to the medicine if we go slower that just as much is accomplished in terms of effectiveness but far fewer side effects are observed.
In terms of paroxetine, the starting dose is 2.5 mg to 10 mg in a child, 10 mg in adolescent, and the dose range is anywhere from 10 mg to 60 mg.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 14 of 22
For citalopram, the starting dose in a child is 2.5 mg to 10 mg per day. In an adolescent, the starting dose is 10 mg to 20 mg per day, and the dose range is 10 mg to 60 mg per day.
For escitalopram, the starting dose is 2.5 mg to 10 mg per day and for an adolescent the starting dose is 10 mg per day. Escitalopram has a dose range that’s very limited between 10 mg and 20 mg and it and citalopram are a nice choice of medicine if the child is on a lot of other medications because escitalopram and citalopram have the fewest drug-drug interactions.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 22
And finally, clomipramine which remember is a non-selective serotonin reuptake inhibitor, so it impacts both serotonin and norepinephrine, the starting dose is 6.25 mg to 25 mg in a child and 25 mg in an adolescent with a range anywhere from 25 mg to 200 mg per day.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Slide 16 of 22
One other key point is that obsessive-compulsive disorder in children and adolescents is actually next to ADHD, the area where there are more FDA-approved medicines.
So there are four FDA-approved medicines for pediatric OCD and they include sertraline , fluoxetine, fluvoxamine, and the non-selective serotonin reuptake inhibitor clomipramine.
Now, I bring that up because there are other medications, other selective serotonin reuptake inhibitors that work perfectly well in pediatric obsessive-compulsive disorder, but are not FDA approved.
While they work, I like to go with the FDA-approved medicines first. One, they have far more studies. Two, from a medical-legal standpoint, you’re using an FDA-approved medication. And three, the companies have not done all of the due diligence in terms of getting the FDA approval.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 22
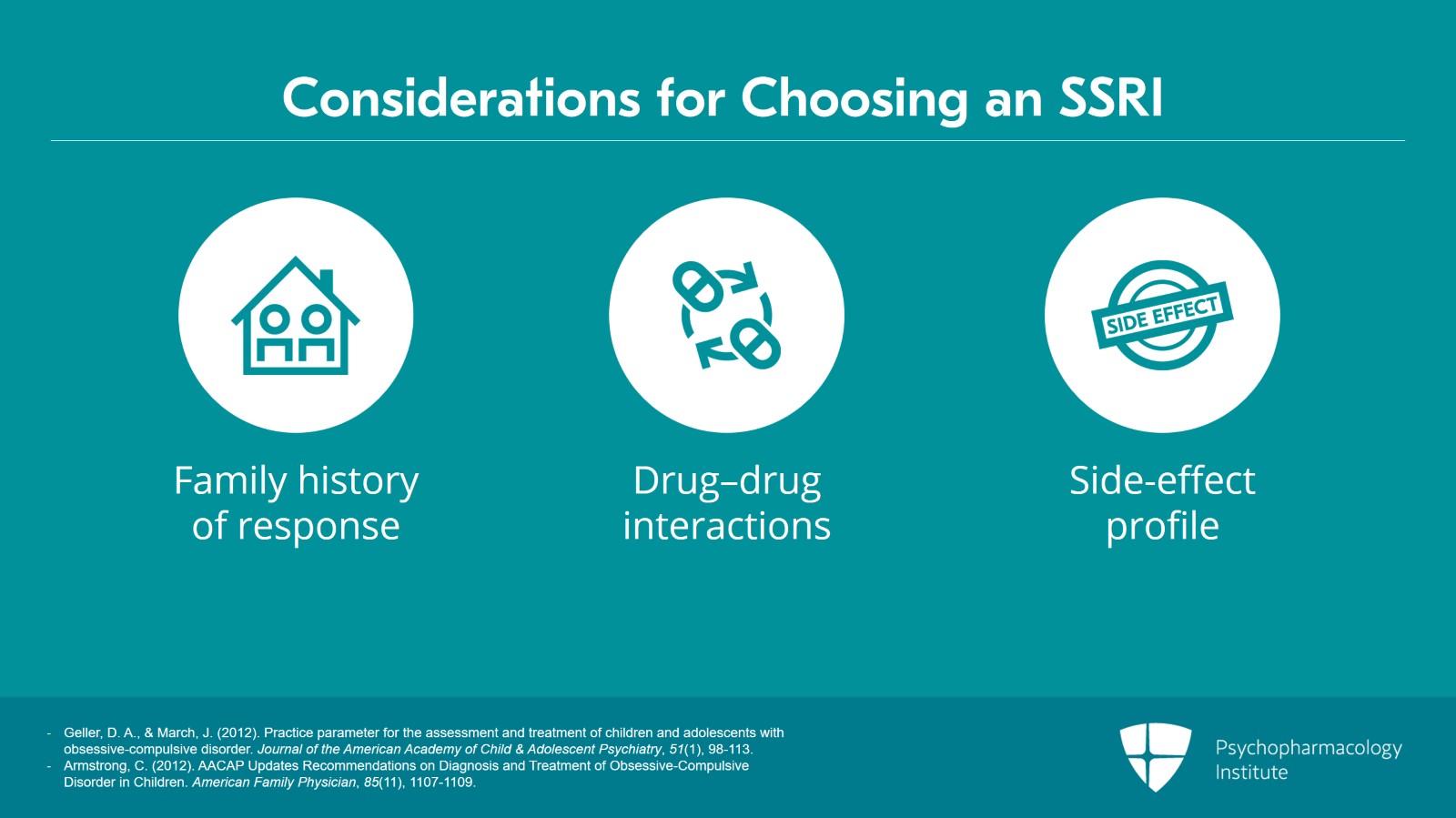
The decision regarding which SSRI to use should be made in coordination with the family based on family history of positive response, potential drug–drug interactions with other medications, and the side–effect profile.
Let’s say there’s a child whose mother has a panic disorder and responded amazingly well to paroxetine and had a horrible side effect or nonresponse to fluoxetine which is FDA approved. In that particular situation, I may want to go with the medicine where a first-degree relative had a good response.
If a child is on a lot of other medicines, then I might be inclined to consider a medicine with fewer drug-drug interactions such as escitalopram or citalopram.
References:
- Geller, D. A., & March, J. (2012). Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113.
- Armstrong, C. (2012). AACAP Updates Recommendations on Diagnosis and Treatment of Obsessive-Compulsive Disorder in Children. American Family Physician, 85(11), 1107-1109.
Slide 18 of 22
At present, there are no head-to-head studies that have been conducted to evaluate the efficacy of different SSRIs for treating pediatric OCD.
That being said, systematic review and meta-analyses have found slightly larger and less heterogeneous effect sizes in OCD patients treated with fluoxetine and sertraline compared to fluvoxamine suggesting potential superiority of these treatments over fluvoxamine.
All three SSRIs though have very good tolerability and are clearly superior to placebo.
References:
- Kotapati, V. P., Khan, A. M., Dar, S., Begum, G., Bachu, R., Adnan, M., Zubair, A., & Ahmed, R. A. (2019). The effectiveness of selective serotonin reuptake inhibitors for treatment of obsessive-compulsive disorder in adolescents and children: A systematic review and meta-analysis. Frontiers in Psychiatry, 10.
- Skapinakis, P., Caldwell, D., Hollingworth, W., Bryden, P., Fineberg, N., Salkovskis, P., Welton, N., Baxter, H., Kessler, D., Churchill, R., & Lewis, G. (2016). A systematic review of the clinical effectiveness and cost-effectiveness of pharmacological and psychological interventions for the management of obsessive–compulsive disorder in children/adolescents and adults. Health Technology Assessment, 20(43), 1-392.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 22
Treatment guidelines for pediatric OCD recommend cognitive behavioral therapy as the initial treatment of choice for children with mild to moderate OCD, and CBT alone or used in combination with SSRIs for children with moderate OCD, and CBT plus SSRI for children with severe cases of OCD.
Slide 20 of 22
There are four FDA-approved medicines for pediatric OCD and they include sertraline, fluoxetine, fluvoxamine, and the non-selective serotonin reuptake inhibitor clomipramine
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 22
For those who are partial or nonresponders to treatment, additional recommendations include a progression of additional treatment steps such as switching to another SSRI and/or augmenting with CBT if not previously administering, augmenting with clomipramine, and then augmenting with an atypical antipsychotic.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.